A 62-year-old gentleman presented with on and off swelling in the left middle finger associated with difficulty in folding the finger.
- A 62-year-old gentleman presented with on and off swelling in the left middle finger associated with difficulty in folding the finger.
- On examination, tenderness was noticed over the region of proximal inter phalangeal joint.
- Further evaluation with MRI of left 3rd digit was suggested.
Imaging:
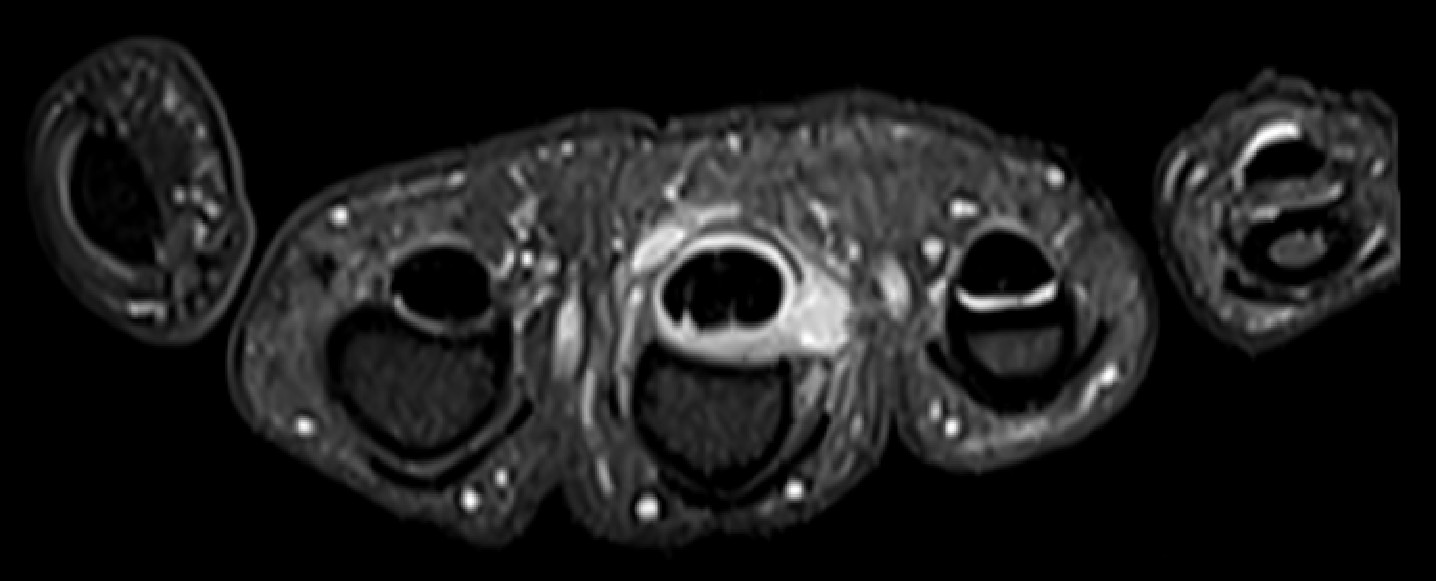
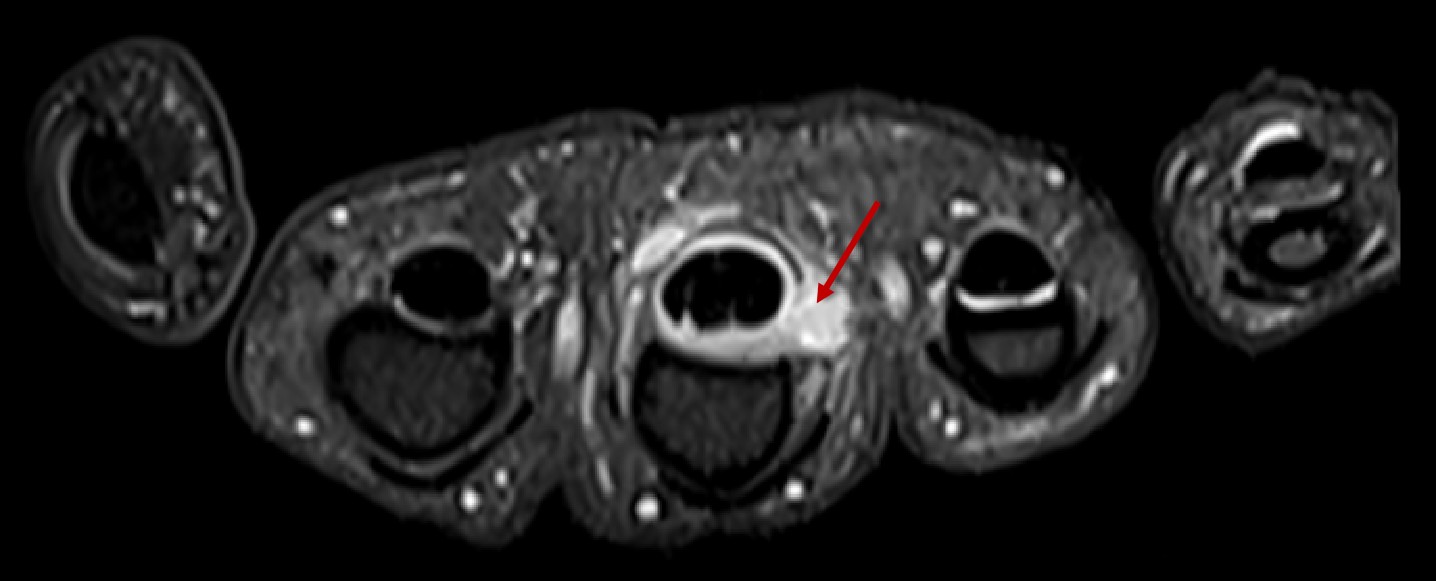
- PDFS axial image at the level of proximal phalanx.
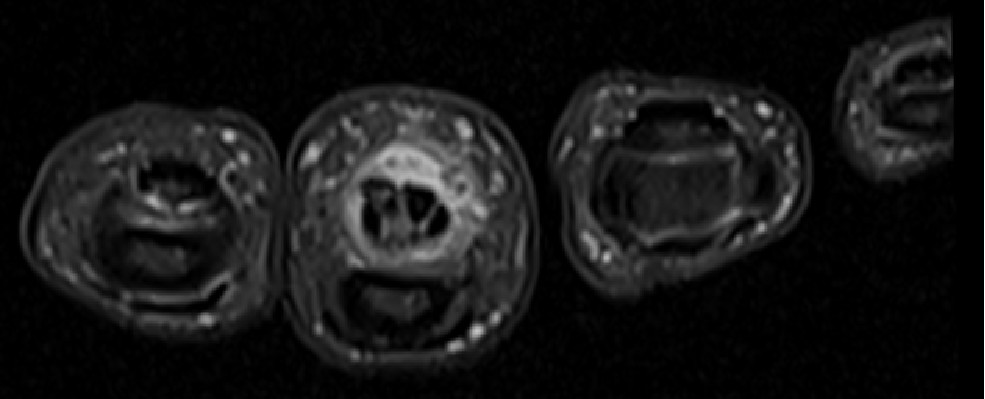
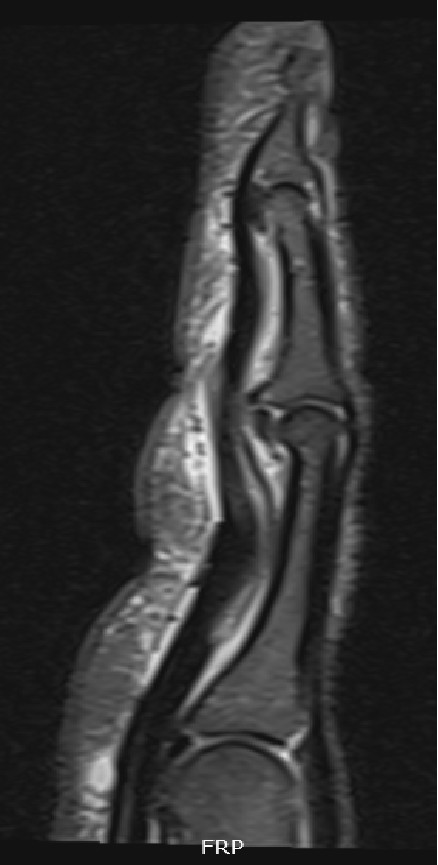
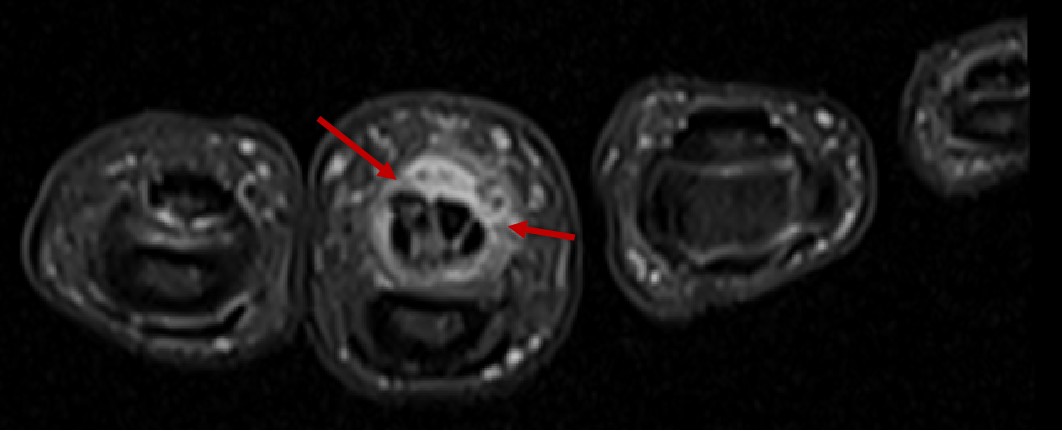
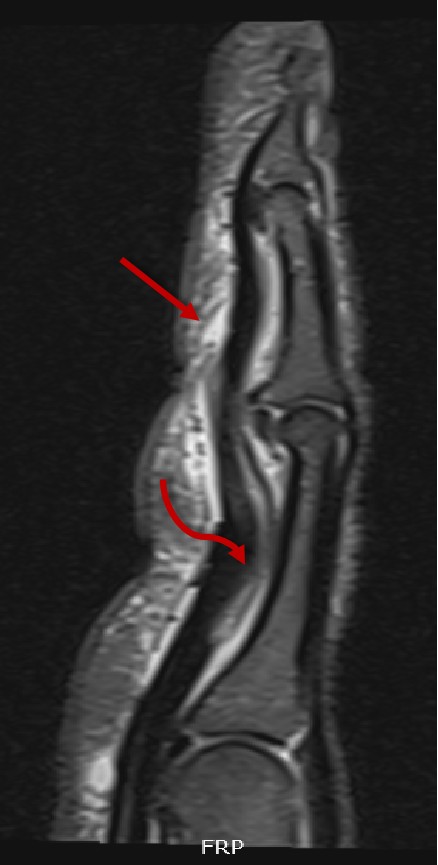
- PDFS axial (at the level of mid proximal phalanx) and sagittal images.
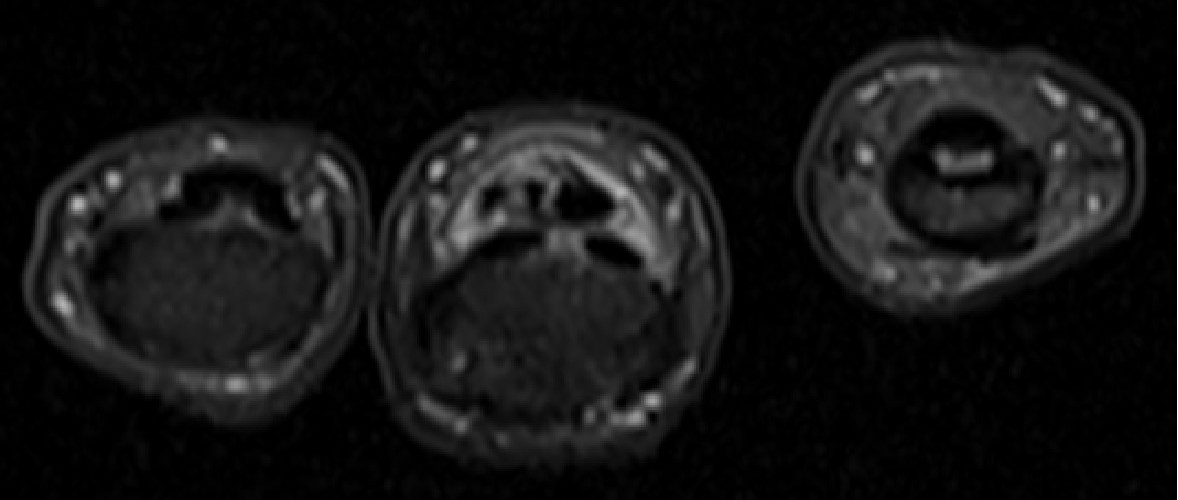
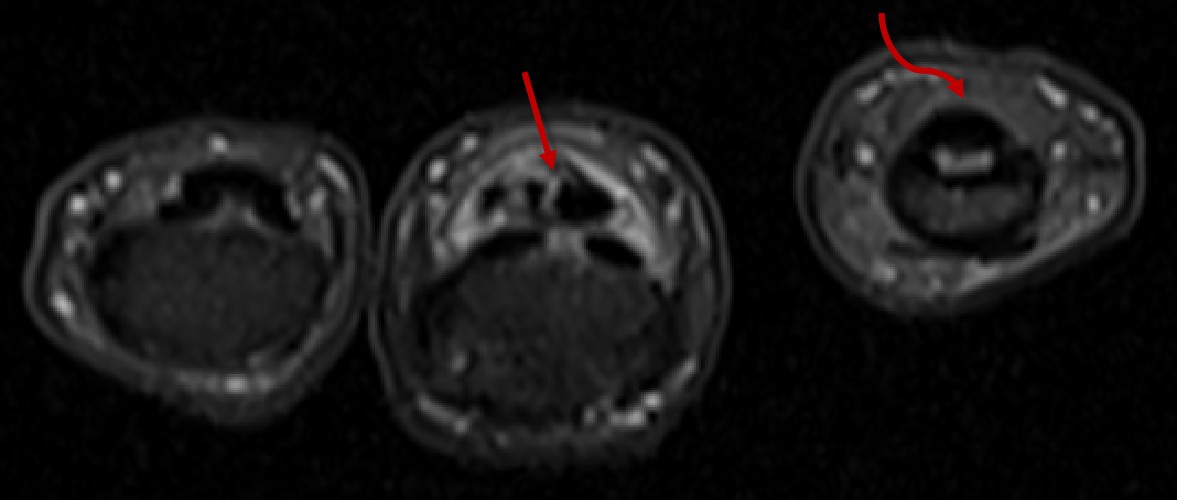
- PDFS axial (at the level of middle phalanx) and coronal images.
- Ulnar side rupture of the A2 pulley around the proximal phalanx with fluid filled outpouching. (red straight arrow)
