5 days old infant presented with history of seizure. History of prolonged difficult delivery present.
Clinical Features:
5 days old infant presented with history of seizure. History of prolonged difficult delivery present.
LEGENDS
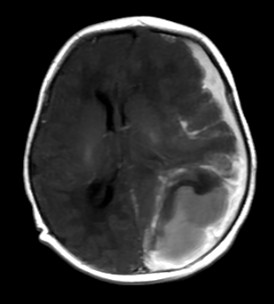
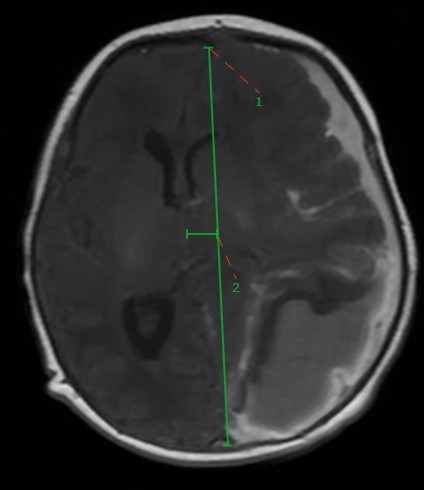
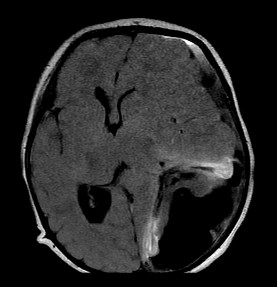
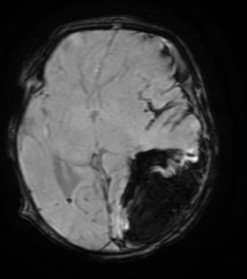
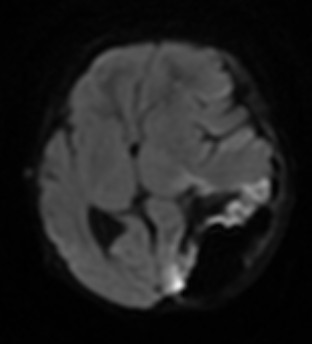
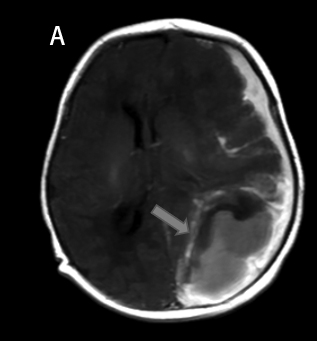
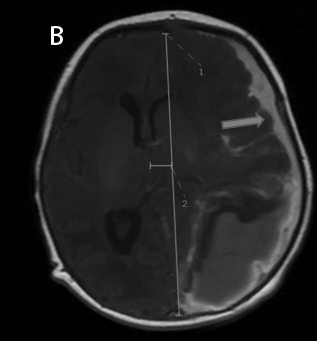
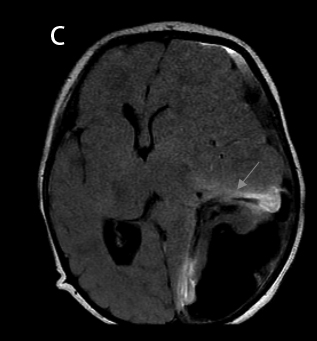
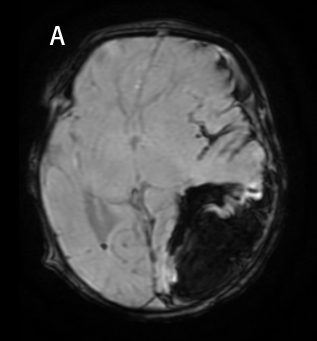
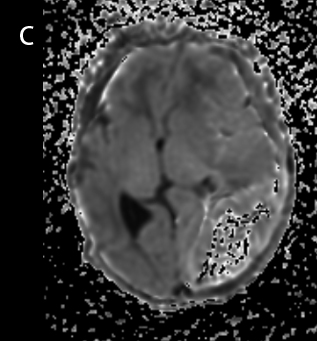
- Acute haematoma in the left parieto occipital convexity (Blue arrow). Haematoma appears mildly hyperintense on T1 (Fig A) and hypointense on FLAIR (Fig C). FLAIR hyperintense oedema in the surrounding parenchyma (Fig C).
