Patient presented in ER with history of not passing urine and stools since 1 day Complains of abdominal discomfort and 5 episodes of vomiting.
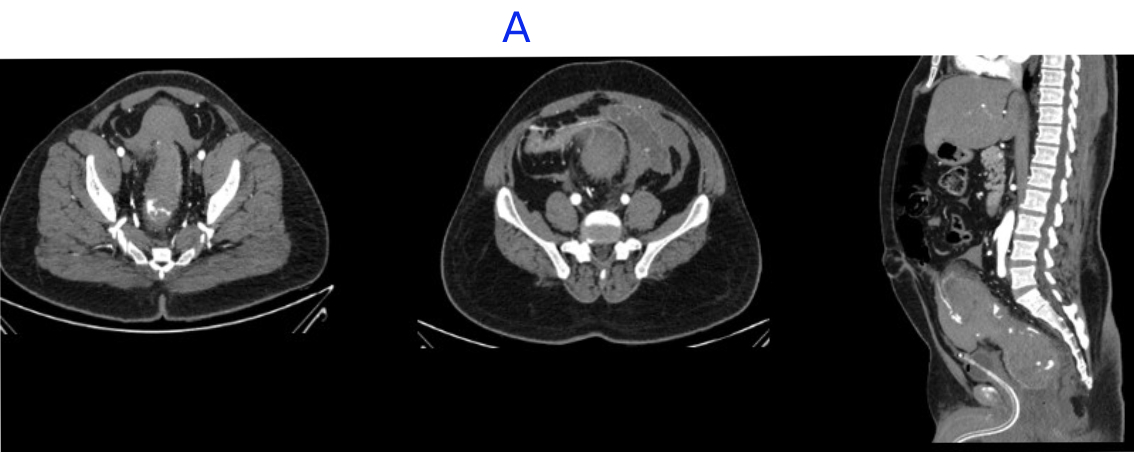
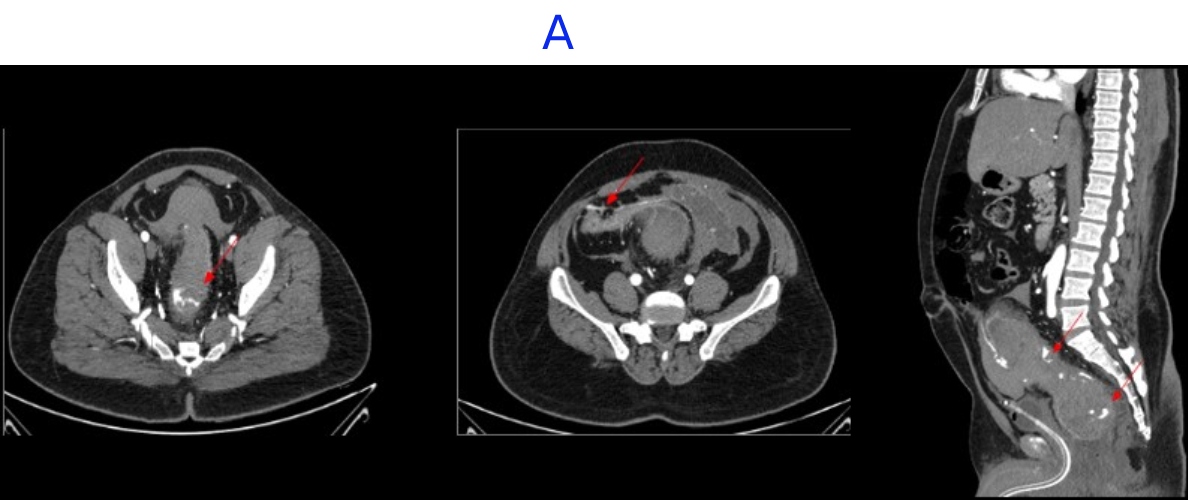
A. LEGENDS
- Large intramural hematoma with significant adjacnet fat starnding noted in rectum and distal sigmoid causing significant luminal narrowing.
- Multiple area of contrast extravasation within the hematoma which shows increase in size in venous and delayed phases with multiple pools of contrast - suggesting active bleeding from branches of inferior mesenteric artery..
- Distal rectum and proximal sigmoid colon mild edematous wall thickening.
- Hemorrhagic fluid noted in bilateral paracolic gutter and pelvis with active contrast extravasation.
- Omentomesenteric fat stranding in lower abdomen with mesorectal fascial thickening noted.
