62 years old with solitary pulmonary lesion
- 62 years old, bleeding per rectum for 4 months
- Diagnosed carcinoma of rectum with lung and nodal metastasis
- Underwent right thoracotomy, metastasectomy and lymphadenectomy for lung and nodal metastasis
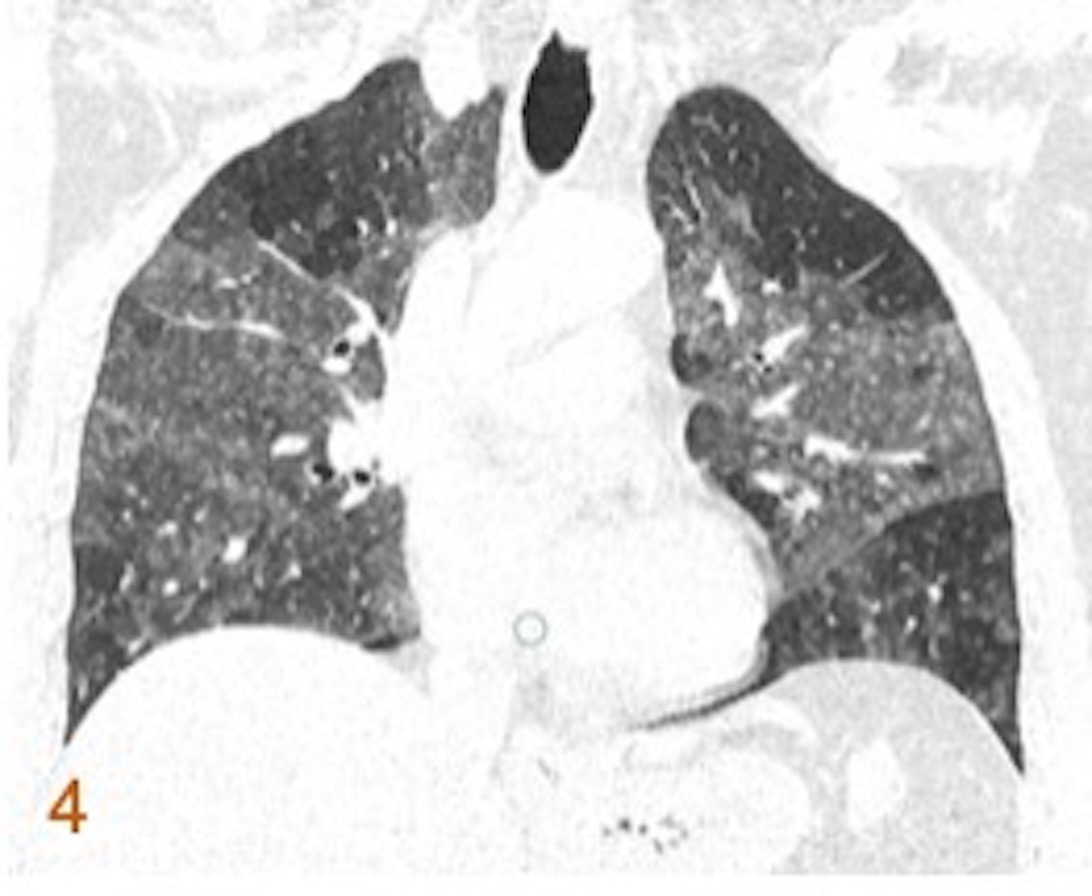
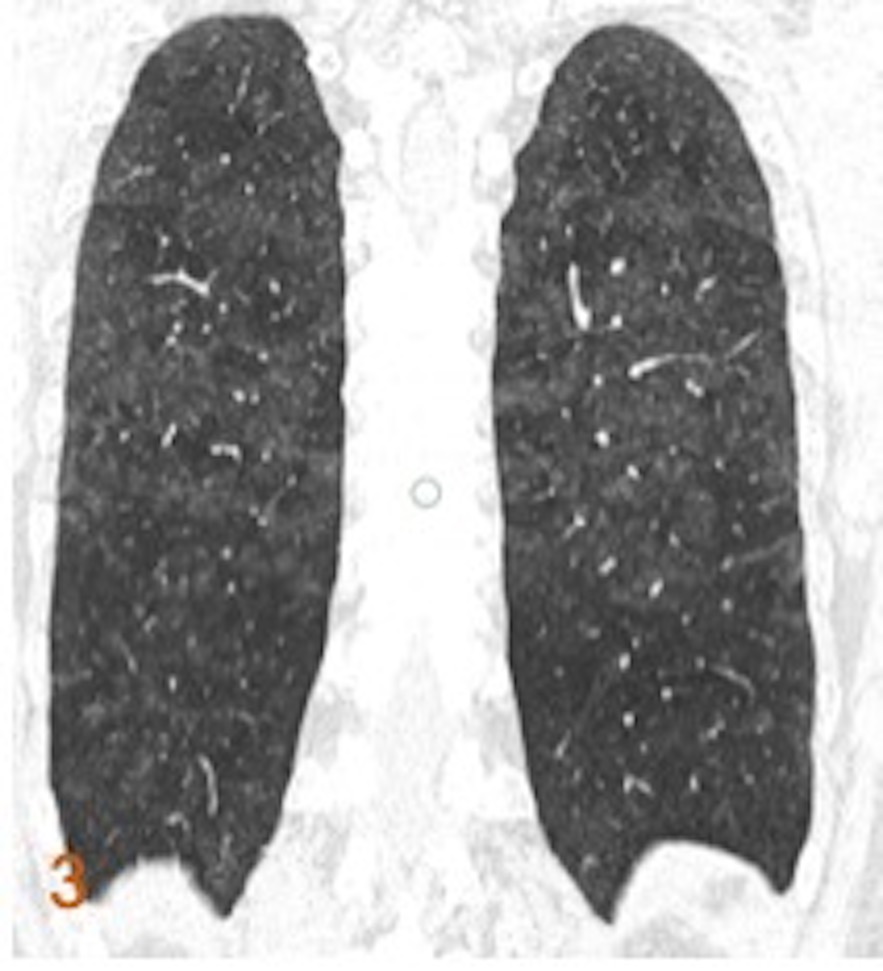
- 20 month after the surgery, developed a solitary right lung lesion adjacent to previous surgical site
- Figure 1 (a, b): sagittal and axial images of the chest CT obtained 20 months after metastasectomy demonstrates a new oval soft tissue lesion with spiculated margins adjacent to the post-surgical changes.
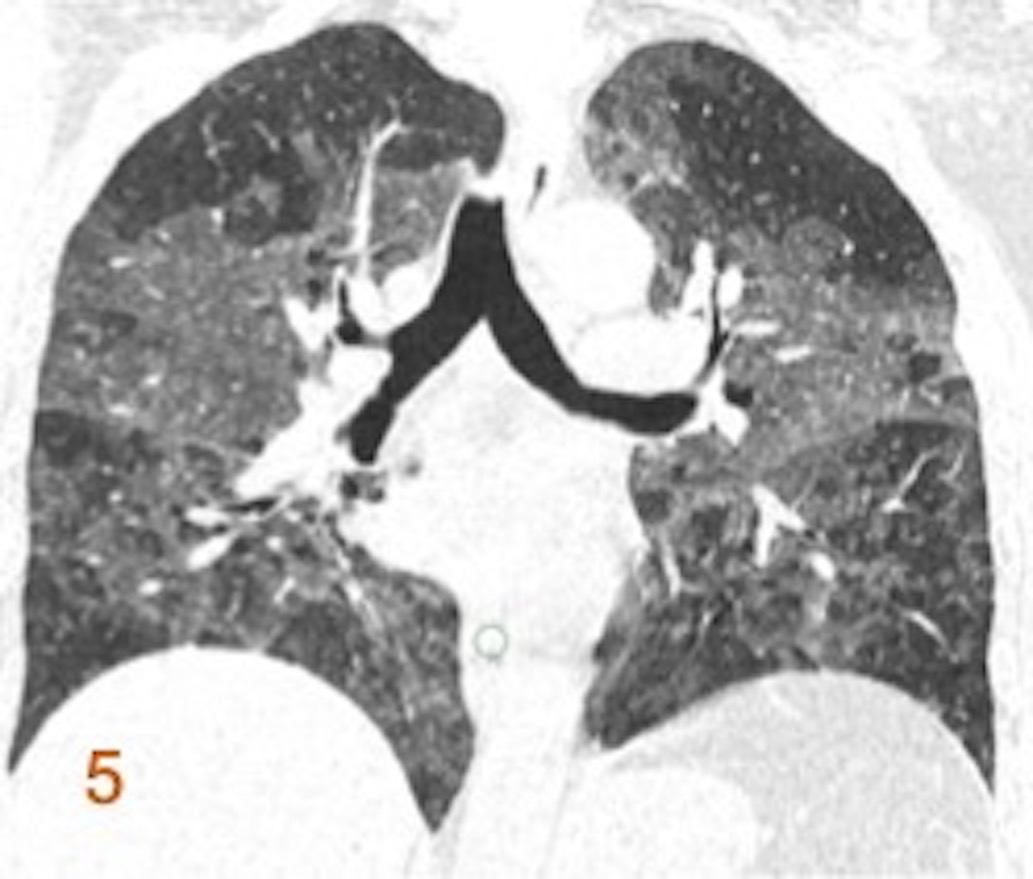
- Figure 2 (a): Pre-ablation planning CT
- Figure 2 (b): Intra-procedural CT demonstrating RFA electrode within the lesion
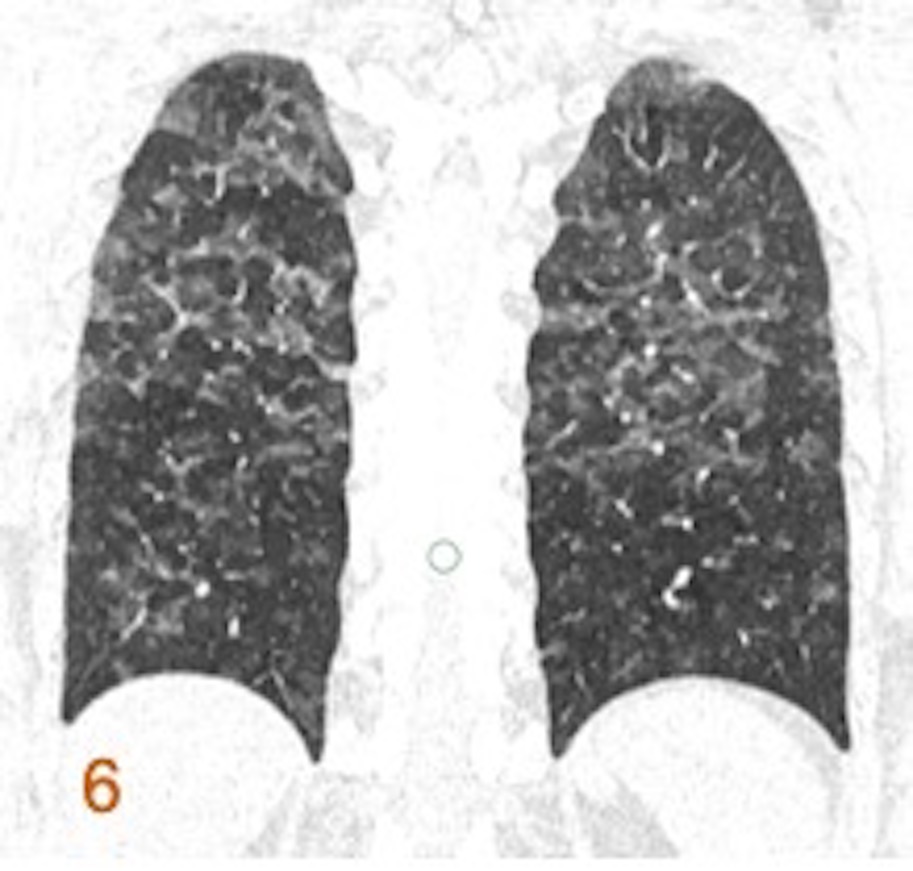
- Figure 3: Axial CT image immediately after ablation shows cavitation of the lesion with perilesional ground-glass opacification.
Diagnosis:
Radiofrequency ablation of lung metastasis
Discussion:
