15-year boy with difficulty in rising from lying or sitting position and mild swelling in calf region.
15-year boy with difficulty in rising from lying or sitting position and mild swelling in the calf region.
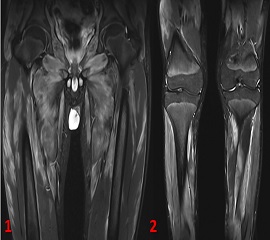
- Coronal STIR images of thigh and leg demonstrate patchy hyperintensity involving muscles around bilateral hip joints, bilateral thighs and legs with pattern of involvement being fairly symmetric bilaterally. Notice the absence of skin edema/fluid collections in muscles/perifascial planes (Fig 1 & 2).
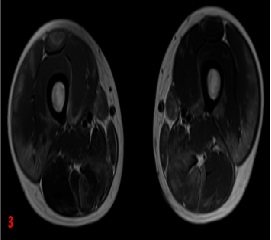
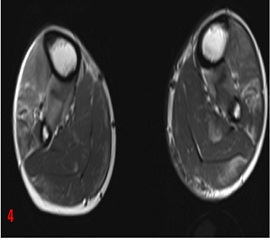
- Serial axial T2 sections at thigh and leg demonstrate the similar findings as described above with associated mild muscle enlargement (Fig 3 & 4).
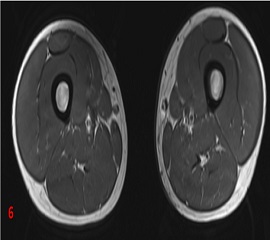
- Axial T1w image of thigh demonstrates no intramuscular T1 hyperintensity – to suggest haemorrhage or fatty infiltration (Fig 6).
DIAGNOSIS:
- Acute stage of muscular dystrophy.
DIFFERENTIAL DIAGNOSIS AND DISCUSSION:
Muscle edema is a frequently encountered finding on routine imaging studies with similar presentation in variety of disease processes. Carefully analyzing the pattern of distribution and surrounding soft tissue changes helps in arriving at a specific diagnosis.
Causes of skeletal muscle edema:
Muscular dystrophy:
- Muscular dystrophy is a broad group of rare genetic disorders characterized by progressive degeneration and muscle loss.
- The muscle initially is edematous (acute stage) and then rapidly becomes atrophic with fatty replacement. Findings are symmetrical and often involves specific muscle groups.
- Muscle involvement pattern differs with different subtypes with considerable overlap.
- Inflammatory features like skin and subcutaneous edema, perifascial fluid collections are conspicuously absent.
Other causes:
Post-traumatic (muscle strain):
- Muscle strain is an acute injury.
- By far the most common is the myotendinous junction pattern, which occurs roughly 97% of the time. The remaining 3% will show an epimysial strain pattern, with the abnormalities found at the periphery of the muscle.
- Depending on the severity of the strain, there might also be fluid collections, retraction or complete tear.
Inflammatory myopathy:
- Inflammatory myopathy is a term that defines a group of immune mediated muscle diseases involving inflammation of skeletal muscle and often the adjacent fascia, with elevated CPK (Creatine phosphokinase).
- Three disease entities, namely dermatomyositis (DM), polymyositis (PM), and inclusion body myositis (IBM) fall under this group.
Radiation myositis:
- Muscle and intermuscular septal edema due to vasculitis. Signal intensity changes peaks at 6-12 months after radiation and may be seen many years after the therapy.
- The history is usually the clue, but also a band like appearance where the radiation changes in the muscles stop, corresponding with the radiation field.
Muscle ischaemia:
- Common in diabetes and sickle cell anemia
- Thigh involved in 80%; calf involved in 20%
- Bilateral in one third of patients
- Diffuse intramuscular and intermuscular increased signal with diffuse enhancement of affected area or ring enhancement of necrotic foci
Muscle denervation:
- Occurs in a specific nerve distribution area commonly due to trauma or nerve entrapment.
- High signal in affected muscles on T2 in acute stage. In chronic stage atrophy and fatty replacement. Inflammatory features are absent.
Pyomyositis (Infection):
- Penetrating injury or hematogenous.
- Rare; usually in immunocompromised host
- Nonspecific MRI with high signal on T2 images in and around muscle with or without fluid collections.
APPROACH TO MUSCLE EDEMA

REFERENCES:
- Smitaman E, Flores DV, Mejía Gómez C, Pathria MN. MR imaging of atraumatic muscle disorders. Radiographics. 2018 Mar;38(2):500-22.
- McMahon CJ, Wu JS, Eisenberg RL. Muscle edema. American Journal of Roentgenology. 2010 Apr;194(4):W284-92.
Dr Vivek J, MD
Senior resident & Cross Section fellow
MHRG
Dr. Dayananda Sagar G, MD
Consultant radiologist
MHRG