A 37-year-old male presented with dyspnea on minimal exertion and recurrent cough since 2 weeks
Clinical Features
- A 37-year-old male presented with dyspnea on minimal exertion and recurrent cough since 2 weeks
DIAGNOSIS
- Silicosis with progressive massive fibrosis
DISCUSSION
SILICOSIS WITH PROGRESSIVE MASSIVE FIBROSIS:
- Silicosis is a chronic occupational pneumoconiosis caused by prolonged inhalation of crystalline silica dust, commonly affecting workers in mining, quarrying, sandblasting, and stone cutting industries.
- Silicosis is a chronic occupational pneumoconiosis caused by prolonged inhalation of crystalline silica dust, commonly affecting workers in mining, quarrying, sandblasting, and stone cutting industries.
- Progressive massive fibrosis (PMF) represents the most severe and advanced form of silicosis and results from the coalescence of smaller silicotic nodules into large fibrotic masses.
- PMF is characterized by upper lobe predominant conglomerate masses associated with architectural distortion, volume loss, and compensatory emphysematous changes.
- The condition is progressive even after cessation of exposure, reflecting ongoing inflammatory and fibrotic responses to retained silica particles.
Imaging Features:
Chest Radiograph
- Multiple small, rounded opacities (2–5 mm) predominantly in the upper lung zones, consistent with simple silicosis.
- Coalescence of nodules forming large, bilateral, irregular opacities (>10 mm), typically in the posterior segments of the upper lobes.
- Progressive massive fibrosis appears as large conglomerate masses with:
- Upward and medial retraction of the hila
- Upper lobe volume loss
- Peripheral compensatory emphysema, often para-cicatricial.
- Eggshell calcification of hilar and mediastinal lymph nodes (highly suggestive but not pathognomonic).
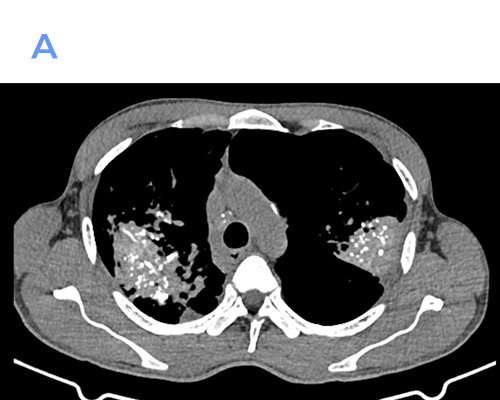
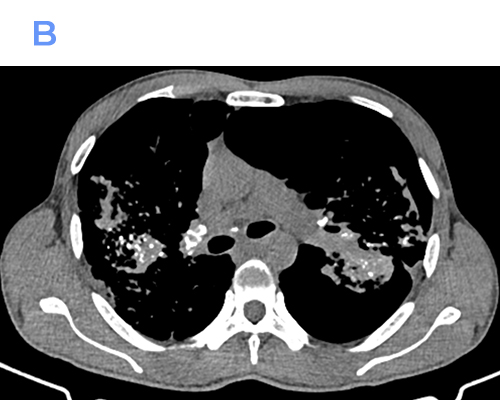
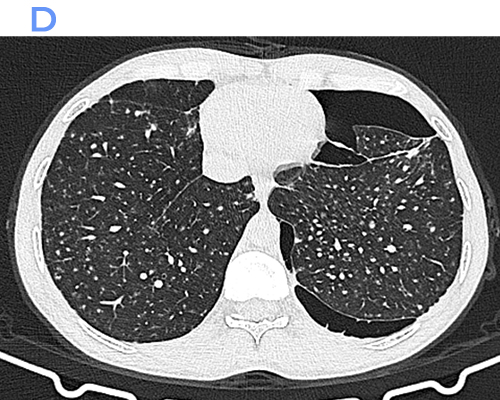
Computed Tomography (CT)
- Numerous well-defined centrilobular and perilymphatic nodules in the upper lobes.
- Conglomerate fibrotic masses with irregular margins and variable internal calcification.
- Traction bronchiectasis and bronchiolectasis adjacent to fibrotic areas.
- Marked architectural distortion with posterior and superior displacement of fissures.
- Enlarged hilar and mediastinal lymph nodes, frequently showing peripheral (“eggshell”) calcification.
- Areas of emphysema, especially adjacent to fibrotic masses.
CT is superior in detecting early PMF, subtle nodal calcifications, and complications such as superimposed infection or lung cancer.
Differential Diagnosis :
Coal Workers’ Pneumoconiosis (PMF)
- Similar imaging appearance; differentiation relies on occupational history.
- Coal workers’ PMF tends to show more central distribution and less nodal calcification.
Pulmonary Tuberculosis
- May coexist with silicosis.
- Cavitation, tree-in-bud nodules, and systemic symptoms favor tuberculosis.
Sarcoidosis
- Upper-lobe fibrosis with conglomerate masses.
- More symmetrical lymphadenopathy; nodules along bronchovascular bundles.
Lung Carcinoma
- Solitary or dominant mass with spiculated margins.
- PMF masses are usually bilateral, symmetric, and slowly progressive.
Chronic Hypersensitivity Pneumonitis
- Upper-lobe fibrosis but associated with ground-glass opacities and mosaic attenuation.
References
- Leung CC, Yu IT, Chen W. Silicosis. Lancet. 2012;379(9830):2008–18.
- Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246(3):697–722.
- Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics. 2006;26(1):59–77.
- Webb WR, Müller NL, Naidich DP. High-Resolution CT of the Lung. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2014.
- Craighead JE, Abraham JL, Churg A, et al. Diseases associated with exposure to silica and nonfibrous silicate minerals. Arch Pathol Lab Med. 1988;112(7):673–720.
Dr Deepti H V
DMRD, DNB, EDiR
Senior Consultant Manipal Hospitals Radiology Group Yeshwantpur
Dr S Shreya
MBBS, MD
Cross section imaging fellow - MHRG