Presented with complaints of fever since 2 days. Headache and vomiting since 1 day. Noticed right eye swelling since 1 day morning which suddenly increased in size over the course of the day.
HISTORY AND CLINICAL EXAMINATION
- Presented with complaints of fever since 2 days.
- Headache and vomiting since 1 day.
- Noticed right eye swelling since 1 day morning which suddenly increased in size over the course of the day.
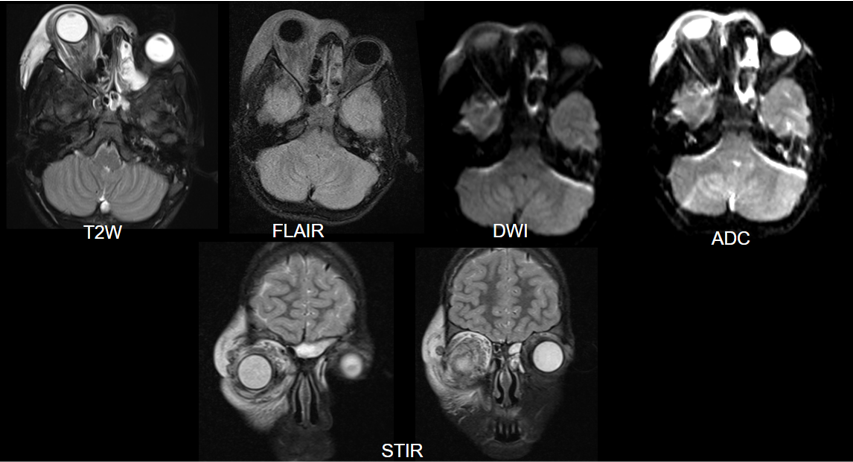
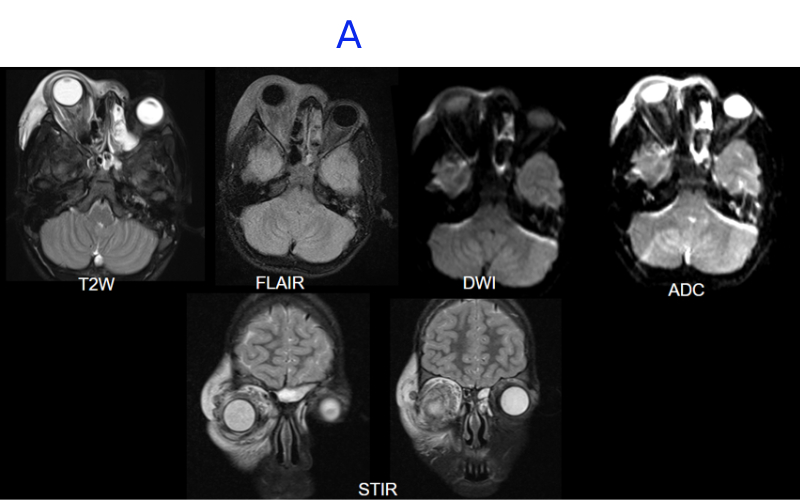
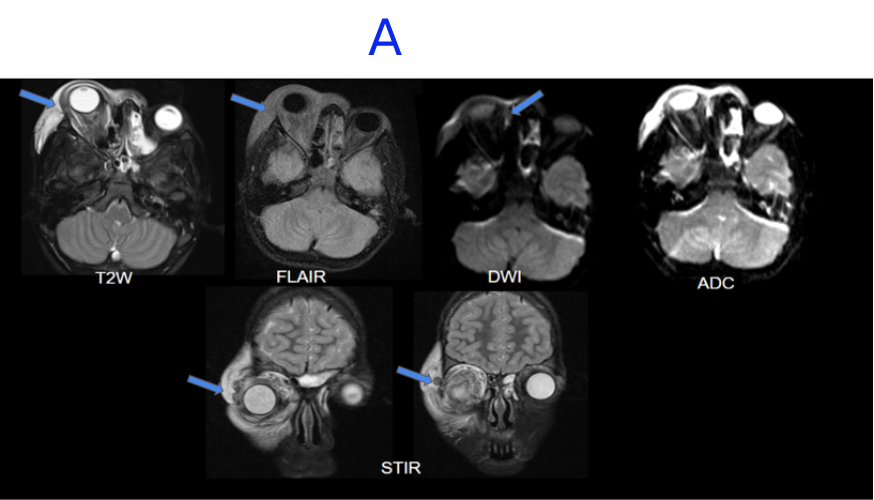
A. FINDINGS – MRI BRAIN WITHOUT IV CONTRAST - DAY 1
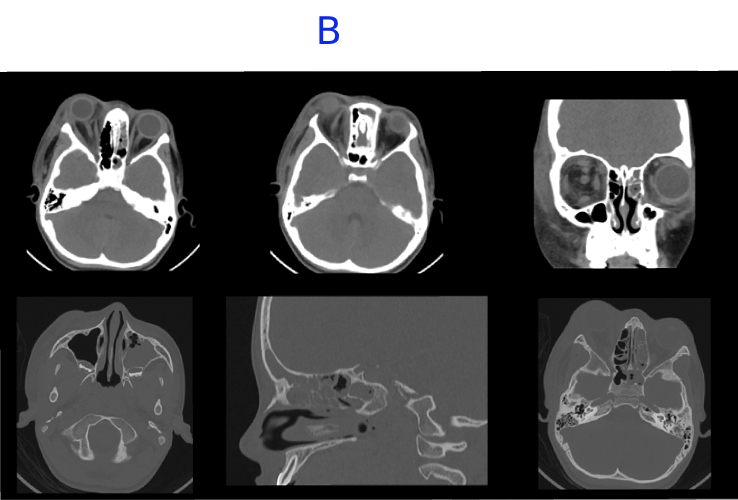
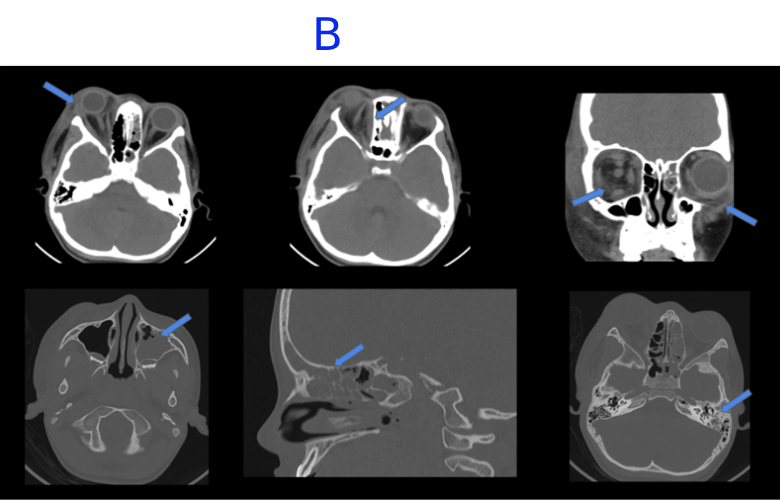