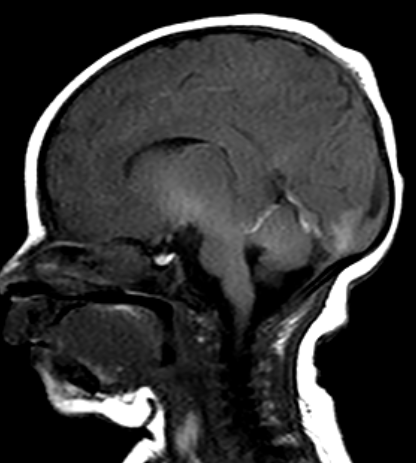
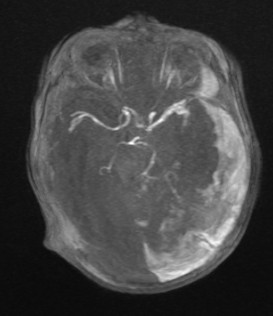
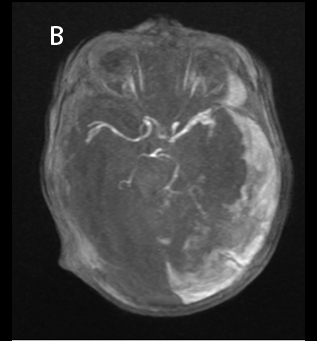
- The underlying parenchyma is markedly compressed and reduced in volume (Orange arrow). Mid line shift towards right (Fig B). The body and occipital horn of the left lateral ventricle are compressed. Acute subdural haematoma in the left cerebral convexity (Blue arrow, Fig B)
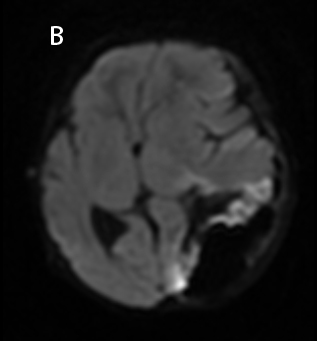
- Internal blooming within the hematoma seen suggestive of haemorrhage. Areas of cortical restricted diffusion seen – Suggestive of hemorrhagic infarct in underlying parenchyma
- Craniovertebral junction appears normal (Fig A) and no abnormality detected in circle of willis (Fig B)
DIAGNOSIS
- Acute haematoma in the left parieto occipital convexity, Underlying parenchyma is markedly compressed and reduced in volume with surrounding edema.
- Features suggestive of subpial hemorrhage with hemorrhagic infarct in underlying parenchyma.
DISCUSSION
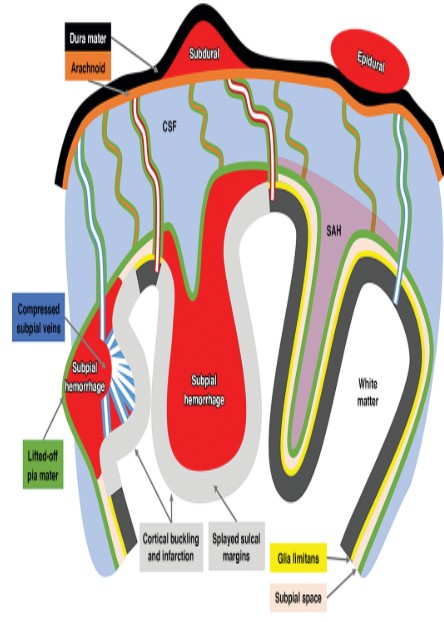
Anatomy of the Subpial Space
The subpial space (SpS) can be defined as the potential space bordered externally by the pia mater and internally by the glia limitans (i.e., the outermost layer of astrocyte foot processes in the neocortex [layer 1]) [1].
