Sudden onset restlessness and breathlessness with few episodes of seizures in a patient with haematological malignancy
- Sudden onset restlessness and breathlessness with few episodes of seizures in a patient with haematological malignancy.
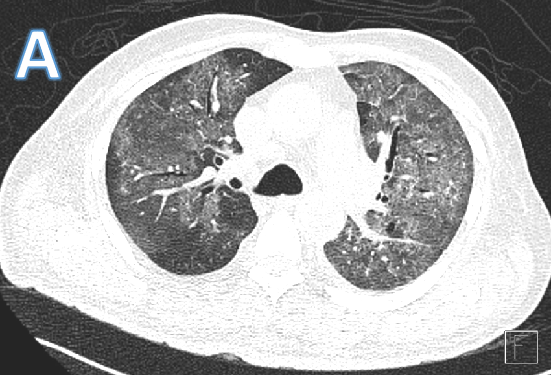
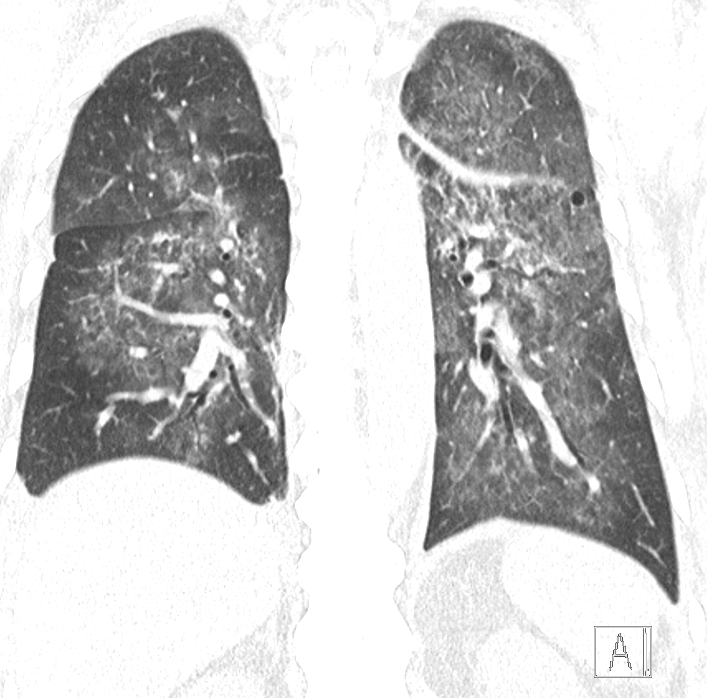
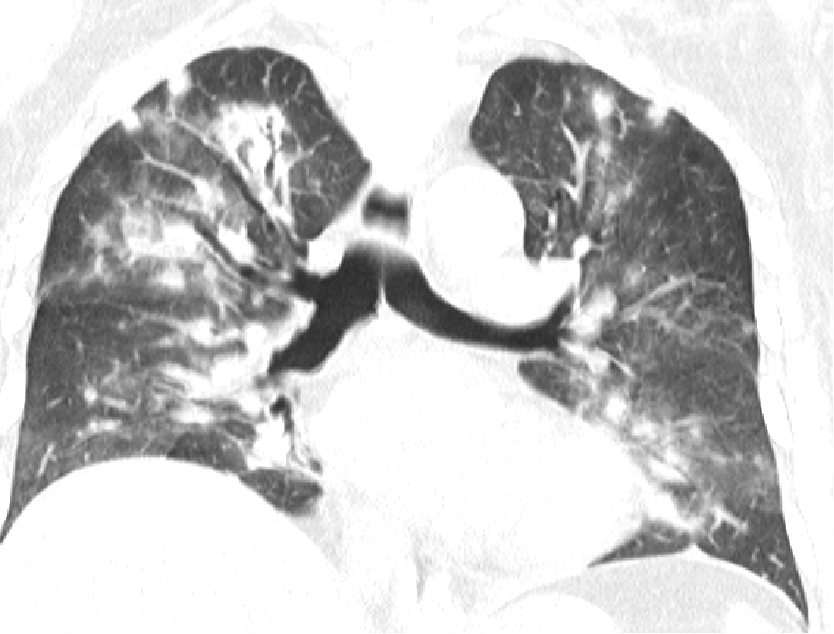