B. FINDINGS – CT PNS WITHOUT IV CONTRAST - DAY 2
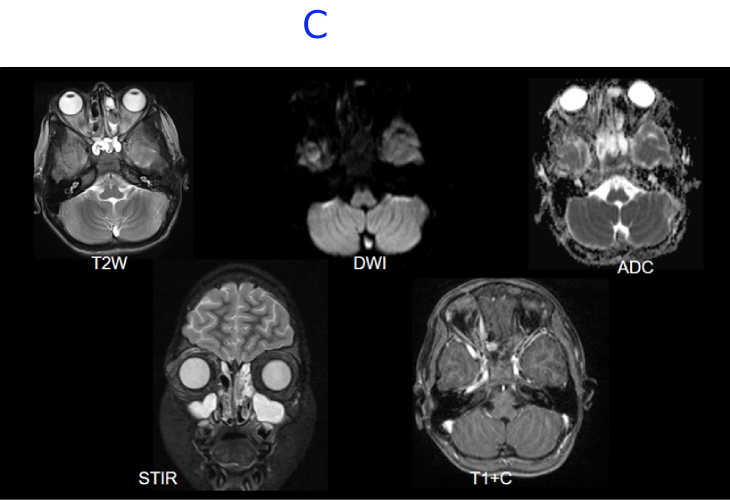
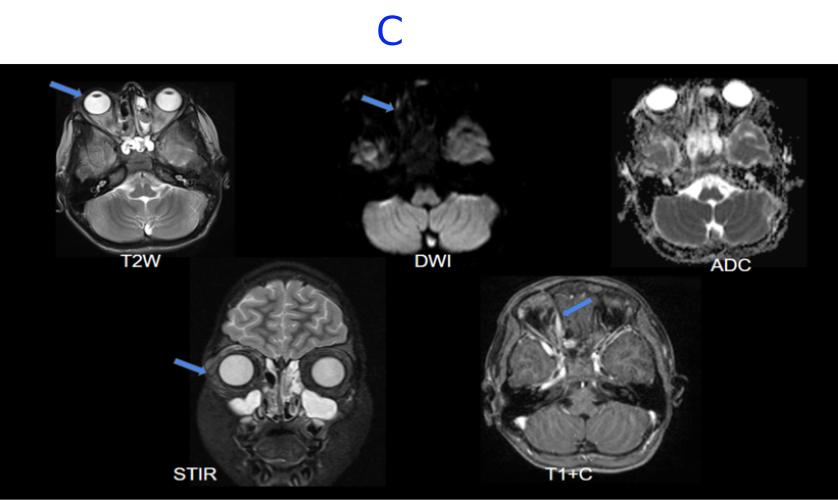
C. MRI BRAIN WITH IV CONTRAST - DAY 11- STATUS POST DECOMPRESSION
A. Right globe proptosis noted . There is extensive T2/STIR hyperintense edema noted in periorbital soft tissue and orbital compartments involving intraconal, extraconal and preseptal space. There is soft tissue stranding involving postseptal fat, surrounding the extraocular muscles and enlargement of lacrimal gland.There is a small diffusion restricting collection along medial wall of orbit. There is thrombophlebitis of an external vein along the superolateral superficial soft tissues.