- Mild thickening of the tendon sheath around FDP and FDS tendons with mild fluid within the tendon sheath. (red straight arrow)
- Bowstringing of the flexor tendon with increased distance between the tendon and phalanx. (red curved arrow)
- Partial thickness longitudinal tear of the FDP tendon extending from mid proximal phalanx to mid middle phalanx with surrounding tendinosis. (red straight arrow)
- Ulnar side rupture of the A2 pulley around the proximal phalanx with fluid filled outpouching. (red straight arrow)
- Mild thickening of the tendon sheath around FDP and FDS tendons with mild fluid within the tendon sheath. (red straight arrow)
- Bowstringing of the flexor tendon with increased distance between the tendon and phalanx. (red curved arrow)
- Partial thickness longitudinal tear of the FDP tendon extending from mid proximal phalanx to mid middle phalanx with surrounding tendinosis. (red straight arrow) Normal tendon of 4th digit. (red curved arrow)
- Ulnar side rupture of the A2 pulley around the proximal phalanx with fluid filled outpouching causing bowstringing of the flexor tendon. (primary diagnosis)
- Partial thickness longitudinal tearing of the FDP tendon extending from mid proximal phalanx to mid middle phalanx with surrounding tendinosis. Tenosynovitis in the FDS/FDP tendon sheath. (associated secondary findings as a consequence of primary pathology)
Discussion:
Introduction, Anatomy:
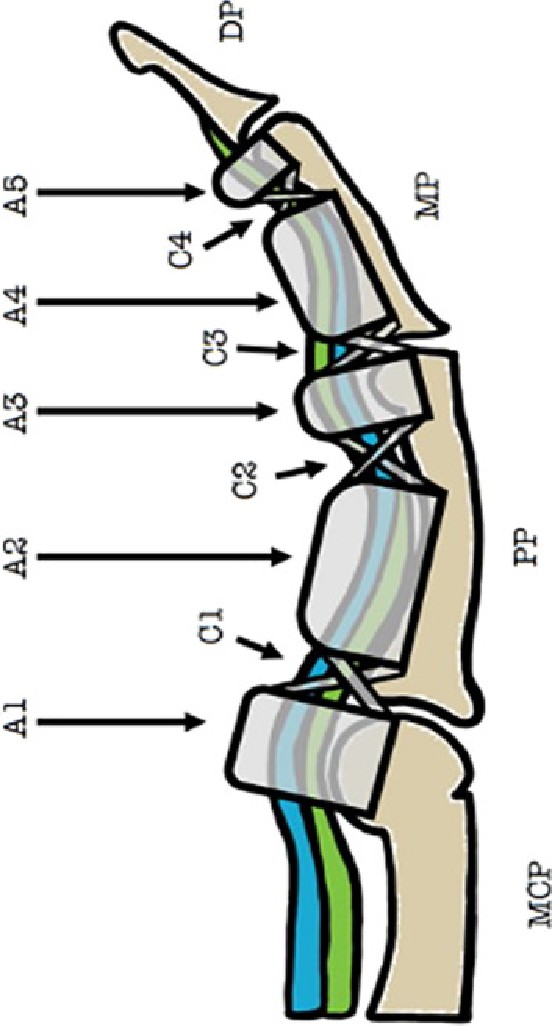
- The annular and cruciate pulleys are areas of focal thickening of the flexor tendon sheath that are of critical importance to the normal biomechanical function of the finger.
- They assure proper movement and apposition of the flexor tendons relative to the adjacent osseous structures.
- Eight functional pulleys are found at each finger, extending from the volar plate of the metacarpal-phalangeal joint to the base of the distal phalanx. The five annular pulleys (A1-A5) are the stronger and more functionally important pulleys, whereas the cruciate pulleys (C1-C3) are important to the intrinsic strength of the flexor tendon sheath. Of these, the A2 pulley is the strongest and has significant functional role. Injuries are seen to usually involve, A2, A3 and A4 pulleys.
