A 27 year old gentleman presented with few episodes of hemoptysis. He also had a history of cough with expectoration since few months.
CLINICAL DETAILS
- A 27 year old gentleman presented with few episodes of hemoptysis. He also had a history of cough with expectoration since few months.
- On examination he was hypoxic, had bilateral crepitations on auscultation along with grade III clubbing of digits.
- CT Aortogram was suggested.
IMAGING:
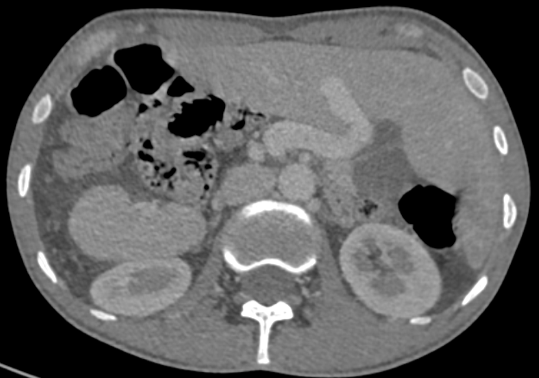
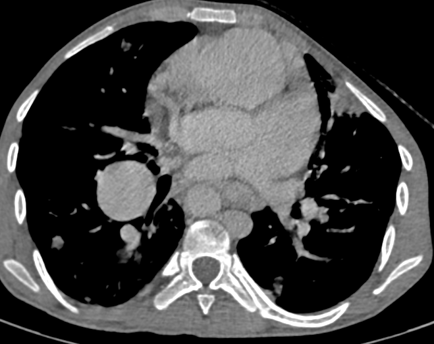
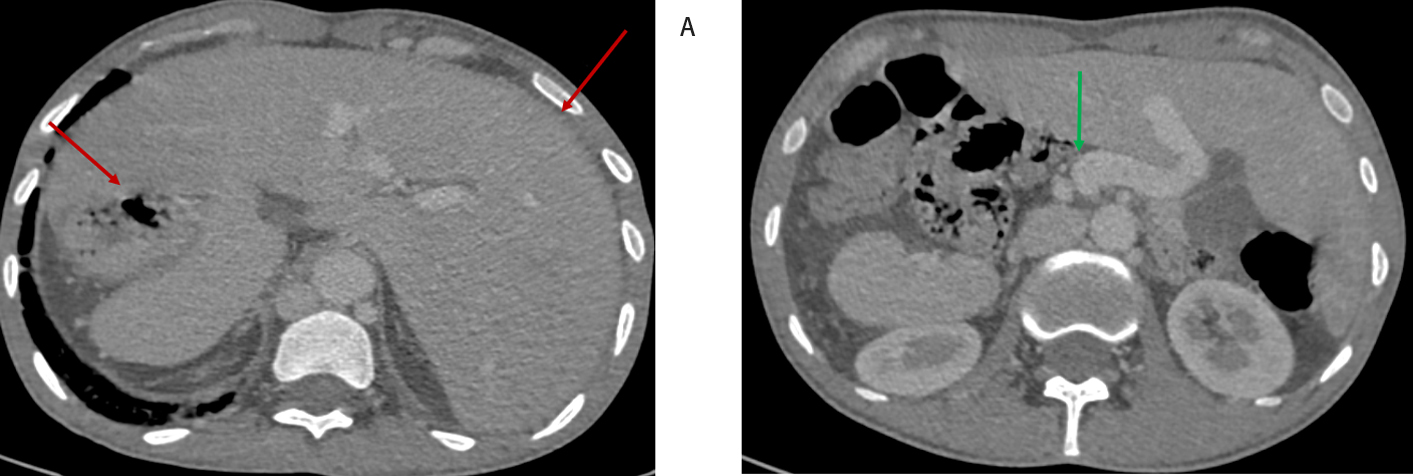
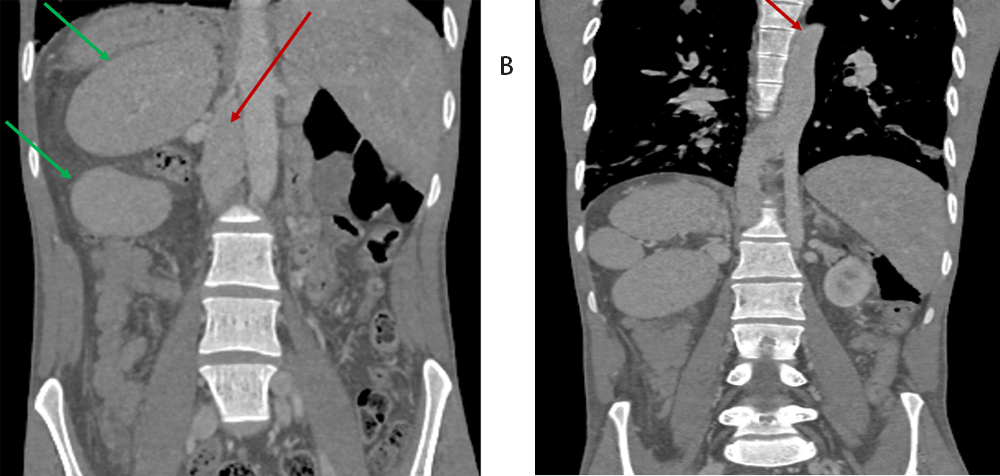
- Axial contrast enhanced CT at the level of upper abdomen.
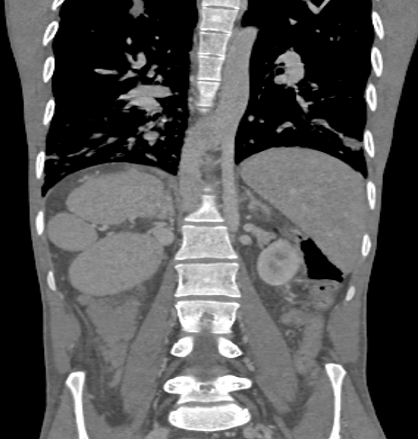
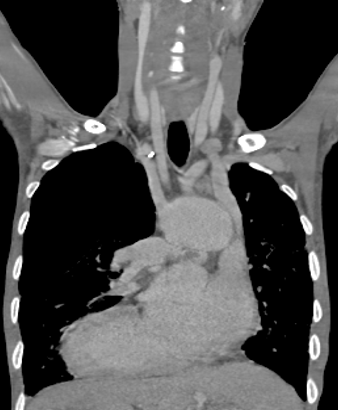