Treatment options for lung metastasis
- Surgical resection
- Laser-Induced Thermotherapy
- Radiofrequency Ablation
- Microwave Ablation
- Radiofrequency ablation offers a similar median survival range as of surgical metastasectomy
- Advantages of thermal ablation
- Minimal effect on pulmonary function/quality of life
- Can be repeated
- Short hospital stay
- Does not require interruption of chemotherapy
Mechanism of action:
- Thermal energy damage to cellular proteins, enzymes, & nucleic acids creates tissue necrosis and coagulation
- RFA is indicated in small (<3 cm) solitary lung lesions located peripherally.
- The lesion should not be contiguous with major vessels as it can lead to heat sink effect.
- Relative contraindications for the procedure include underlying interstitial disease, coagulopathies and immediate proximity to sensitive structures such as central airways, major vascular structures or esophagus.
- Rarely, the procedure is complicated by bronchopleural fistula, tumor seeding, neural or diaphragmatic injury.
Complications:
- Most frequent complications include
- Pleuritis
- Pneumonia
- Abscess
- Hemorrhage
- Refractory pneumothorax requiring pleurodesis
- Major complications are rare and include
- Bronchopleural fistula
- Tumor seeding
- Nerve or diaphragmatic injury.
References:
- Vogl TJ, Eckert R, Naguib NN, Beeres M, Gruber-Rouh T, Nour-Eldin NE. Thermal ablation of colorectal lung metastases: retrospective comparison among laser-induced thermotherapy, radiofrequency ablation, and microwave ablation. American Journal of Roentgenology. 2016 Dec;207(6):1340-9.
- Ridge CA, Solomon SB. Percutaneous ablation of colorectal lung metastases. Journal of gastrointestinal oncology. 2015 Dec;6(6):685.
- Bhatia S, Pereira K, Mohan P, Narayanan G, Wangpaichitr M, Savaraj N. Radiofrequency ablation in primary non-small cell lung cancer: What a radiologist needs to know. The Indian Journal of Radiology & Imaging. 2016 Jan;26(1):81.
Dr Rajesh Helavar
MD, PDCC
Consultant Interventional Radiology
Columbia Asia Radiology Group
Dr Renu Jadiya
DNB Resident
Columbia Asia Radiology Group