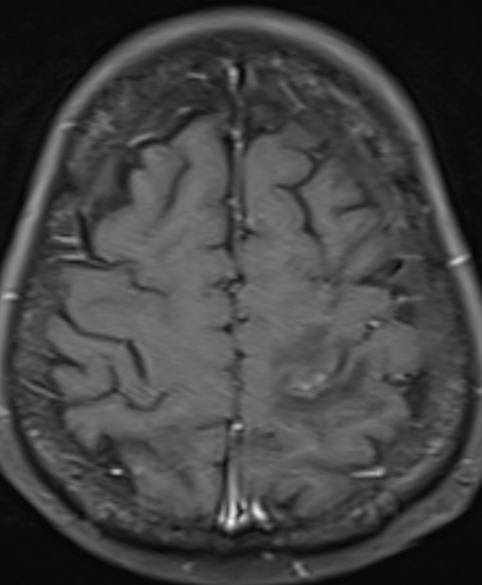
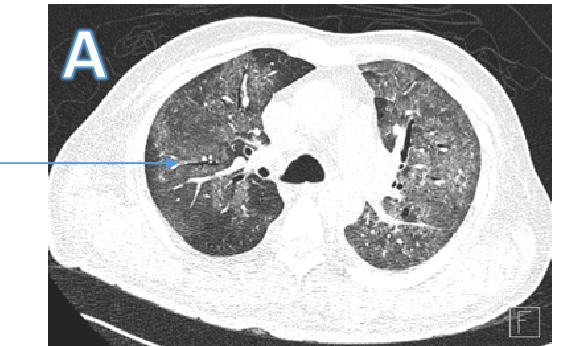
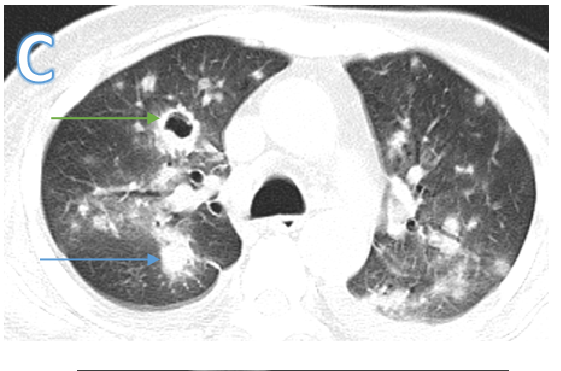
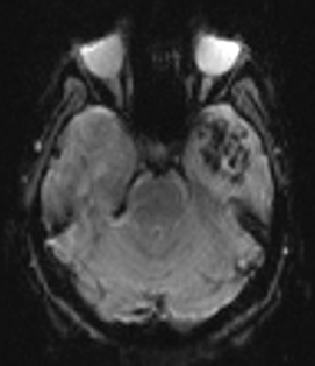
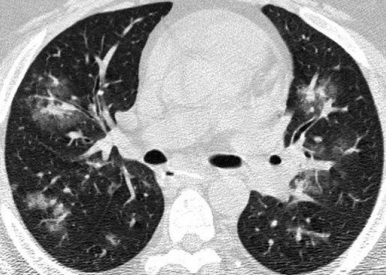
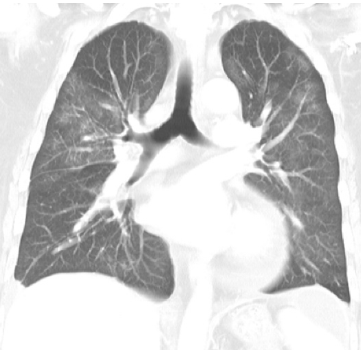
Fig A
- Blue arrows - Bilateral peribronchovascular groundglass opacities
- Green arrows - Pulmonary cysts.