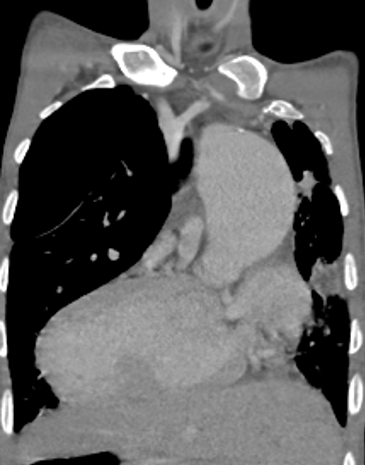
- Coronal contrast enhanced CT showing aorta and IVC
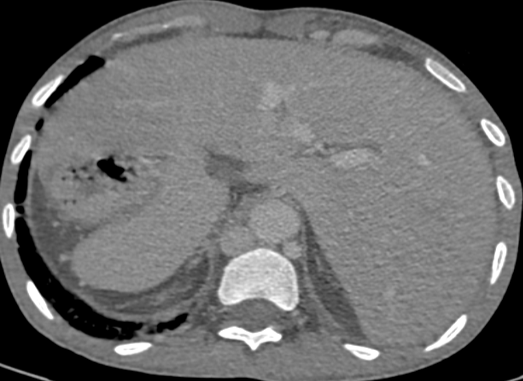
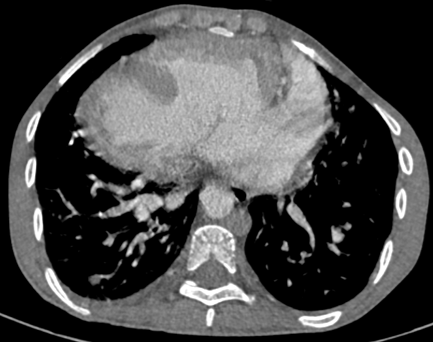
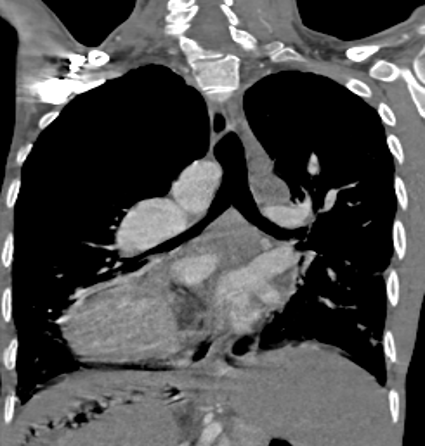
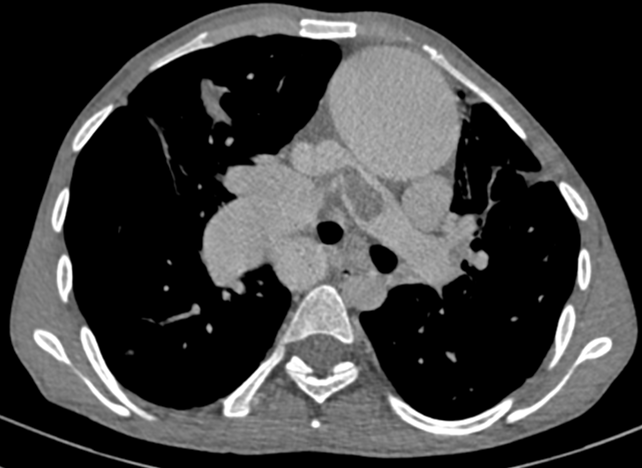
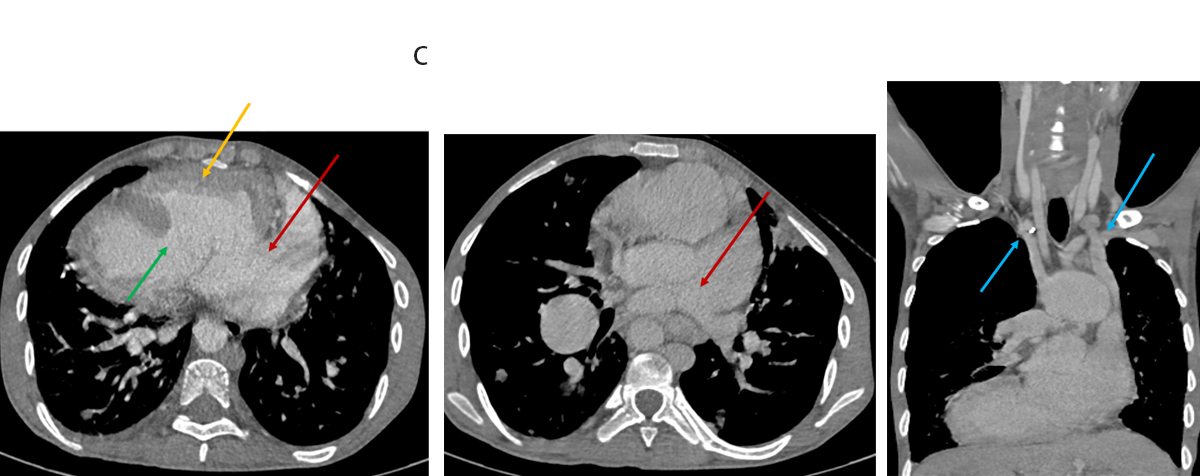
- Axial and coronal contrast enhanced CT at level of the heart.
