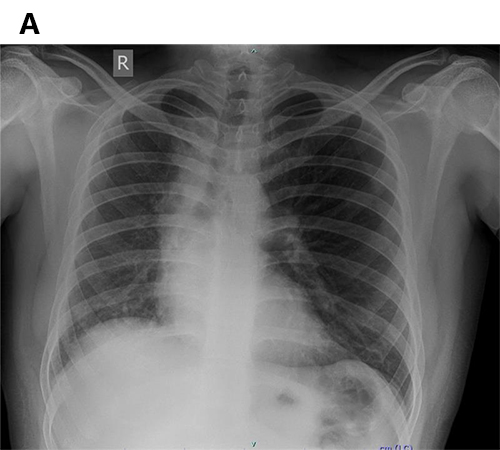
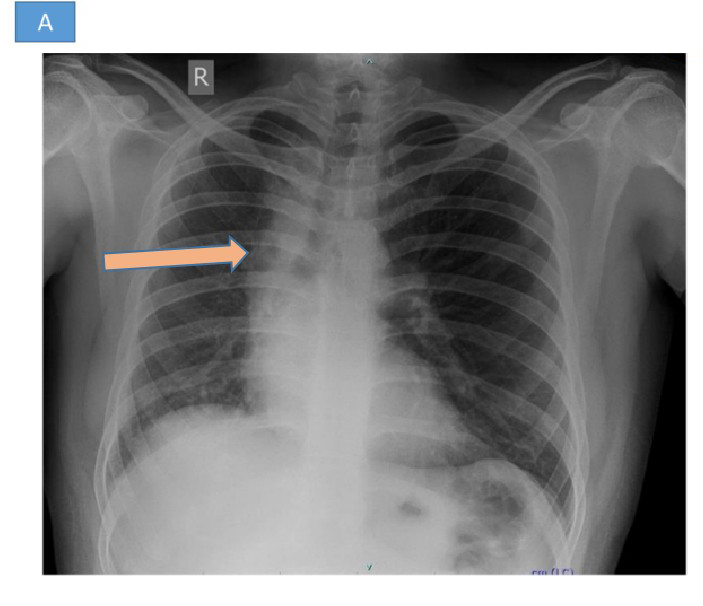
37 year old male presented with sudden loss of consciousness following nocturnal micturition with abnormal screening chest X- ray.
A.widening of paratracheal stripe. Hyperinflation of left lung. Volume loss of right lung.
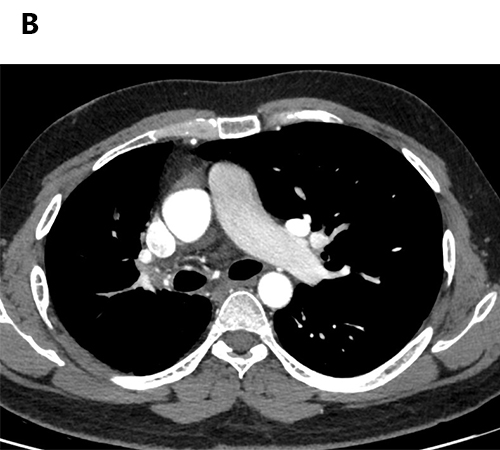
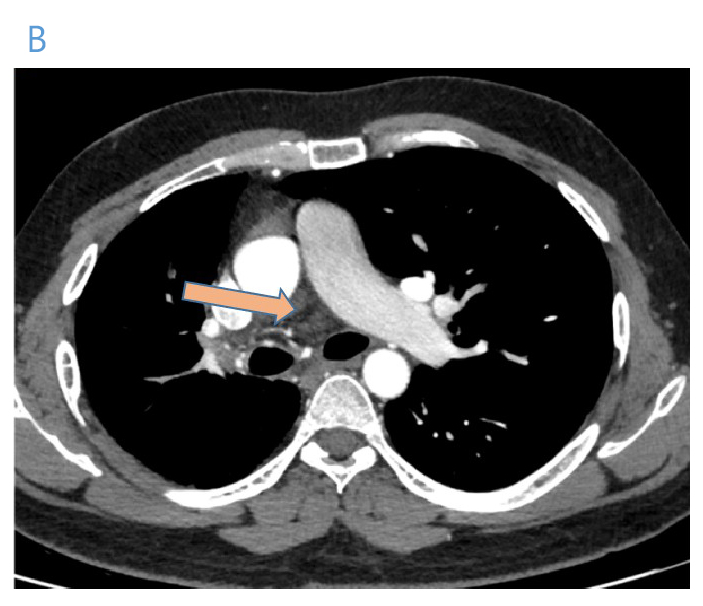
B.Absent right pulmonary artery
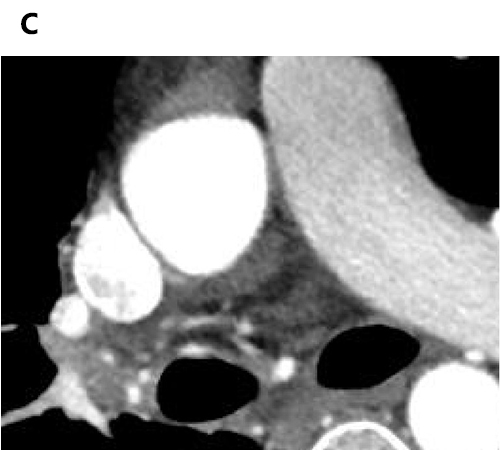
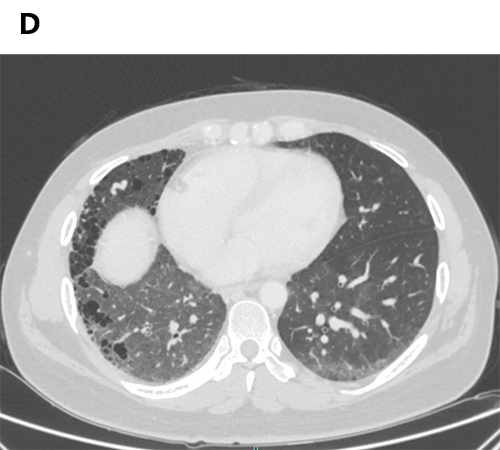
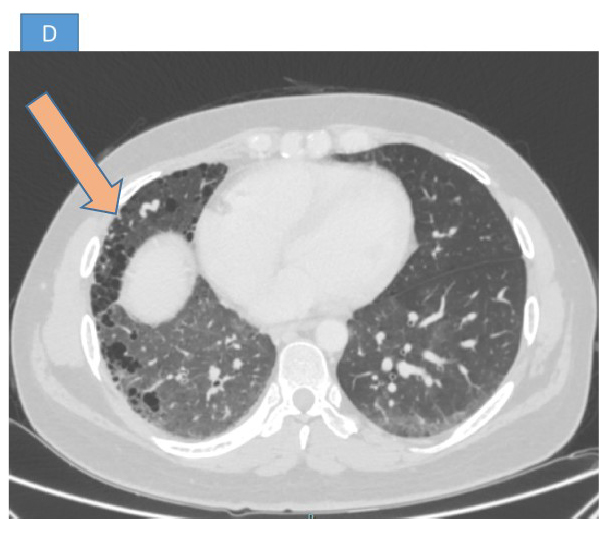
C and D - hypertrophic right bronchial arteries with multiple collaterals. Fibrotic and multicystic changes in right lung with reduced volume and compensatory left lung hyperinflation.
UNILATERAL RIGHT PULMONARY ARTERY ATRESIA
| Feature | Pulmonary Artery Agenesis | Pulmonary Artery Atresia |
|---|---|---|
| Primary Structural Abnormality | Complete absence of one pulmonary artery, including its origin and distal branches | Occlusion or failure of continuity of one pulmonary artery, often with distal branches present |
| Embryologic Basis | Failure of the sixth aortic arch to develop the PA and its derivatives | Interruption in the proximal sixth aortic arch connection with the pulmonary trunk |
| Pulmonary Parenchyma | Often hypoplastic but present; perfused via systemic collaterals | Also hypoplastic; typically perfused via MAPCAs or PDA |
| Vascular Findings | Main PA and hilar branches absent; intrapulmonary arteries may exist and are perfused via systemic collaterals | Proximal PA segment may be absent or narrowed; a stump is often present but not always identifiable |
| Bronchial Anatomy | Usually intact; may be hypoplastic in severe agenesis | Intact |
| Imaging Differentiation | No PA stump; complete absence of PA from origin to branches; systemic collaterals supply lung; distal intrapulmonary bed may exist but is disconnected | PA stump usually present; distal branches may be seen filled via MAPCAs or PDA; however, stump may be absent if atresia occurs early or is complete |
| Clinical Implications | Often asymptomatic; may present with hemoptysis or recurrent infections | Similar symptoms; treatment depends on distal PA presence and symptoms |
- Congenital absence or severe underdevelopment of one pulmonary artery (usually right), with preservation of the contralateral pulmonary circulation.
