A 33 year old male, History of proptosis in both eyes since 2 years. Headache and vertigo since 2 years. History of intermittent fever. No history of seizures.
A 33 year old male, History of proptosis in both eyes since 2 years. Headache and vertigo since 2 years. History of intermittent fever. No history of seizures.
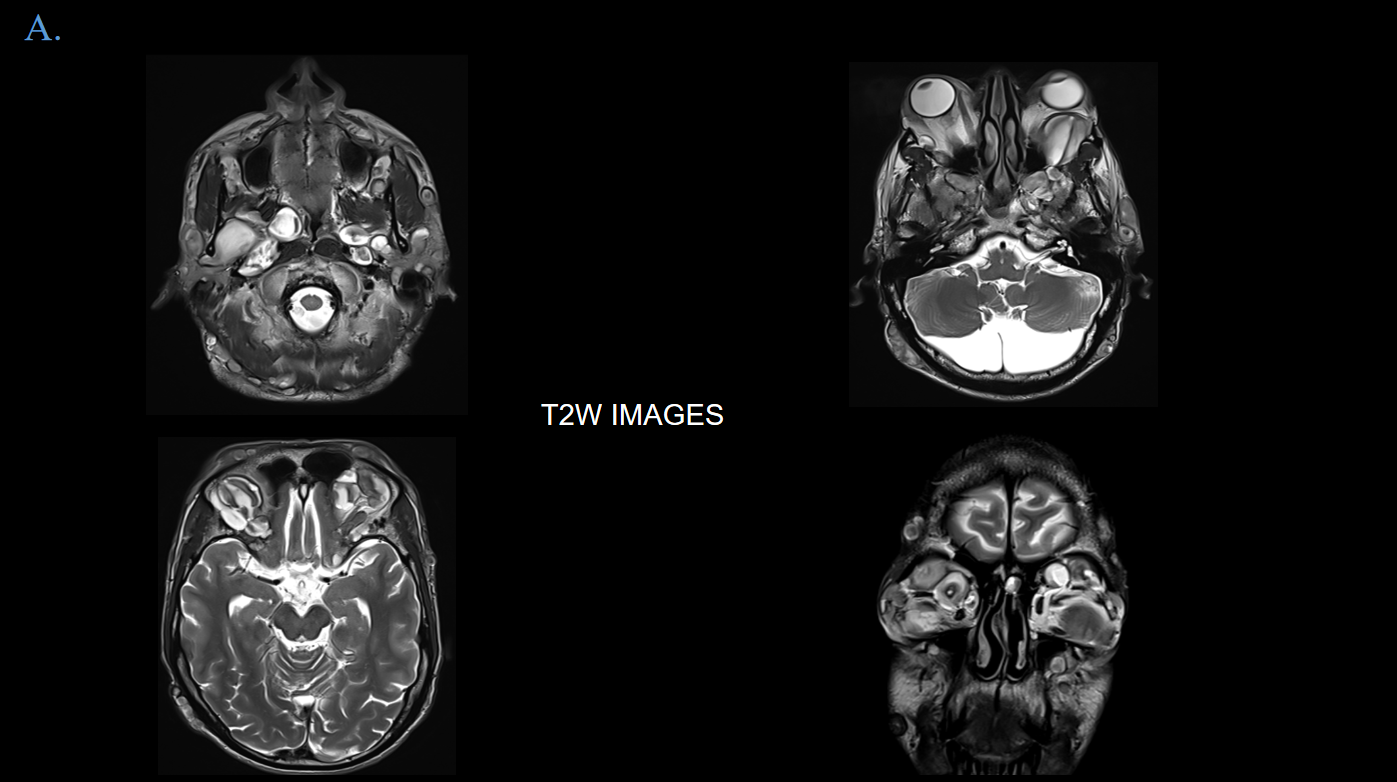
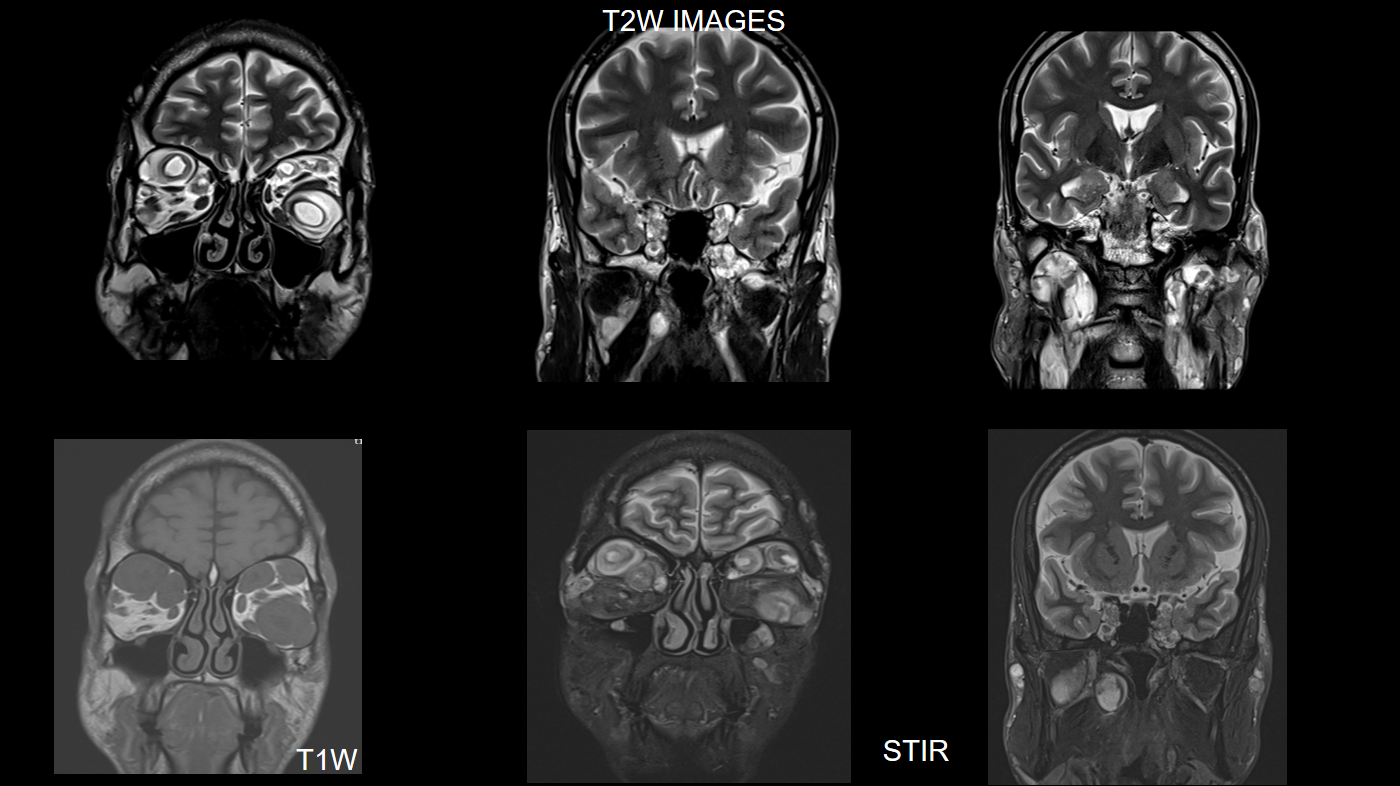
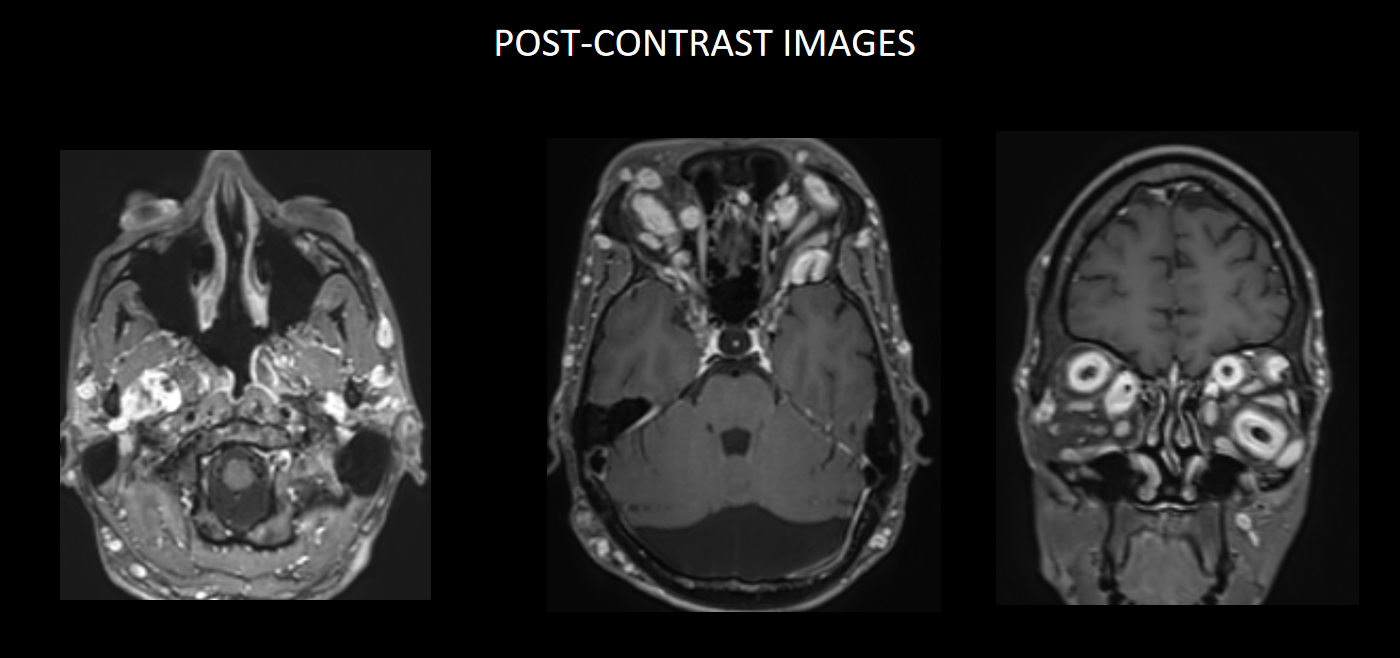
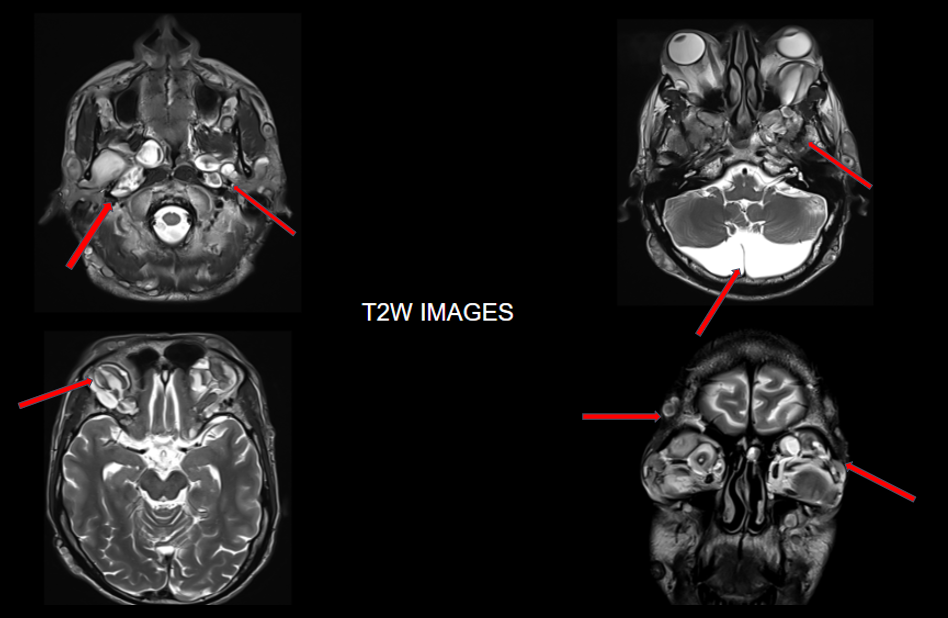
