One-year-old female infant presenting with a seizure disorder.
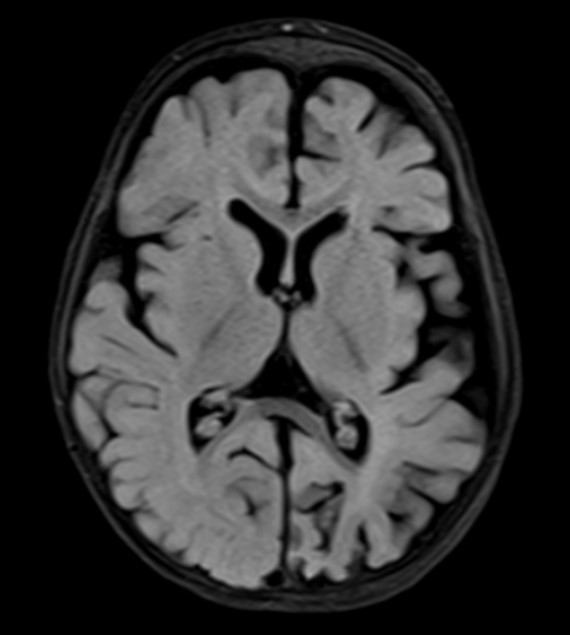
- T2 weighted image in axial sections shows hemi atrophy of the left cerebral hemisphere with prominent sulci and sub-arachnoid space.
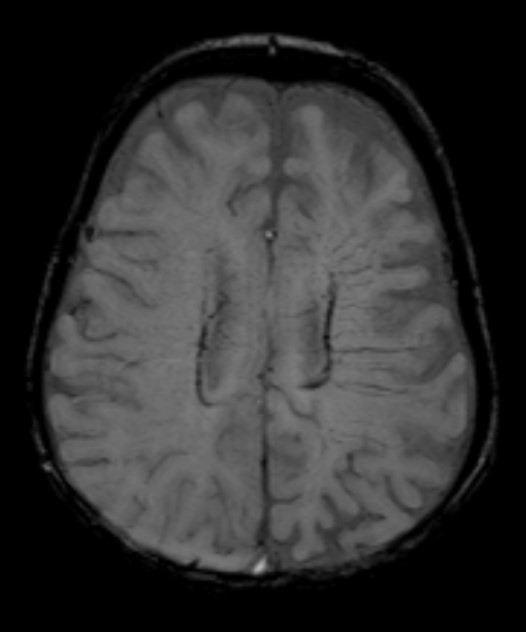
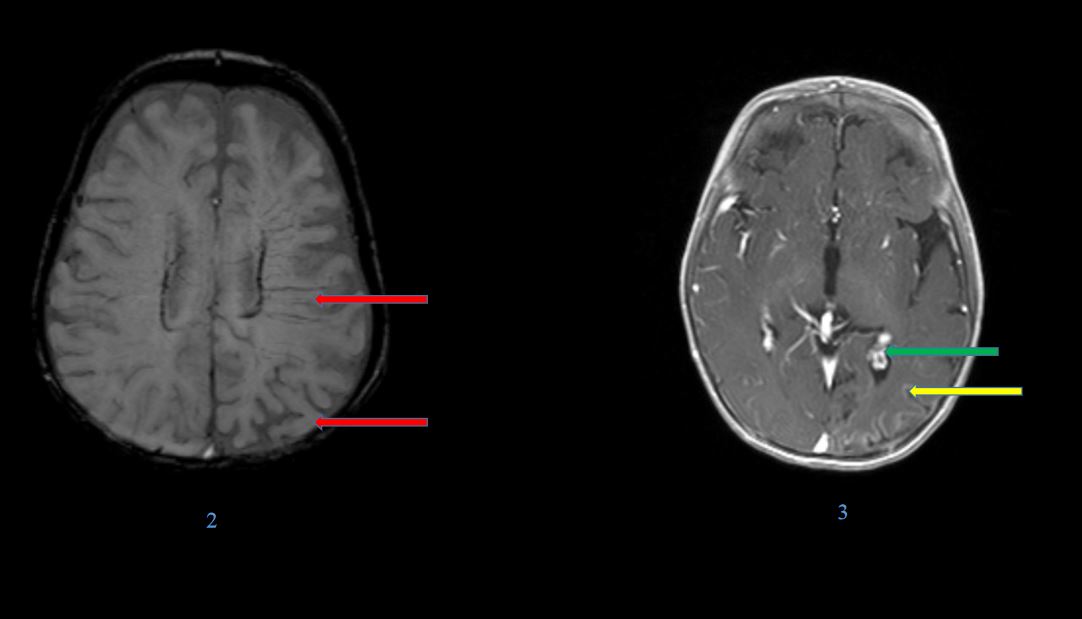
- Susceptibility images in axial sections show foci of blooming in the left parietal and occipital gyral region with prominent medullary veins.