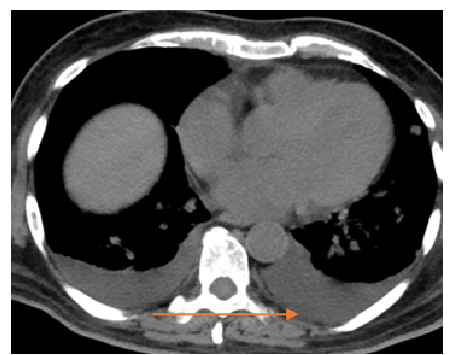
- Orange arrows - Right sided mild to moderate and left mild effusion
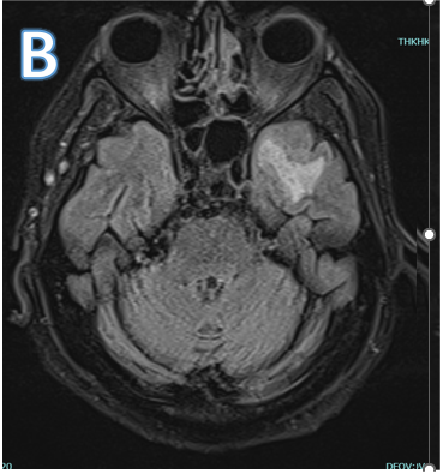
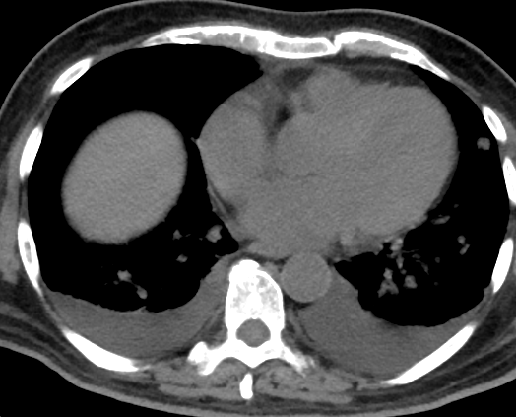
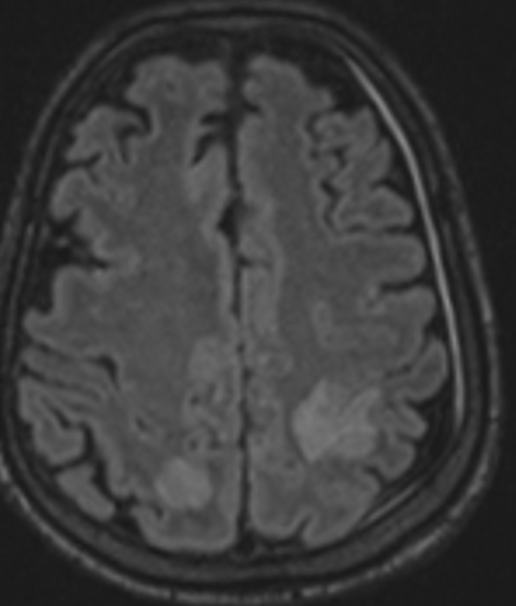
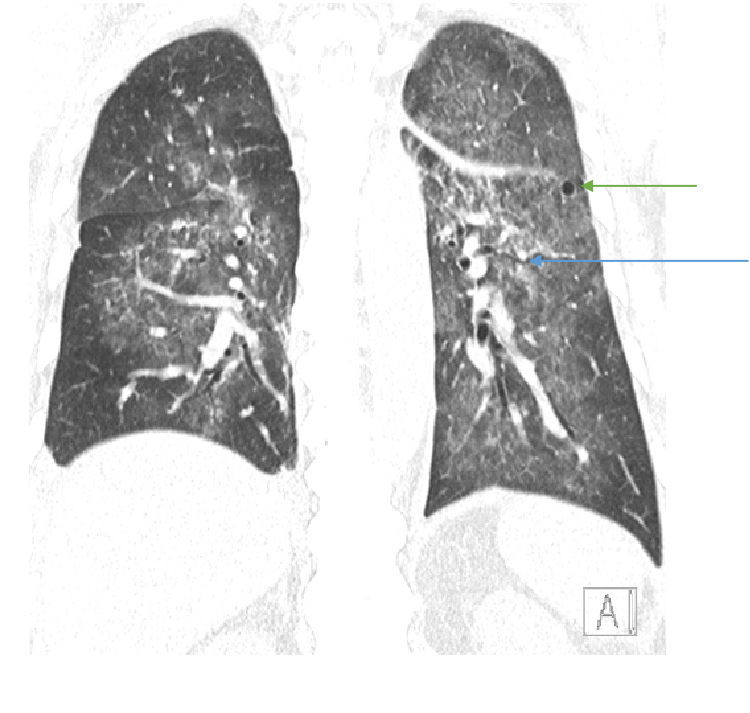
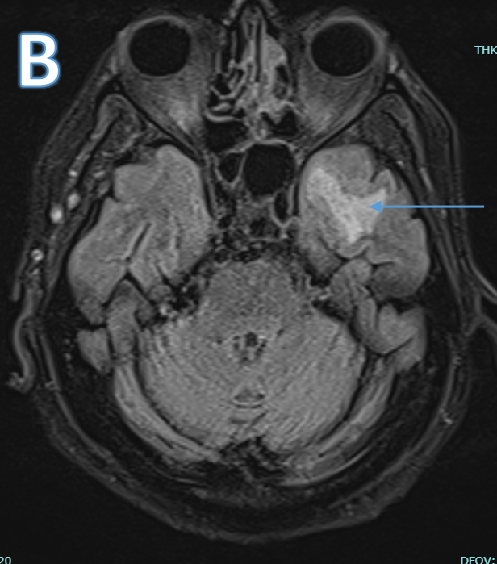