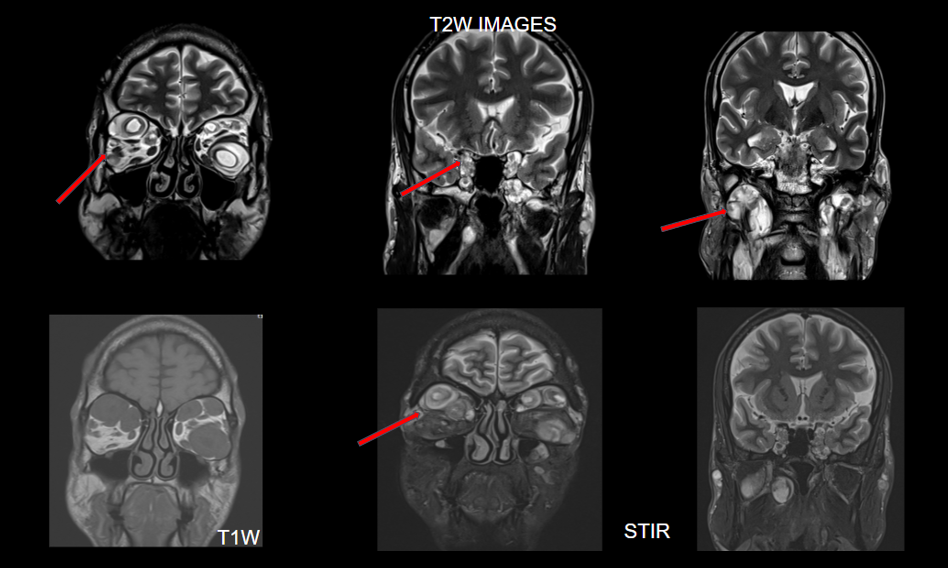
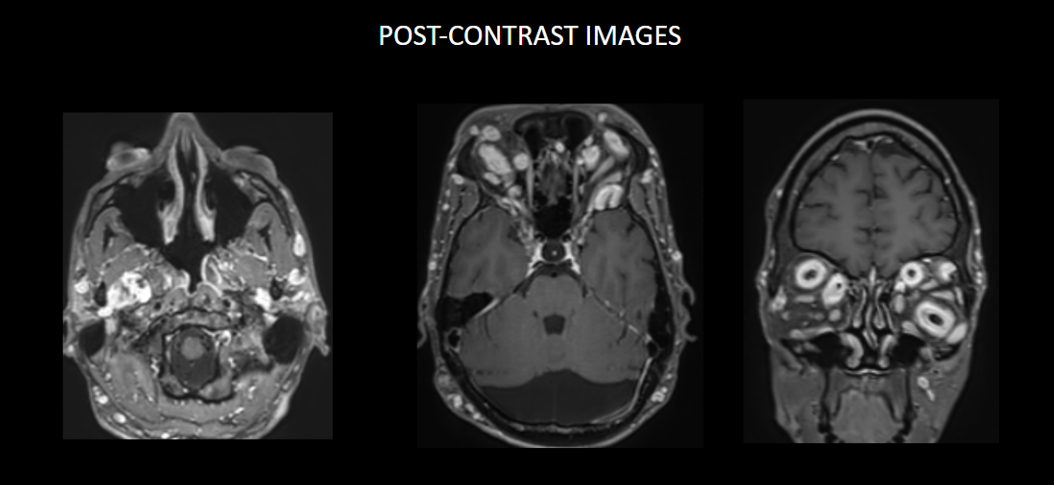
FINDINGS – MRI BRAIN WITH IV CONTRAST
Multinodular T2 hyperintense hypointense transpatial lesions seen within the bilateral orbits occupying the intra and extraconal spaces with targetoid appearance.
The lesion extends through the inferior orbital fissure into the pterygopalatine fossa bilaterally.
The lesions also extend through the foramen ovale into the superior aspect of masticator space bilaterally.
