49 year male, presents with abdominal pain since 3 days. No h/o loose stools, vomiting.
HISTORY AND CLINICAL EXAMINATION
49 year male, presents with abdominal pain since 3 days. No h/o loose stools, vomiting.
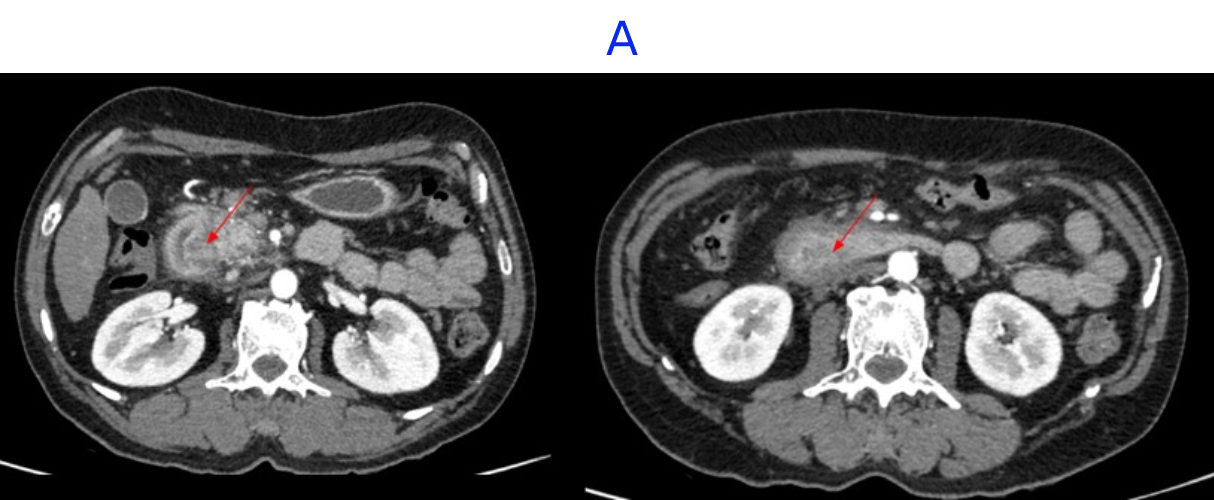
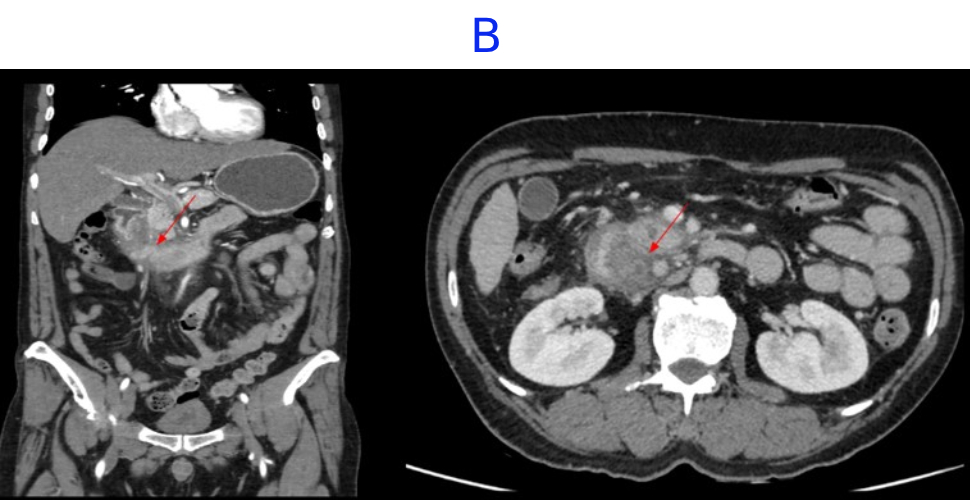
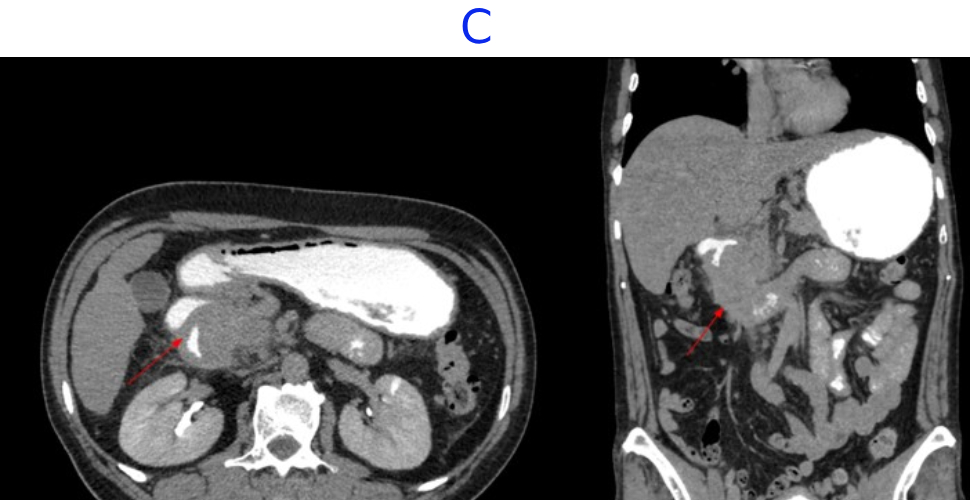
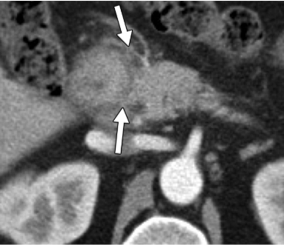
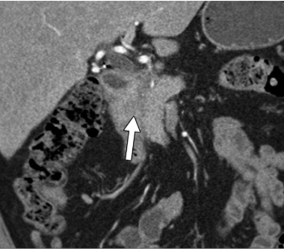
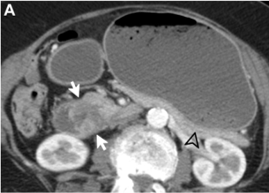
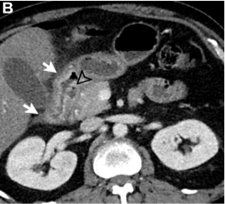
- A. Circumferential irregular submucosal wall thickening noted in D2 and D3 segment of duodenum causing luminal narrowing.
- B. Few hypoenhancing areas within the medial wall of duodenum. Uncinate process of pancreas appears oedematous.
- C. Contrast is seen passing from the duodenum into the jejunum. No contrast leakage noted.