- Failure of the proximal sixth aortic arch to connect with the pulmonary trunk during development.
- Hemodynamics: Affected lung receives blood via systemic collaterals (MAPCAs) or patent ductus arteriosus (PDA).
- Associated Conditions: Tetralogy of Fallot, right aortic arch, VSD (if syndromic or complex case)
Chest X-ray (CXR) Findings
- Affected Side:
- Small hemithorax with volume loss
- Absent or diminished hilar vascular markings
- Mediastinal shift toward affected lung
- Unaffected Side:
- Hyperinflation and increased vascular markings
- Enlarged contralateral pulmonary artery
- Other Clues:
- Rib crowding on affected side
- Elevated hemidiaphragm
CT / CTA Findings
- Absent Pulmonary Artery:
- No visualization of one main/branch PA within ~1 cm of expected origin
- Possible blind-ending PA stump
- Collateral Circulation:
- Systemic collaterals (MAPCAs) from bronchial, subclavian, or aortic origins
- Contrast opacification of pulmonary parenchyma via systemic arteries
- Lung Parenchyma Changes:
- Hypoplastic lung with reduced vascularity
- Bronchiectasis, scarring, or chronic infection features
- Right vs. Left UAPA:
- Right UAPA is more common, especially in isolated cases. Left UAPA more often coexists with right?sided aortic arch or complex cardiac defects.
Clinical Relevance & Imaging Role
- Clinical Presentation:
- Often asymptomatic in childhood
- May present with recurrent infections, dyspnea, or hemoptysis
- Imaging Utility:
- CXR: Initial suspicion
- CT Angiography: Defines vascular anatomy, collateral supply, parenchymal effects
- MRI: Alternative in young patients for functional assessment
- Echocardiography: Evaluate associated cardiac anomalies
Treatment
- Treatment Tailored by:
- Age of presentation
- Symptomatology
- Associated cardiovascular anomalies
- Young Patients:
- Revascularization (systemic-to-pulmonary artery shunt) if distal PA formed
- Hemoptysis or Focal Infection:
- Lobectomy or selective embolization of systemic arterial supply
- Asymptomatic Adults:
- Risk of pulmonary hypertension remains
- Endothelin receptor antagonists may be considered
- Monitoring:
- ???????Regular follow-up with pulmonary hemodynamic surveillance recommended
REFERENCES
- Steiropoulos P, Archontogeorgis K, Tzouvelekis A, Ntolios P, Chatzistefanou A, Bouros D. Unilateral pulmonary artery agenesis: a case series. Hippokratia. 2013;17(1):73–6.
- Lee EY, Boiselle PM, Cleveland RH. Multidetector CT evaluation of congenital lung anomalies. Radiology. 2008;247(3):632–48.
- Ten Harkel ADJ, Blom NA, Ottenkamp J. Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest. 2002;122(4):1471–7. doi:10.1378/chest.122.4.1471.
- Sadikot RT, Suresh MV. Unilateral absence of the left pulmonary artery with an associated vascular anomaly in adulthood. Cureus. 2016;8(3):e527. doi:10.7759/cureus.527.
Dr. DEEPTI H V
CONSULTANT RADIOLOGIST
MANIPAL HOSPITAL , YESHWANTHPUR, BENGALURU
Dr. VINEETH BABY
FELLOW IN CROSS SECTIONAL IMAGING
MANIPAL HOSPITAL , YESHWANTHPUR, BENGALURU