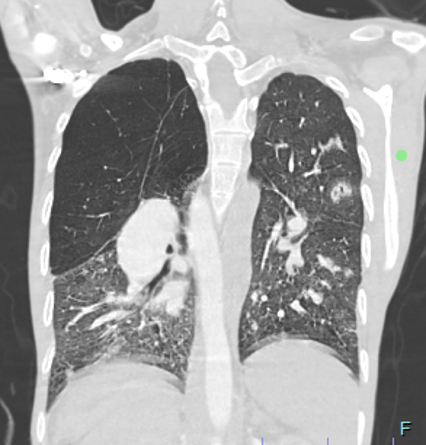
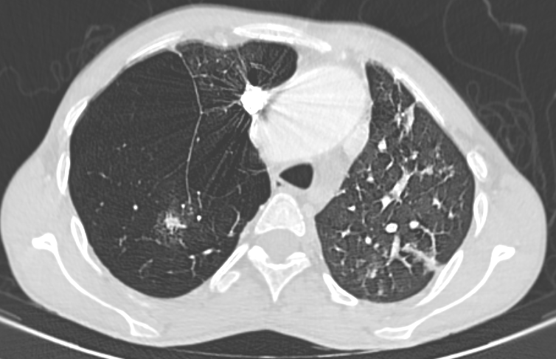
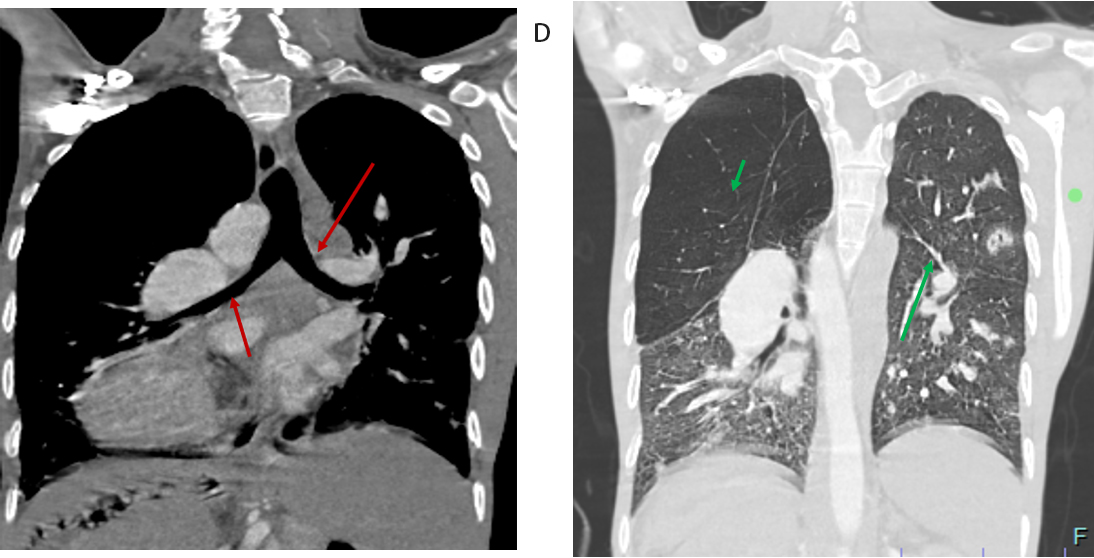
- Coronal contrast enhanced CT chest with lung window.
- Coronal and axial contrast enhanced CT chest at the level of aorta and pulmonary artery.
