48 year old male Presented with history of 3 episodes of melena. No known comorbidities Gastro -Duodenoscopy - Erosive duodenitis Colonoscopy – unremarkable.
LEGENDS
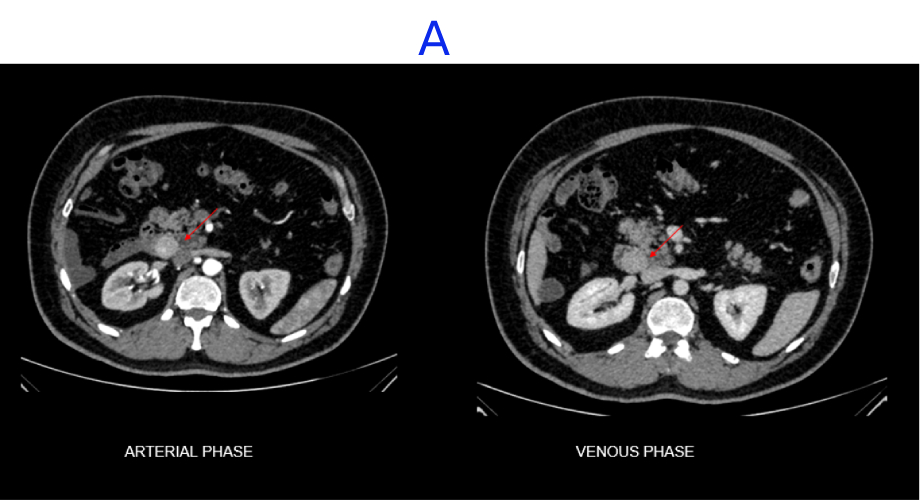
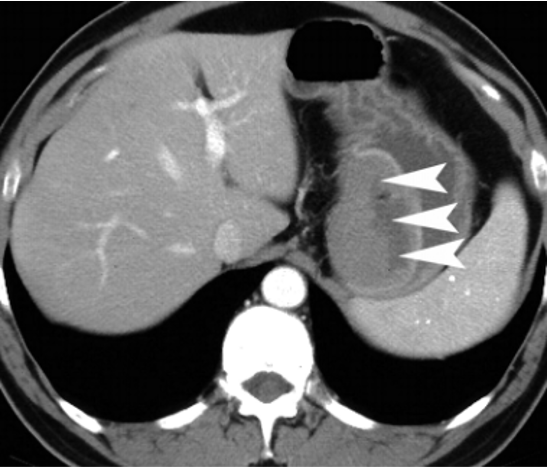
A. A well-defined, heterogeneously enhancing lesion seen in the D3 segment of the duodenum.
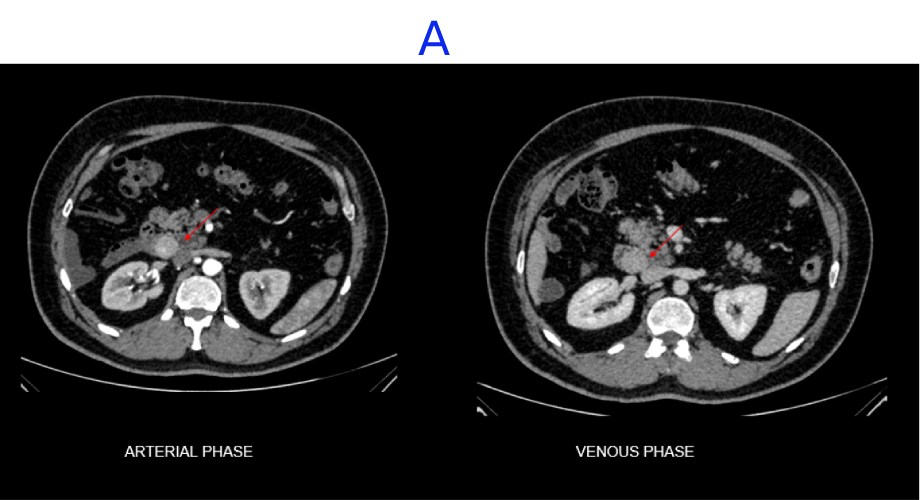
B. Few internal non-enhancing areas are seen in the superior aspect of the lesion.
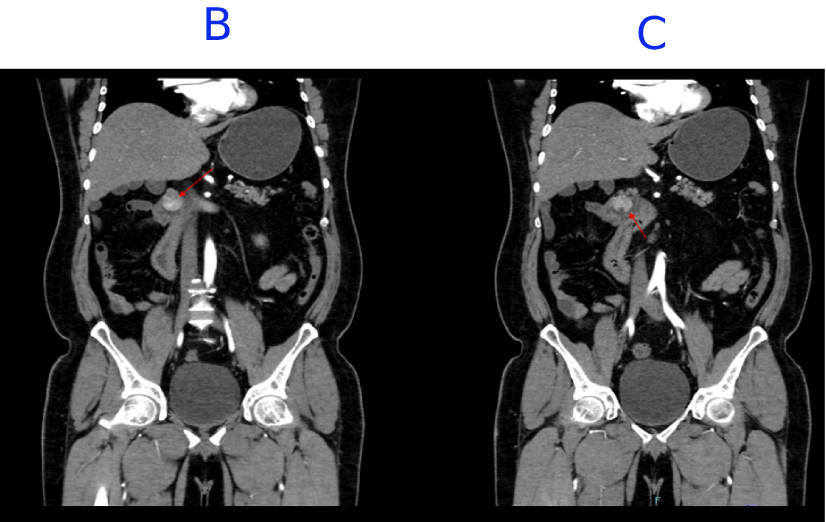
C. A focal defect seen in the inferior aspect of the lesion, suggestive of ulceration.
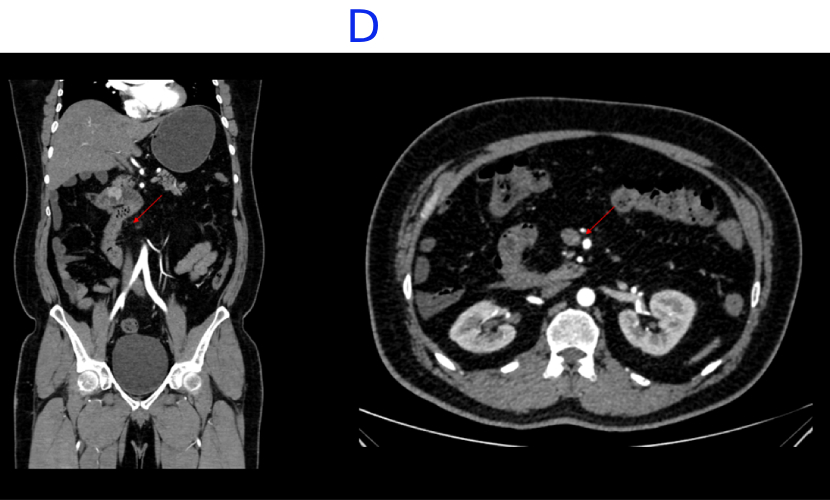
D. Incidental note of malrotation with the duodenojejunal junction lying to the right of the midline and altered SMA-SMV relationship.
DIAGNOSIS
GASTROINTESINAL STROMAL TUMOR
- GIST – spindle cell type.
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors to arise from the gastrointestinal tract. They are characterized by expression of a tyrosine kinase growth factor receptor, also called kit receptor or CD117.
The average patient with GIST is 40–70 years old.
Male to female incidence is now considered to be equal.
Stomach is the most common site, accounting for 60–70% .
Approximately one-third occur in the small bowel, with rare occurrence in the colon and rectum (5%), esophagus (< 2%), and appendix .
Some GISTs primarily arise in the omentum, mesentery, or retroperitoneum and are unrelated to the tubular gastrointestinal tract.
Clinical presentation is often vague. Abdominal pain or distention is the most common presentation of GISTs. Gastrointestinal bleeding or unexplained anemia is the next most common presentation. Duodenal tumors present with obstructive jaundice and may be confused with pancreatic cancer.