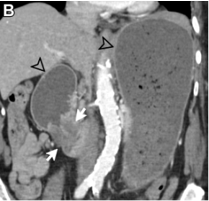
PET-CT
- FDG avid heterogeneously enhancing lesion exophytic growth / thickening in D2/D3 segment of duodenum- likely malignant.
- FDG avid upper abdominal nodes.
DIAGNOSIS
Differential include:
- Inflammatory duodenal mass.
- Groove pancreatitis.
- Duodenal neoplastic etiology [Submucosal].
DISCUSSION
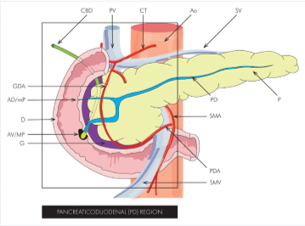
THE PANCREATICODUODENAL GROOVE
The pancreaticoduodenal groove (PDG) is a small space between the pancreatic head and duodenum where vital interactions between multiple organs and physiologic processes take place.
SPECTRUM OF PATHOLOGIES
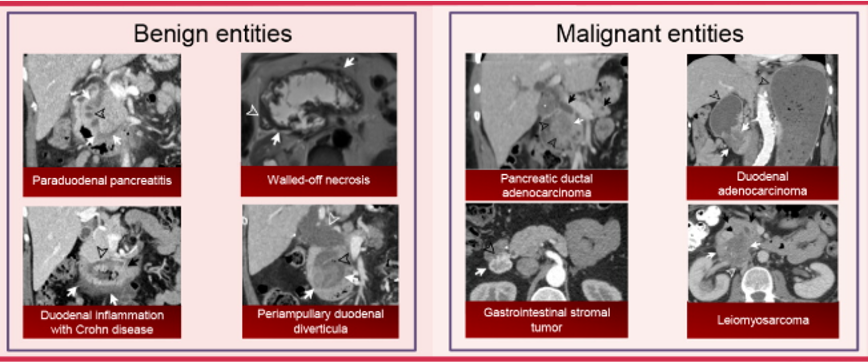
PARADUODENAL PANCREATITIS (PDP)
Paraduodenal pancreatitis (PDP)/groove pancreatitis, is a form of focal chronic pancreatitis involving the PDG.