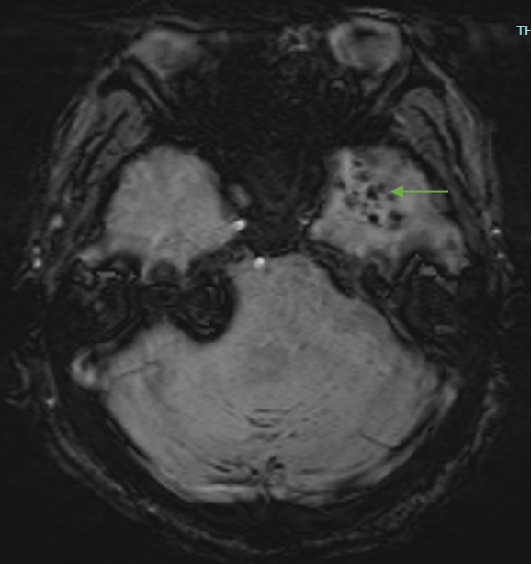
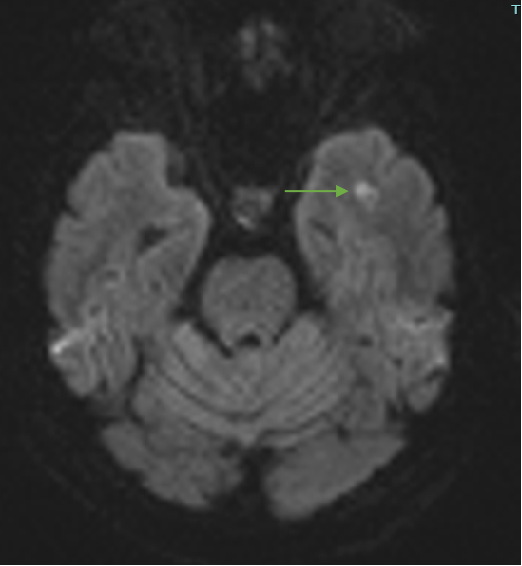
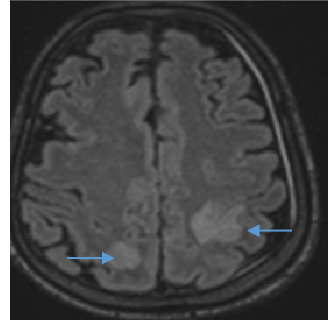
Fig B
- Blue arrow - FLAIR hyperintensity in left anterior temporal lobe
- Green arrow - foci of diffusion restriction and blooming.
- Orange arrow - Tiny blooming focus in splenium of Corpus callosum.