IMAGING FINDINGS:
- The predominant pattern seen is a heterogeneously enhancing exophytic mass.
- Small gastric GISTs may show intense enhancement with IV contrast administration; this is a less common finding in the small bowel, probably because enteric tumors are larger and more malignant at presentation.
- Hemorrhage can be seen in larger tumors on unenhanced images.
- An intraluminal component can occasionally be seen on CT.
- Mucosal ulceration occurs in 50% of gastric tumors shown by the presence of air or oral contrast material within the mass.
- Usually, GIST does not involve the bowel wall concentrically.
The tumors may also damage the myenteric plexus, allowing dilatation of lumen. The cavitation may allow air to collect in the nondependent aspect of larger tumors, described as the “Toricelli-Bernouilli” crescentic necrosis sign
MANAGEMENT
- In the absence of metastatic disease, complete surgical excision is undertaken and offers the best hope of cure.
- Lymphadenectomy is usually not required because these tumors do not show lymph node metastases.
- However, despite apparently complete resection with clear margins, the recurrence rate is high. This may be partly due to tumor rupture leading to mesenteric implants; hence, the risk of recurrence emphasizes the importance of having meticulous surgical technique For this reason, percutaneous biopsy is best avoided.
Gastrointestinal Stromal Tumors: Clinical, Radiologic, and Pathologic Features
https://doi.org/10.2214/ajr.184.3.01840803
Dr MADHU KUMAR S B
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr NIKITHA U N
Radiology Resident
Manipal Hospital, Yeshwanthpur, Bengaluru.