The pathogenesis of PDP is not entirely clear but is thought to be related to ectopic pancreatic rests in the medial duodenal wall .
Chronic inflammation in this space results in sheetlike crescentic fibrotic soft-tissue expansion of the PDG.
In the pure form, the appearance can range from ill-defined fat stranding and inflammatory change in the groove between the pancreatic head and duodenum, to frank soft tissue in the groove.
This soft tissue often has a “sheetlike” curvilinear crescentic shape that is best appreciated on coronal images.
If multiphase imaging is performed, this soft tissue tends to show increasing delayed enhancement as a result of a significant fibrotic component.
There can be of the medial duodenal wall (particularly on the coronal images), and small cysts are a common feature either within the thickened duodenal wall or the pancreaticoduodenal groove itself.

Ampullary or duodenal adenocarcinoma may also manifest as infiltrative soft tissue extending to the PDG and be difficult to differentiate from inflammation.
Duodenal adenocarcinoma can manifest as :
- a focal mass or involve the duodenal wall circumferentially
- may have an infiltrative component involving the adjacent fat planes, encasing vascular structures
- nodal or distant metastatic disease.
- When this tumor arises in close proximity to the ampulla, it can involve and obstruct the biliary and pancreatic ducts and result in the double duct sign, similar to primary ampullary adenocarcinoma

DUODENAL INFLAMMATION
Duodenal inflammation—evidenced by circumferential wall edema appearing striated hyperenhancing mucosa, and periduodenal stranding—is most commonly seen as reactive to external processes such as acute pancreatitis and cholecystitis.
Infectious duodenitis :Mycobacterium avium-intracellulare (MAI) or cytomegalovirus (CMV) in the context of HIV infection or AIDS
Inflammatory duodenitis -after radiation exposure, with immunoglobulin A (IgA) vasculitis (formerly Henoch-Schönlein purpura), and in Crohn disease.
Findings of duodenitis are nonspecific; therefore, clinical correlation and evaluation of adjacent organs are key to making a unifying diagnosis.
Peptic ulcer disease - most frequently affects the duodenal bulb, which forms the superior border of the PDG. Small ulcers may be occult at imaging, and most are evident only when leading to perforation, with associated wall thickening, periduodenal fluid, and extraluminal air.
Peptic ulcer disease is the most common cause of abnormal gas in the PDG.

Approach to Entities Involving PDG
- Expansion of the space between the pancreatic head and duodenum is to be expected, with medial displacement of the pancreatic head and a laterally shifted duodenum- likely arising from the groove
- If both pancreas and duodenum are displaced in the same direction, the lesion is most likely located outside the groove
- Presence or absence of biliary and pancreatic duct obstruction degree and morphology of upstream ductal dilatation Effect on adjacent vascular structures -mesenteric and portal veins and the pancreaticoduodenal artery Rarer ancillary features such as abnormal air, hemorrhage, and fistulization can also be helpful if present.
MANAGEMENT
RESECTION OF ADENOMA
REFERENCES
Pancreaticoduodenal Groove: Spectrum of Disease and Imaging Features Hernan R. Bello,, Aarti Sekhar, Ross W. Filice, Amir Reza Radmard, and Amir H. Davarpanah https://doi.org/10.1148/rg.210168
Groove Pancreatitis: Spectrum of Imaging Findings and Radiology-Pathology Correlation Authors: Siva P. Raman, Safia N. Salaria, Ralph H. Hruban, and Elliot K. FishmanAUTHOR INFO & AFFILIATIONS Volume 201, Issue 1 https://doi.org/10.2214/AJR.12.9956
Dr MADHU KUMAR S B
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr NIKITHA U N
Radiology Resident Manipal Hospital,
Yeshwanthpur, Bengaluru.