Proposed risk factors associated with leptomeningeal hemorrhages include neonatal asphyxia, birth injuries, fetal head molding, clotting disorders, venous sinus compression, variations in intracranial pressure, and incomplete regression of the primary vascular network
Subpial Hemorrhage
In the strict sense, it is a primary intracortical hemorrhage which is so superficial that it easily extends outside the cerebral gray matter and is contained under the pia mater.
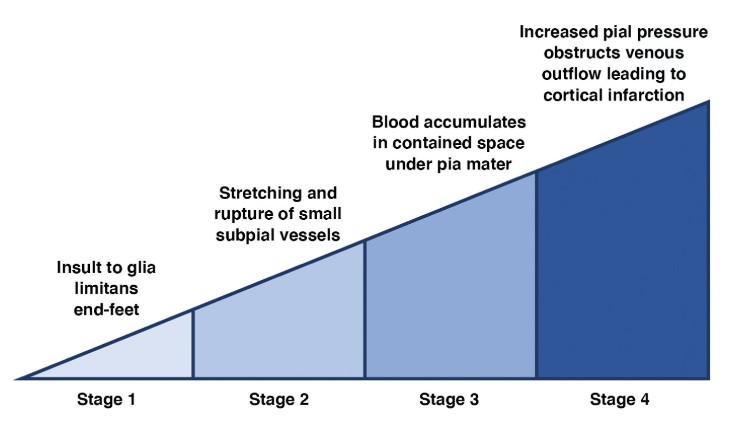
Specifically, subpial veins are more susceptible to this local pressure increase because, compared with their arterial counterparts. Therefore, subpial hemorrhage causes local venous congestion and hypertension due to blockage of cortical venous outflow, which is normally directed toward the SpS (2).
The result is focal cortical or subcortical infarction characteristic of subpial hemorrhage
IMAGING
- Head sonography is very useful in depicting the periphery of the brain, where most subpial hemorrhages occur. Although some head sonography findings raise suspicion of subpial hemorrhage, they may not allow definitive diagnosis of subpial hemorrhage.
- MRI provides the most precise anatomic detail, and combinations of sequences enable evaluation of the full spectrum of injury in subpial hemorrhage. Because it cannot easily diffuse through the collagen-rich SpS, blood collects in a contained localized hematoma between the lifted-off pial lining and the subjacent cortex on either side. The resulting mass effect explains the unique imaging feature of cortical inward depression (cortical buckling) and patchy cortical and subcortical injury.
- Depending on the extent of the hemorrhage, global mass effect, and associated lesions, it is possible to have accompanying deep white matter damage that is venous ischemic or hemorrhagic in nature (3).
Imaging Differential
- Differentiation of locations of leptomeningeal hemorrhage is important because of the distinct pathophysiology and clinical sequelae.
- Subpial hemorrhage sits underneath an impermeable pia mater, which is otherwise closely adherent to the circumjacent glia limitans, preventing prompt resorption of blood and invariably causing some degree of cortical damage, analogous to what happens in compartment syndrome.
- Conversely, subarachnoid hemorrhage can diffuse through the CSF and eventually be absorbed, preventing direct mass effect on the cortex but presenting other potential risks, such as hydrocephalus.
Reference
- Glaser J. The cerebrospinal fluid of premature infants: with special reference to intracranial hemorrhage and pigmentation. Am J Dis Child 1928; 36:195–247
- Gunda D, Cornwell BO, Dahmoush HM, Jazbeh S, Alleman AM. Pediatric central nervous system imaging of nonaccidental trauma: beyond subdural hematomas. RadioGraphics 2019; 39:213–228
- Huang AH, Robertson RL. Spontaneous superficial parenchymal and leptomeningeal hemorrhage in term neonates. AJNR 2004; 25:469–475
Dr HARSHA C CHADAGA
Senior Consultant Manipal Hospitals Radiology Group.
Dr Sanjana.N
Cross section imaging fellow - MHRG