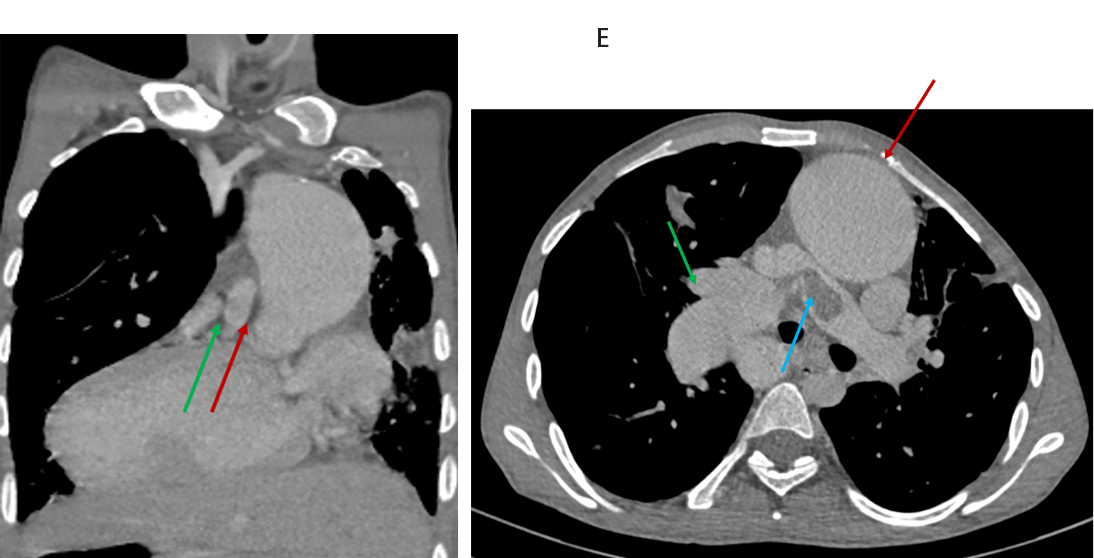
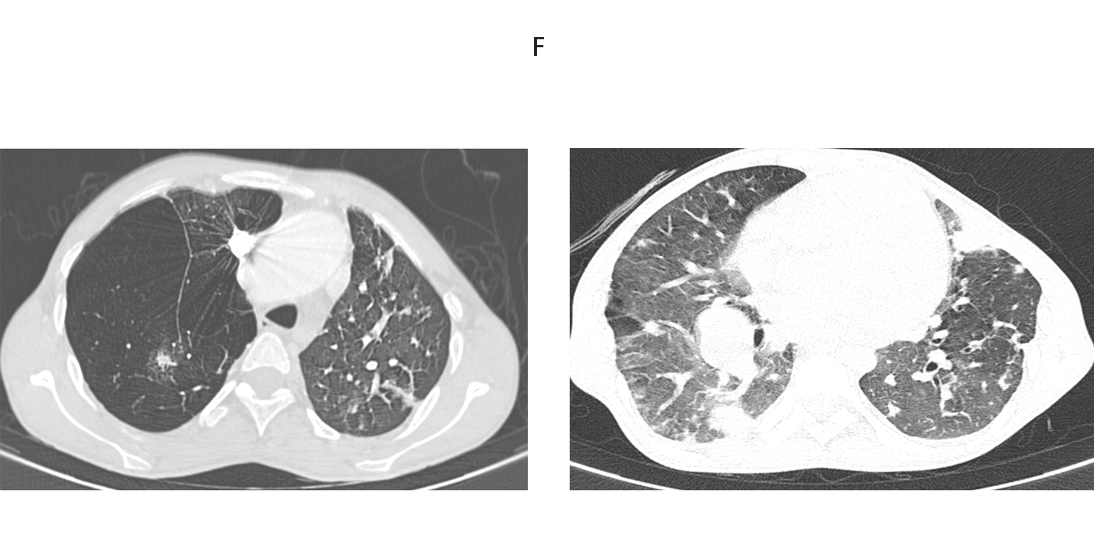
- Axial CT chest lung window.
- Situs abnormality: Left-sided liver, right-sided stomach (red); SMV left of SMA → Malrotation (green).
- Venous anomalies: Interrupted intrahepatic IVC with hemiazygous continuation (red); Double SVC draining into RA (blue).
- Cardiac findings: Dextrocardia, single atrial chamber receiving pulmonary veins (red); large VSD (green); morphological LV on left (yellow).
- Pulmonary features: Bilateral hyparterial bronchi, bilobed lungs (green); enlarged RPA compressing right main bronchus with RUL emphysema.
- Vascular anomalies: Dilated aortic root left of pulmonary artery (red); pulmonary valve atresia with atretic main PA; confluent RPA and LPA (green).
- Acute findings: Saddle embolus at PA bifurcation (red); dilated right PA (blue).
- Parenchymal findings: Multifocal broncho-vascular nodules + GGOs.
- Infarcts: Wedge-shaped opacities in left lingula and right lower lobe → likely pulmonary infarcts.
- Other signs: Smooth interlobular septal thickening; mosaic attenuation in lower lobes.
A. Left-sided liver and right-sided stomach (red arrows) with polysplenia – consistent with situs ambiguous. SMV located to the left of SMA (green arrow) – suggestive of intestinal malrotation.