| Pulleys of 2nd–5th fingers | Levels and attachments of the pulleys |
|---|---|
| A1 | Metacarpophalangeal Joint (Volar plate and head of the metacarpal) |
| A2 | Proximal and mid-diaphysis of the proximal phalanx |
| C1 | Between the A2 and A3 pulleys |
| A3 | Proximal interphalangeal joint (Volar plate and head of the proximal phalanx) |
| C2 | Between A3 and A4 pulleys |
| A4 | Mid-diaphysis of the middle phalanx |
| C3 | Between A4 and A5 pulleys |
| A5 | Distal interphalangeal joint (Volar plate and head of the middle phalanx) |
PATHOPHYSIOLOGY, CLINICAL PROFILE:
- Pulley injuries are an overuse phenomenon, occurring in rock climbers because of the repetitive, excessive forces placed upon the fingers during the activity.
- Biomechanical analysis has shown that injury to the A2 pulley likely occurs when the pulley is eccentrically loaded, resulting in high tensile forces between the pulley and tendon and has been reported in rock climbers, traumatic cases, baseball players, bowlers, and other persons who engage in activities that involve a sudden extension force applied to an acutely flexed digit.
- When the A2 pulley is significantly injured, bowstringing of the flexor tendons occurs, which can lead to a range of motion loss and reduced finger function. Bowstringing is a result of the flexor tendon gaining an increased mechanical advantage over the extensors, causing the tendon to separate from the phalanx and restrict digit extension.
PATHOPHYSIOLOGY, CLINICAL PROFILE:
- Patients with acute pulley injuries may report a sudden onset of pain coinciding with a slip or forceful maneuver, limited range of motion and an audible pop may be heard.
- Chronic injuries are caused by repetitive microtrauma to the pulley, which can lead to symptoms of focal tenderness, limited range of motion and pain while gripping.
- Bowstringing is generally considered to be indicative of a major A2 pulley injury
- However, the diagnosis of a pulley lesion may be challenging, as pain, swelling, and limited range of motion makes the physical examination difficult and clinicians have to rely on imaging to make the diagnosis.
