Walk in OPD patient with History of on and off mild breathlessness and fever since 6 months.
Clinical Data:
Walk in OPD patient with History of on and off mild breathlessness and fever since 6 months. No history of tuberculosis or ICU admission.
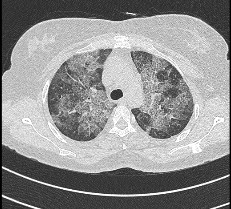
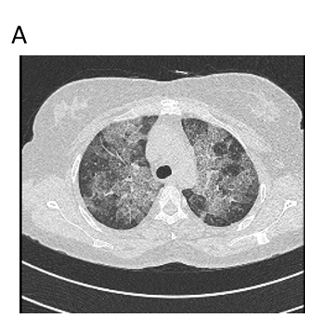
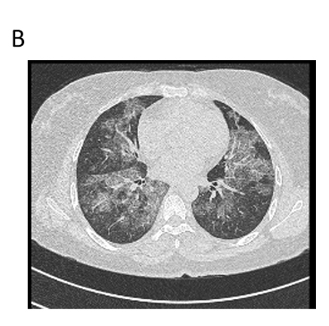
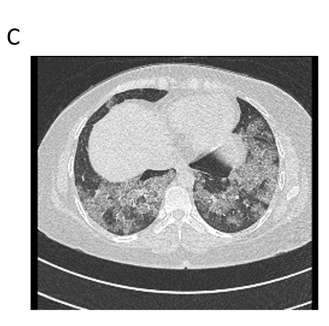
Axial lung window thorax CT of upper (A), middle (B) and lower lobe (C) of lung with zoomed in image (D) showing diffuse areas of ground-glass opacities (blue arrow) with superimposed interlobular and intralobular septal thickening (orange arrow) suggestive of crazy paving pattern in both lungs predominantly involving perihilar and peribronchovascular distribution.
Pulmonary alveolar proteinosis ( PAP).
Imaging differentials include ARDS, atypical infection
Introduction:
- Pulmonary alveolar proteinosis (PAP) is a rare disease characterized by abnormal intra alveolar accumulation of surfactant-like material
- Clinical presentation is usually with non-specific respiratory symptoms such as dyspnea or a minimally-productive cough. Approximately one-third of patients may be asymptomatic (1).
- In children, the presentation is often less clearly respiratory in nature, with diarrhea, vomiting, failure to thrive and even cyanosis being more common.Pulmonary alveolar proteinosis may be divided into three broad categories:idiopathic, secondary, and congenital.
- Idiopathic PAP (also termed “acquired” or “adult-type” PAP) accounts for the great majority of cases (90%).
- Secondary PAP (5%–10% of cases) is recognized in patients with industrial inhalational exposure to materials such as silica particles, cement dust, aluminum dust, titanium dioxide, nitrogen dioxide, and fiberglass; underlying hematologic malignancy; or immunodeficiency disorders (including cytotoxic or immunosuppressive therapy and human immunodeficiency virus infection).
- Congenital PAP is quite rare (2% of cases) and manifests in the neonatal period with severe hypoxia. “Congenital PAP” is not universally regarded as a true form of PAP, but may instead represent the disease entity termed “chronic pneumonitis of infancy”
Imaging
Chest radiograph:
- The typical radiograph reveals bilateral central and symmetric lung opacities, with relative sparing of the apices and costophrenic angles
- Opacities range from a ground glass appearance with indistinct margins, to reticular or reticulonodular, to consolidation with air bronchograms
Computer tomography:
- The CT appearance of “crazy-paving,” is seen, which is defined as a network of smoothly thickened reticular (septal) lines superimposed on areas of ground-glass opacity.
- Areas of crazy-paving in PAP are typically widespread and bilateral, often with sharply marginated areas.
- Few patterns of parenchymal sparing, including geographic, costophrenic angle, supradiaphragmatic, subpleural, and perifissural sparing seen.
- Extent and degree of CT ground-glass opacity or consolidation appear to correlate directly with severity of compromised pulmonary functional parameters (2)
Complications:
- Superimposed infectious pneumonia affects approximately 13% of all PAP patients. The increased risk of developing pneumonia in PAP may be due to macrophage dysfunction or the microbial growth medium provided by intraalveolar proteinaceous material.
- Complicating infectious pneumonias in PAP are often opportunistic
Imaging differential:
- Although the CT finding of crazy-paving is highly characteristic of PAP, it is also seen in several other conditions.
- Therefore, the radiologic differential diagnosis of crazy-paving is broad and includes left heart failure, pneumonia (especially pneumocystis pneumonia), alveolar hemorrhage, bronchoalveolar carcinoma, lymphangitic carcinomatosis, diffuse alveolar damage (adult respiratory distress syndrome), radiation- or drug-induced pneumonitis, hypersensitivity pneumonitis, and pulmonary veno-occlusive disease (3)
Reference:
1. Katzenstein ALA. Katzenstein and Askin’s surgical pathology of non-neoplastic lung disease. 4th ed. Philadelphia, Pa: Saunders Elsevier, 2006.
2. Rosen SH, Castleman B, Liebow AA. Pulmonary alveolar proteinosis. N Engl J Med 1958;258: 1123–1142.
3. Ioachimescu OC, Kavuru MS. Pulmonary alveolar proteinosis. Chron Respir Dis 2006;3:149–159.
Dr Deepti H V
DMRD, DNB, EDiR,
Senior Consultant Manipal Hospitals Radiology Group.
Dr Sanjana.N
MDRD,Cross section imaging fellow - MHRG