B. Interrupted intrahepatic IVC with hemiazygous continuation (red arrows). Multiple right-sided spleens suggestive of polysplenia syndrome (green arrows).
C. Dextrocardia with common single atrial chamber (red arrows).Double SVC draining into right atrium (blue arrows).Large VSD (green arrow); morphological LV on the left (yellow arrow).
D. Bilateral hyparterial bronchi (red arrows); bilobed lungs (Short green arrow).Enlarged right pulmonary artery compressing right main bronchus.Emphysematous changes in the right upper lobe (green arrows).
E. Dilated aortic root left of pulmonary artery (red arrows).Pulmonary valve atresia with atretic main pulmonary artery; confluent RPA & LPA (green arrows).Saddle thrombus at pulmonary bifurcation (red arrow).Dilated right pulmonary artery (blue arrow).
F. Multifocal broncho-vascular consolidation and nodules with surrounding ground-glass opacities.Peripheral wedge-shaped opacities in left lingula and right posterior basal segment — suggestive of pulmonary infarcts.Smooth interlobular septal thickening and mosaic attenuation in bilateral lower lobes.
Cardiac and Vascular Anomalies:
- Dextrocardia with large ASD (common atrium) and large VSD.
- Pulmonary valve atresia with atretic main pulmonary artery and confluent branch PAs.
- Dilated aortic root left of the pulmonary artery.
- Double SVC and interrupted IVC with hemiazygous continuation.
Pulmonary Findings:
- Saddle pulmonary embolism with dilated right PA compressing the right upper lobe bronchus → emphysematous changes.
- Bilateral hyparterial bronchi, bilobed lungs (left isomerism).
- Pulmonary infarcts (lingular and right lower lobe).
- Multifocal consolidation, ground-glass opacities, centrilobular nodules – likely infection.
- Septal thickening and mosaic attenuation – suggestive of perfusion/air trapping abnormalities.
Abdominal and Situs Anomalies:
- Left-sided liver, right-sided stomach, polysplenia, and intestinal malrotation.
HETEROTAXY SYNDROME (LEFT ISOMERISM) WITH COMPLEX CONGENITAL CARDIAC ANOMALIES, ASSOCIATED PULMONARY AND VASCULAR COMPLICATIONS, AND SECONDARY INFECTIVE AND PERFUSION-RELATED PULMONARY CHANGES.
Introduction:
Situs solitus:
- Normal anatomical positioning of thoracic and abdominal organs (liver on the right, stomach on the left).
Situs inversus:
- Mirror-image reversal of situs solitus; usually asymptomatic and discovered incidentally.
Situs ambiguous (Heterotaxy):
- Abnormal, inconsistent arrangement of visceral organs with indeterminate atrial situs.
Heterotaxy Syndrome:
- A spectrum of congenital anomalies due to abnormal embryological lateralization, leading to disruption of normal left-right asymmetry in thoraco-abdominal organs.
Two distinct patterns of isomerism are recognized in heterotaxy syndromes:
Right isomerism
- Characterized by bilateral right atrial appendages
- Commonly associated with absence of the spleen (Asplenia syndrome)
- Often presents with more severe and complex cardiac anomalies
Left isomerism
- Characterized by bilateral left atrial appendages
- Associated with presence of multiple, often malformed, spleens (Polysplenia syndrome)
Although there is overlap in cardiac abnormalities, certain features help distinguish the two patterns.
Both types are frequently associated with extracardiac anomalies involving the lungs, bronchi, liver, spleen, gastrointestinal tract, and systemic venous system.
Left Atrial Isomerism (Polysplenia Syndrome)
- Defined by bilateral symmetry of paired structures, resembling left-sided morphology
- Common features:
- Bilobed lungs with hyparterial bronchi
- Multiple spleens (polysplenia)
Associated Cardiac Anomalies
1. Cardiac position abnormal in 40–50%
2. Bilateral left atrial appendages
3. Systemic venous anomalies:
- Bilateral SVC (~66%), one may drain into coronary sinus
- IVC interruption with azygous/hemiazygous continuation (~80%)
- Hepatic veins may drain into either or both atria.