Similar heterogeneously enhancing nodular lesions are also seen bilateral fronto-temporal and occipital scalp regions. Incidental retrocerebellar arachnoid cyst.
Lesion extends into the orbital apex and along the bilateral cavernous sinuses.
Similar heterogeneously enhancing nodular lesions are seen extending into the upper neck in bilateral parotid and the visualised level II regions.
The lesions show heterogenous post-contrast enhancement.
Extensive orbitofacial plexiform neurofibroma.
DISCUSSION:
Neurofibromatosis type 1 (NF1) or von Recklinghausen disease is an inherited autosomal dominant disorder and the most common of the phakomatoses (neurocutaneous syndromes).
Pathogenesis involves mutations in the NF1 gene that encodes the protein neurofibromin. Some common clinical manifestations include café au lait macules, axillary or inguinal freckling, Lisch nodules (iris hamartomas), and neurofibromas.
The 3 general types of neurofibroma are cutaneous, nodular, and plexiform.
Plexiform neurofibroma is a type of peripheral nerve sheath tumor, and it is essentially pathognomonic of NF1.
These tumors develop from angiogenic and invasive Schwann cells that create either a superficial overgrowth of skin and soft tissues or a deep palpable cord of thickened nerves.
Plexiform neurofibroma occur in utero or in early childhood and are found in approximately 30 to 40% of individuals with NF1.
Plexiform neurofibromas which infiltrate the orbit can involve the intra-orbital cranial nerves, such as branches of the ophthalmic branch of the trigeminal nerve and infraorbital nerve.
They can then exert mass effect and displace the orbital content, including the extraocular muscles and globe, as well as result in secondary skeletal dysplasias.
Other features which can occur concomitantly with orbital encroachment by plexiform neurofibromas include proptosis, sphenoid wing dysplasia and buphthalmos.
On CT imaging, they appear as contrast-enhancing, irregular, soft-tissue masses with associated distortion of the normal anatomy of the eyelid, periorbital soft tissues and orbital contents.
They are best visualised on fat suppressed T2 weighted MR imaging where they appear as hyperintense masses with or without multiple target signs.
They demonstrate mild enhancement with IV gadolinium and are isointense on T1 signal.
They demonstrate mild enhancement with IV gadolinium and are isointense on T1 signal.
Malignant peripheral nerve sheath tumours arising from plexiform neurofibromas are aggressive tumours which have a tendency to metastasize widely and are associated with a poor prognosis.
MRI findings which indicate malignant transformation include:
- Perilesional oedema
- Irregular tumour shape
- Large size
- Rapid growth of mass on interval imaging
- Cystic change
- Hyperintensity and heterogeneous enhancement on T1 weighted images
MANAGEMENT
Managing NF1-related PNFs remains challenging; however, selumetinib, the MEK inhibitor, is the first FDA-approved medication for children with symptomatic and inoperable PNFs.
Active treatment is critical in patients with symptoms or progressive tumor growth. Surgery remains the standard treatment for managing PNFs and Malignant peripheral nerve sheath tumors ( MPNSTs); however, it has often demonstrated insufficient results because of its wide distribution and the frequent involvement of major organs.
REFERENCES
Growing nervous about losing eyesight: orbital manifestations of neurofibromatosis type 1
M. T. H. Nguyen et al
DOI-Link: https://dx.doi.org/10.1594/ecr2017/C-0885
Radiological insights into orbital and periorbital plexiform neurofibromas in children with neurofibromatosis type 1
Hind Qajia MD et al.
https://doi.org/10.1016/j.radcr.2025.10.027
Clinical Images: Imaging Manifestations of Orbital Neurofibromatosis Type 1
James M Milburn et al
https://pmc.ncbi.nlm.nih.gov/articles/PMC5158145/
Treatment of Plexiform Neurofibromas : Current Perspectives on Surgery and Medical Treatment
Jun Kyu Hwang et al
https://pmc.ncbi.nlm.nih.gov/articles/PMC12062538/
Dr. RAHUL KARTHIK LINGUTLA
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. NIKITHA U N
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.