IMAGING: MRI
- MRI helps in the early diagnosis and grading of pulley injuries. Schöffl et al. graded pulley injuries as follows:
- Grade 1: Sprain of the pulley - seen as edema within and adjacent to the pulley with no disruption of fibers.
- Grade 2: Partial tear of A2/A3 pulleys or complete tear of A4 pulley - partial discontinuity of the pulley with edema (fluid) superficial and deep to the pulley. There is no significant increase in the distance between the tendon and the underlying bone.
- Grade 3: Complete tear of A2/A3 pulleys - there is non-visualization of the pulley with fluid intensity at the site of the injury (direct sign) and increased gaps between the flexor tendon and underlying bone (indirect sign)
- Grade 4: Multiple pulley tear or single pulley tear associated with injuries lumbricals or collateral ligaments. Grade 4 injuries require surgical intervention.
- The pulley system of the finger is often difficult to visualize on routine sagittal MR images. Normal pulleys can be visualized by utilizing MR tenography, but this invasive technique is rarely performed. In patients with tenosynovitis, the fluid within the tendon sheath provides a physiologic tenogram, and outlines the pulleys, particularly the larger A2 and A4 pulleys.
- Sometimes it may be difficult to visualize the finger pulley even in uninjured patients. Relying completely on direct visualization of the torn pulleys on axial images may lead to over or under diagnosis of pulley injury. The presence of bowstringing, tenosynovitis, fluid surrounding the pulley, pulley thickening, or the presence of cysts may serve as indirect signs of pulley injury.
- In case of suspected pulley injury, another PDFS sagittal image is acquired in a flexed position. In this position, there is an increase in the gap as compared to the neutral position which is referred to as the “bowstring sign”. The longitudinal extent and degree of the bowstringing of the tendon from bone depend on the number of pulleys injured. A comparison is done of this gap with the adjacent uninjured finger on axial images.
IMAGING: ULTRASOUND
- “Bowstringing” may be exaggerated if the patient is scanned in forced flexion, which is accomplished by having the patient flex the finger while pushing the tip of the finger against a firm surface by the use of dynamic ultrasound, which has been found to be sensitive for both A2 and A4 pulley ruptures. With ultrasound the distance between the flexor tendon and the phalanx can be measured in forced flexion, with abnormal separation of greater than 1mm being seen in pulley injuries. With complete A2 pulley ruptures, separation of greater than 3mm is often present.
- Additionally, we may also see fluid along the pulley or within the flexor tendon sheath, flexor tendon sheath cyst, presence of fibrous tissue, PIP or DIP joint fluid, or irregular thickening of the A2 pulley
- However, ultrasound lacks the soft-tissue contrast and resolution of MR, is more operator dependent, and lacks sensitivity for associated osseous or intrinsic tendon injuries that may be found in this patient group.
CONCLUSION:
- Pulley injuries can be either secondary to overuse or trauma and may cause significant functional distress to the patient. Lower grade injuries can be managed conservatively, however, higher grade injuries require surgical intervention.
- MRI allows accurate diagnosis in these patients and helps assess the extent and grade of injury while at the same time it is able to provide a simultaneous evaluation for occult osseous, ligamentous, or intrinsic tendon injuries.
REFERENCES:
- https://radsource.us/pulley-lesion-of-the-fingers/
- Berrigan W, White W, Cipriano K, Wickstrom J, Smith J, Hager N. Diagnostic Imaging of A2 Pulley Injuries: A Review of the Literature. J Ultrasound Med. 2022 May;41(5):1047-1059. doi: 10.1002/jum.15796. Epub 2021 Aug 2. PMID: 34342037; PMCID: PMC9292555.
- Desai S, Gaitonde A, Subramanian S, Lokhande P, Asthana K. 3T-MRI of finger pulleys - Review of anatomy and traumatic conditions involving them. Indian J Musculoskelet Radiol. 2023;5:77-81. doi: 10.25259/IJMSR_22_2023.
Dr Deepti H V
Senior Consultant Radiologist
MHRG, Manipal Hospital, Yeshwanthpur
Dr Kanupriya Grover
Cross Sectional Imaging Fellow
MHRG, Manipal Hospital, Yeshwanthpur