4. Anomalous pulmonary venous return
5. Interatrial septum: AV septal defects common; rarely intact septum
6. Atrioventricular connection: Biventricular but often ambiguous (75%)
7. Ventriculo-arterial connection: Discordant or DORV in 20–30%
8. Outflow tracts:
- Unobstructed pulmonary flow common
- Pulmonary stenosis (50%), atresia (<10%)
- Subaortic obstruction (~22%)
9. Conduction system abnormalities
Pulmonary Atresia and Diagnostic Evaluation
- Pulmonary Atresia without PDA or MAPCAs on non-gated CT.
- However, bronchial and intercostal collaterals were identified, likely serving as the source of pulmonary perfusion.
- These systemic collaterals are also a probable cause of hemoptysis, due to high-pressure systemic blood flow entering fragile pulmonary circulation.
- Patient underwent bronchial artery embolization, with good symptomatic response.
- Patient remains stable, underscoring the role of targeted endovascular therapy in palliative management of complex congenital cases.
Further Management
- Gated CT Angiography – detailed anatomical assessment
- Cardiac Catheterization – evaluate collateral supply, pressures, surgical feasibility
- Cardiac MRI – assess ventricular function and flow dynamics
- Multidisciplinary Team (MDT) planning to decide between:
- Unifocalization with RV-PA conduit
- or Single-ventricle palliation (Glenn/Fontan)
- Close follow-up – monitor hemoptysis recurrence or complications
- Genetic counselling – due to heterotaxy syndrome
Basic steps in sequential segmental approach to congenital heart diseases.Segmental Approach - Steps
- Step 1: Determine situs (abdominal, bronchopulmonary, atrial) & heart position.
- Step 2: Identify cardiac chambers and arterial trunks by morphological criteria.
- Step 3: Assess relationships within each segment:
- 3-1: Atrial relationship (atrial situs) → Already known from Step 1.
- 3-2: Ventricular relationship → Check ventricular loop pattern (D-loop, L-loop, etc.).
- 3-3: Arterial relationship → Position of aortic root relative to pulmonary trunk.
- Step 4: Assess intersegmental connections:
- 4-1: Systemic and pulmonary venous connections to atria.
- 4-2: Atrioventricular connections.
- 4-3: Ventriculoarterial connections.
- Step 5: Look for associated abnormalities at each segmental level.
- Heterotaxy syndrome represents a complex spectrum of thoracoabdominal laterality defects with highly variable cardiac and extracardiac manifestations.
- Due to the near-infinite combinations of anomalies, a segmental and individualized diagnostic approach is essential.
- Left atrial isomerism (polysplenia) in adults often presents late and is typically managed with palliative, symptom-directed care, depending on functional status and defect severity.
- Gated cardiac CT plays a critical role in:
- Defining vascular anatomy and pulmonary arterial supply
- Identifying intracardiac anomalies and systemic-pulmonary collaterals
- Planning surgical or endovascular interventions
- Multidisciplinary team (MDT) evaluation is vital to tailor appropriate long-term care, balancing intervention risks with quality of life.
REFERNCES
- Yoo SJ, Perens G, Nguyen KL, Yoshida T, Saprungruang A, Van Arsdell GS, Finn JP. Contemporary sequential segmental approach to congenital heart disease using four-dimensional magnetic resonance imaging with ferumoxytol: an illustrated editorial. Front Cardiovasc Med. 2023 Jul 4;10:1107399.
- Lapierre C, Déry J, Guérin R, Viremouneix L, Dubois J, Garel L. Segmental approach to imaging of congenital heart disease. Radiographics. 2010 Mar;30(2):397-411. doi: 10.1148/rg.302095112.
- Agarwal R, Varghese R, Jesudian V, Moses J. The heterotaxy syndrome: associated congenital heart defects and management. Indian J Thorac Cardiovasc Surg. 2021 Jan;37(Suppl 1):67-81. doi: 10.1007/s12055-020-00935-y. Epub 2020 Mar 27.
Dr. Faizel A
Consultant Radiologist,
Manipal Hospitals, Varthur Road.
Dr Kanupriya Grover
Cross Section Imaging Fellow,
Manipal Hospital, Yeshwanthpur.