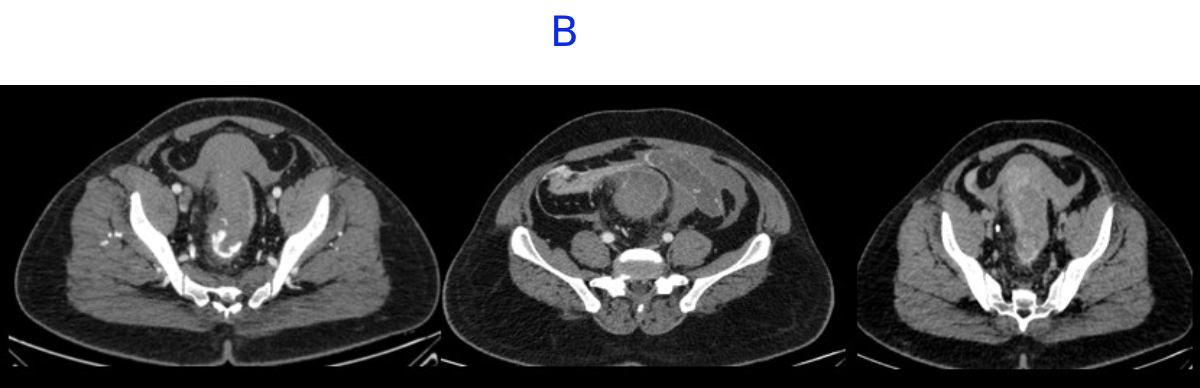
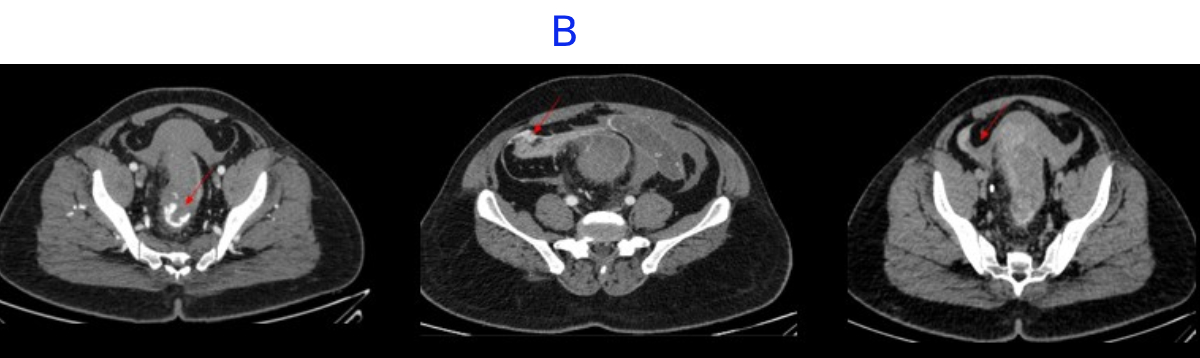
B. LEGENDS
- Distal rectum and proximal sigmoid colon mild edematous wall thickening.
- Hemorrhagic fluid noted in bilateral paracolic gutter and pelvis with active contrast extravasation.
- Omentomesenteric fat stranding in lower abdomen with mesorectal fascial thickening noted.
DIAGNOSIS
- INTRAMURAL RECTAL AND DISTAL SIGMOID HEMATOMA WITH ACTIVE BLEEDING
DISCUSSION
Intramural hematoma of the colon - rare entity
Features:
- Gastrointestinal bleeding,
- Progressive secondary anemia,
- Abdominal pain
- Bowel obstruction with hemorrhagic shock.
Causes:
- Blunt abdominal trauma, particularly in patients receiving anticoagulant therapy or those with coexisting bleeding disorders.
- Colorectal malignancies, in the absence of trauma or anticoagulation therapy
- Idiopathic intramural hematomas of the colon - exceedingly rare.
- Increased abdominal pressure during straining may play an important role in hematoma formation, especially in patients on anticoagulant therapy -
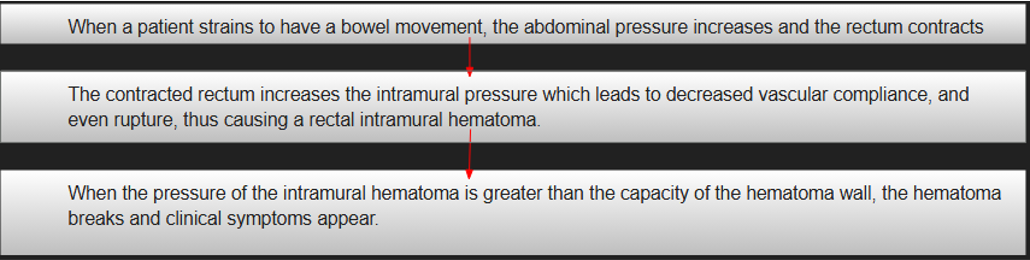
Pathophysiology
INVESTIGATIONS
- CT with intravenous contrast
- colonoscopy are primary diagnostic modalities for intramural hematomas of the colon.
- Endoscopic ultrasonography - additional information on wall thickness, extent of involvement, and adjacent tissue damage
MANAGEMENT STRATEGIES
- Conservative management- anticoagulation reversal, parenteral nutrition, and intravenous hydration, is preferred for hemodynamically stable patients.
- Endoscopic techniques - hemostatic clip application, mucosal incision with hematoma evacuation, and ultrasound-guided fine-needle aspiration, offer less invasive alternatives to surgery.
- Transcatheter arterial embolization - highly effective, but carries a 20% complication rate, including perforation, ischemia, and intestinal wall necrosis.
- Surgical resection is the standard approach for hemodynamically unstable patients or those with complications such as peritonitis, intestinal wall necrosis, obstruction, or perforation.
Clots tend to form first near the site of bleeding -thus, the identification of a heterogeneous and relatively higher attenuation clot allows localization of the site of hemorrhage - SENTINEL CLOT SIGN
On contrast-enhanced CT - active hemorrhage- usually serpiginous high-attenuation foci nearly isodense to adjacent vessels.

REFERENCES
Kula, Joanna MDa; Szmigiel, Pawe? MDb; Rusinowski, Cezary MDb; Mrowiec, S?awomir MD, PhDb; Wosiewicz, Piotr MD, PhDc,*. Extensive spontaneous intramural hematoma of rectum and sigmoid colon in a patient undergoing anticoagulant therapy: A case report. Medicine 104(22):p e42428, May 30, 2025. | DOI: 10.1097/MD.0000000000042428
Dr Rajesh Helavar
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr Neha Sathyanarayana
Radiology Resident
Manipal Hospital, Yeshwanthpur, Bengaluru.