Case of the week
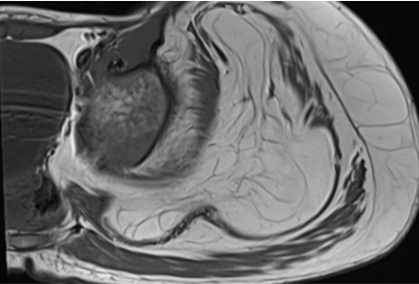
31 yr old female with history of right shoulder and upper arm pain, difficulty in lifting the arm.
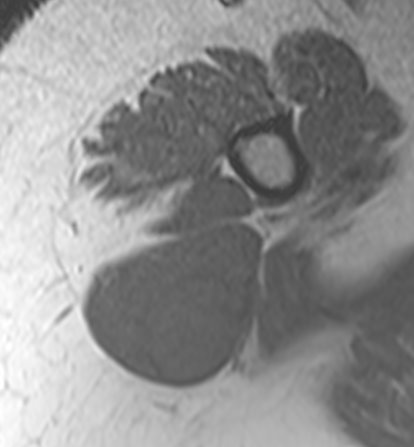
View Case2 years old male presented with progressive disproportionate enlargement of left thigh, leg, foot and hand.
2 years old male presented with progressive disproportionate enlargement of left thigh, leg, foot and hand.
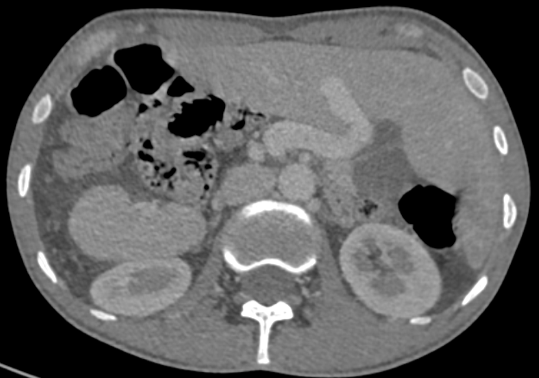
View CaseA 54 years old, male patient presented with complaints of swelling in the bilateral lower limbs and breathlessness.
A 54 years old, male patient presented with complaints of swelling in the bilateral lower limbs and breathlessness.
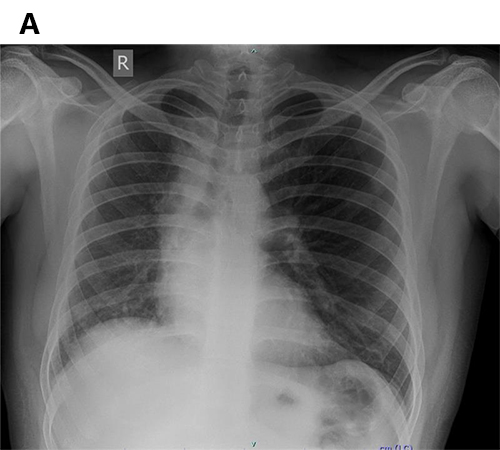
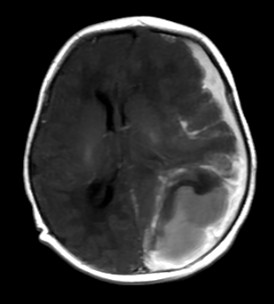
View Case37 year old male presented with sudden loss of consciousness following nocturnal micturition with abnormal screening chest X- ray.
37 year old male presented with sudden loss of consciousness following nocturnal micturition with abnormal screening chest X- ray.
View CaseA 27 year old gentleman presented with few episodes of hemoptysis. He also had a history of cough with expectoration since few months.
A 27 year old gentleman presented with few episodes of hemoptysis. He also had a history of cough with expectoration since few months.
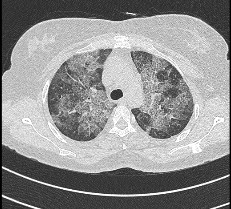
View CaseWalk in OPD patient with History of on and off mild breathlessness and fever since 6 months.
Walk in OPD patient with History of on and off mild breathlessness and fever since 6 months. No history of tuberculosis or ICU admission.
View Case5 days old infant presented with history of seizure. History of prolonged difficult delivery present.
5 days old infant presented with history of seizure. History of prolonged difficult delivery present.
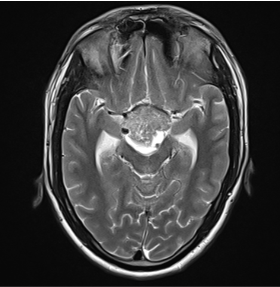
View CaseA 18 year old male, History of headache since 1 month. Change of voice since 1 month.
A 18 year old male, History of headache since 1 month.Change of voice since 1 month.
View Case