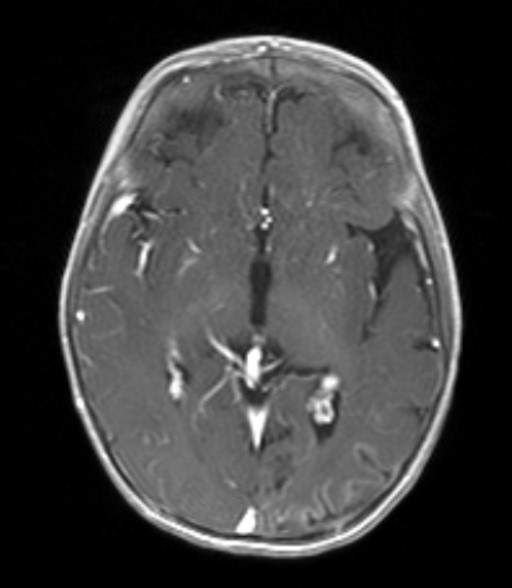
- T1 post-contrast images in axial sections showing gyral hyperintensity in left parietal and occipital lobes with prominent sub ependymal vein along the frontal horn of left lateral ventricle.
- On clinical examination – A note is made of a port wine stain on the face.
DIAGNOSIS : Sturge Weber syndrome
Discussion:
Also known as encephalo-trigeminal angiomatosis.
Hallmarks: variable combinations of
(1)A dermal capillary-venular malformation in the sensory distribution of the trigeminal nerve.
(2)Retinal choroidal angioma (either with or without glaucoma).
(3)A cerebral capillary venous leptomeningeal angioma.
Genetics: GNAQ mutations causing an overlapping phenotypic spectrum of vascular and melanocytic birthmarks.
Pathology: A tangle of thin-walled vessels—multiple enlarged capillaries and venous channels—forms the characteristic leptomeningeal (pial) angioma. The angioma covers the brain surface, dipping into the enlarged sulci between shrunken apposing gyri.
Presentation:
Patients exhibit a nevus flammeus—formerly termed a facial “angioma” or “port-wine stain”—that is plainly visible at birth.
It can be uni- (63%) or bilateral (31%) and is distributed over the skin innervated by one or more sensory branches of the trigeminal nerve.
Imaging: CT
- Detects subcortical calcification at an earlier age than plain film and can also demonstrate associated parenchymal volume loss.
- Tram track sign of cortical and subcortical calcification.
- Calvarial and regional sinus enlargement may be evident.
- Ipsilateral choroid plexus may be enlarged.
- In severe cases, a Dyke-davidoff-mason appearance may be seen.
- Orbital choroidal hemangioma may be present
- Asymmetric cavernous sinus enlargement.
Patients exhibit a nevus flammeus—formerly termed a facial “angioma” or “port-wine stain”—that is plainly visible at birth.
It can be uni- (63%) or bilateral (31%) and is distributed over the skin innervated by one or more sensory branches of the trigeminal nerve.
Imaging: CT
- Detects subcortical calcification at an earlier age than plain film and can also demonstrate associated parenchymal volume loss.
- Tram track sign of cortical and subcortical calcification.
- Calvarial and regional sinus enlargement may be evident.
- Ipsilateral choroid plexus may be enlarged.
- In severe cases, a Dyke-davidoff-mason appearance may be seen.
- Orbital choroidal hemangioma may be present
- Asymmetric cavernous sinus enlargement.
MR Findings.