B. Mild interval increase in hypodense collection along medial wall of right orbit. There is interval appearance of edema and fat stranding in periorbital soft tissue and preseptal space in the left orbit. Near complete mucosal opacification with bubbly secretions of left maxillary, ethmoid, frontal and sphenoid sinus with bubbly secretions. Mild mucosal thickening in the right ethmoid and sphenoid sinus.Opacification in left middle ear cavity and left mastoid air cells.
C. Near complete resolution of the right globe proptosis.Interval reduction in the thin enhancing collection along the medial wall of right orbit demonstrating minimal diffusion restriction.Near complete resolution of the extensive T2/STIR hyperintense edema noted in right periorbital soft tissue and orbital compartments with minimal residual edema in the preseptal space.Near complete resolution of the soft tissue stranding involving postseptal fat, surrounding the extraocular muscles.
DIAGNOSIS:-
EXTENSIVE RIGHT ORBITAL CELLULITIS WITH SUBPERIOSTEAL ABSCESS AND ORBITAL COMPARTMENT SYNDROME WITH INTERVAL APPEARANCE OF LEFT PRESEPTAL ORBITAL CELLULITIS
- Orbital cellulitis is a sight-threatening, and potentially life-threatening, condition. Therefore, urgent imaging is indicated to assess the anatomic extent of disease.
- Orbital cellulitis can be either preseptal (periorbital) or postseptal (orbital). The fibrous orbital septum normally does not allow the spread of periorbital infections into the orbit.
- The differentiation between periorbital and orbital infections is important clinically because their management is different.
- Postseptal infections have a higher rate of complications like intracranial spread, meningitis, and cavernous sinus thrombosis, which can be potentially life-threatening, they require early detection and subsequent aggressive management.
- Identification of orbital abscesses is also important because they may require surgical intervention.
- Orbital cellulitis causes diffuse, oedematous infiltration of the orbital connective tissue that is best demonstrated by the high signal intensity in T2-weighted fat-saturated sequences.
- Other findings are swelling and ill-defined margins of the extraocular muscles and exophthalmos.
- Abscesses show a well-described phenomenon of diffusion restriction, likely related to the viscosity and dense cellular packing of purulent material. This diffusion restriction manifests as a region of intense signal on diffusion-weighted imaging (DWI) and associated low intensity on apparent diffusion coefficient (ADC) images within the central, nonenhancing portion of the abscess cavity.
- Periorbital cellulitis is a preseptal process, which is limited to the soft tissues anterior to the orbital septum. It usually occurs due to the contiguous spread of infection from adjacent structures such as the teeth and face. CT and MRI demonstrate diffuse soft-tissue thickening anterior to the orbital septum.
- Paranasal sinusitis is the commonest cause of orbital cellulitis and is the underlying cause in two-thirds of all cases.
- The most common cause of orbital cellulitis in our study was found to be ethmoid sinusitis, followed by frontal sinusitis.
- The factor primarily responsible for the development of orbital cellulitis in ethmoid sinusitis is the anatomic contiguity of the two structures, thin lamina papyracea and the valveless ethmoidal veins, which allow rapid spread of infection into the orbit. Apart from being thin, the lamina papyracea has multiple tiny natural deficiencies, perforating nerve vessels.
- The periorbita is the periosteum lines the walls of the bony orbit and it serves as a barrier against the early spread of infection from the paranasal sinus into the orbit. Therefore, disease spread from the ethmoid sinus to the orbit initially leads to subperiosteal abscess formation before it spreads into the orbit.
MANAGEMENT :-
ORBITAL DECOMPRESSION WITH CONCURRENT MEDICAL MANAGEMENT WITH INTRAVENOUS ANTIBIOTICS
REFERENCES:-
- MRI of Orbital Cellulitis and Orbital Abscess: The Role of Diffusion-Weighted Imaging Authors: Ali R. Sepahdari, Vinay K. Aakalu, Rashmi Kapur, Edward A. Michals, Nitu Saran, Adam French, and Mahmood F. Mafee AUTHOR INFO & AFFILIATIONS Volume 193, Issue 3 https://doi.org/10.2214/AJR.08.1838
- Spectrum of Orbital Cellulitis on Magnetic Resonance Imaging Ruchir Jyani 1, Dilip Ranade 1, Priscilla Joshi 1,? Editors: Alexander Muacevic, John R Adler Cureus. 2020 Aug 11;12(8):e9663. doi: 10.7759/cureus.9663
Dr. SHWETHA C
Junior Consultant
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. NIKITHA U N
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.