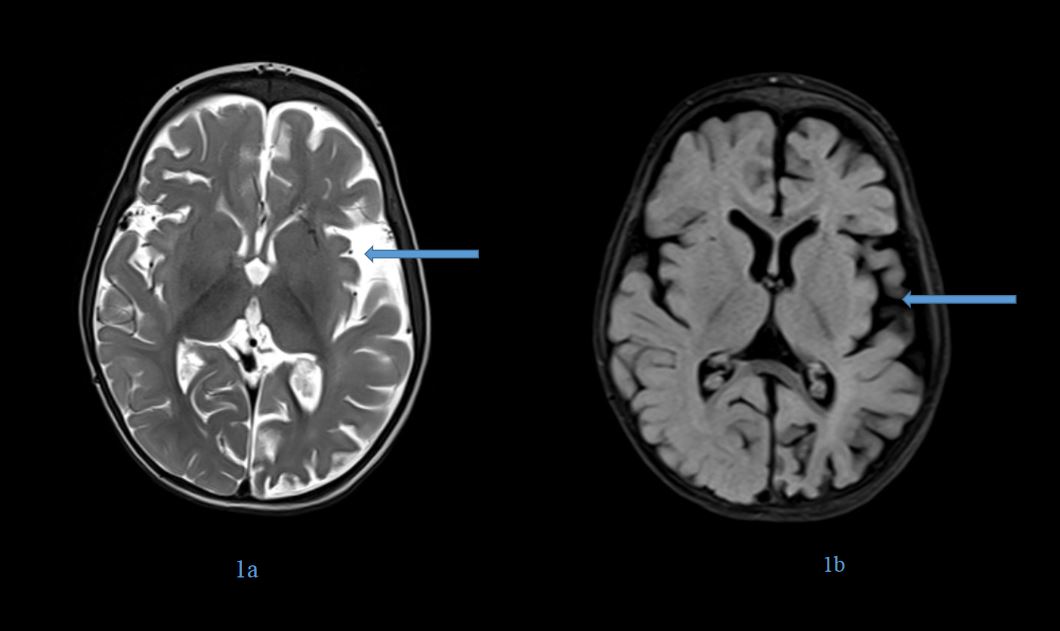
- T1 and T2 scans show volume loss in the affected cortex with enlargement of the adjacent subarachnoid spaces. Myelination is usually normal or even accelerated, and malformations of cortical development may be present.
- White matter ischemic damage with subcortical T2/FLAIR hyperintensities in the affected hemisphere is common in older patients.
- Dystrophic cortical/subcortical calcifications are seen as linear hypo intensities on T2WI that “bloom” on T2* (GRE, SWI). SWI scans often demonstrate linear susceptibility in enlarged medullary veins.
- FLAIR scans may demonstrate serpentine hyperintensities in the sulci, the “ivy” sign.
- DWI is usually negative unless acute ischemia is present.
- Postcontrast T1WI or FLAIR sequences best demonstrate the pial angioma. Serpentine enhancement covers the underlying gyri, extending deep into the sulci and sometimes almost filling the subarachnoid space.
- Enlarged medullary veins—sources of compensatory collateral venous drainage—can sometimes be identified as linear enhancing foci extending deep into the hemispheric white matter.
- The ipsilateral choroid plexus is almost always enlarged and enhances intensely.
- Angiography. DSA typically demonstrates a lack of superficial cortical veins with corresponding dilatation of deep medullary and subependymal veins.
Differential diagnosis:
- Meningioangiomatosis.
- Blue rubber bleb nevus
- Syndrome and Wyburn-Mason syndrome
References:
- Boukobza M, Enjolras O, Cambra M, Merland J. Sturge-Weber syndrome. The current neuroradiologic data J Radiol 2000 Jul;81(7):765-71. (PMID: 10915989)
- Fischbein NJ, Barkovich AJ, Wu Y, Berg BO. Sturge-Weber syndrome with no leptomeningeal enhancement on MRI. Neuroradiology 1998 Mar;40(3):177-80. (PMID: 9561524)
- Griffiths PD, Blaser S, Boodram MB, Armstrong D, Harwood-Nash D. Choroid plexus size in young children with Sturge-Weber syndrome. AJNR Am J Neuroradiol. 1996 Jan;17(1):175- 80. (PMID: 8770273)
- Griffiths PD, Boodram MB, Blaser S, Altomare F, Buncic JR, Levin AV, Jay V, Armstrong D, Harwood-Nash D. Abnormal ocular enhancement in Sturge-Weber syndrome: correlation of ocular MR and CT findings with clinical and intracranial imaging findings. AJNR Am J Neuroradiol. 1996 Apr;17(4):749-54. (PMID: 8730196)
- Hart BL, Depper MH, Clericuzio CL. Neurocutaneous syndromes. In Orrison WW (ed) Neuroimaging. W.B. Saunders & Co., Philadelphia (2OOO).
Dr. Srinivas P
Cross-sectional Fellow
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru
Dr. Harsha Chadaga
Lead Neurology Imaging and Senior Consultant Radiologist.
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.
Dr. Sriram Patwari
Consultant Radiologist
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.