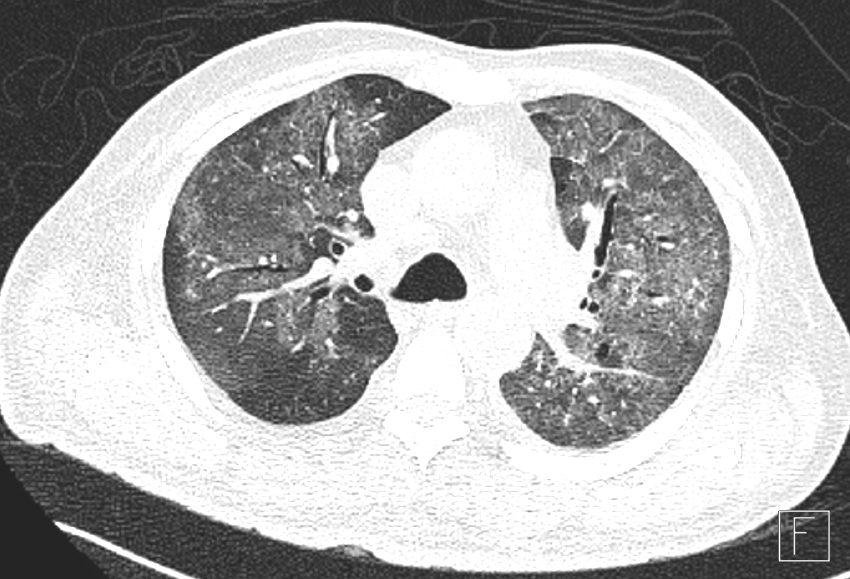
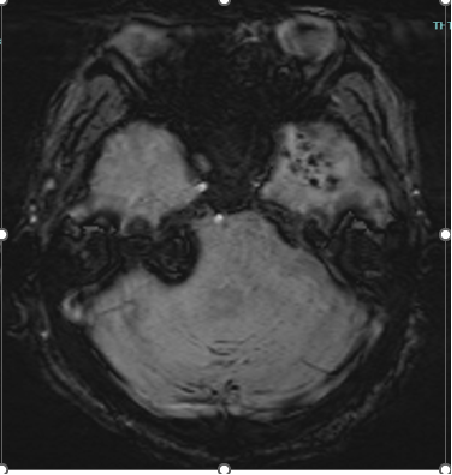
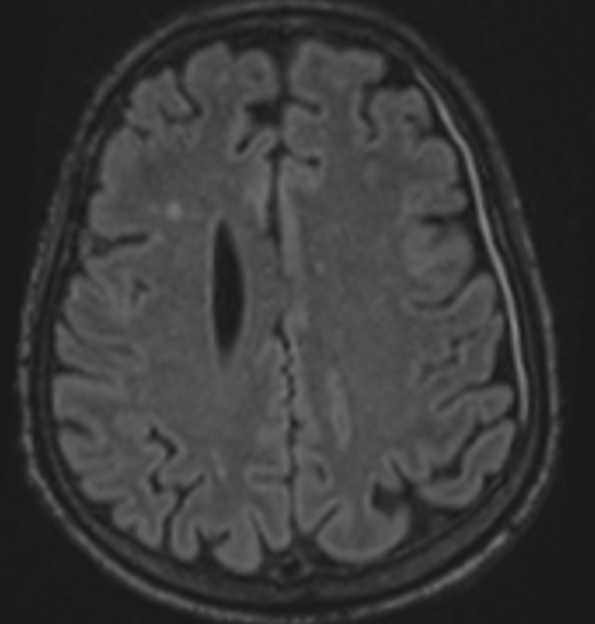
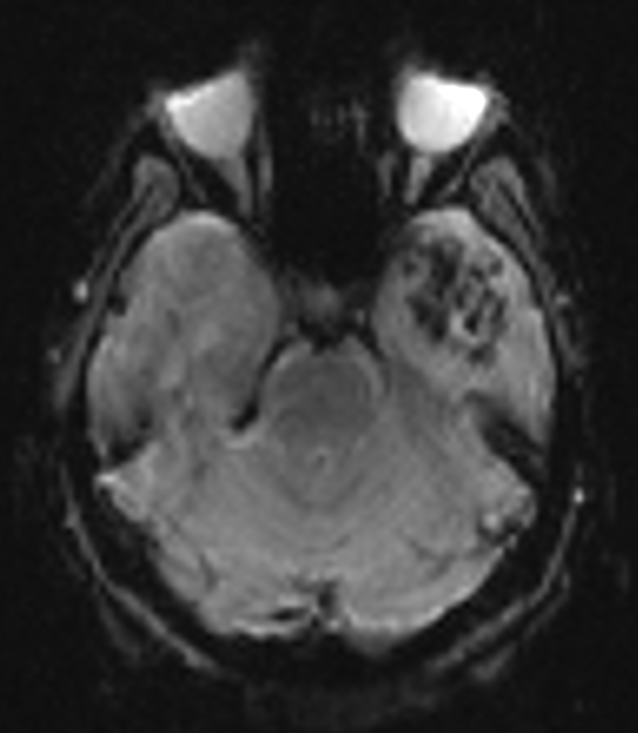
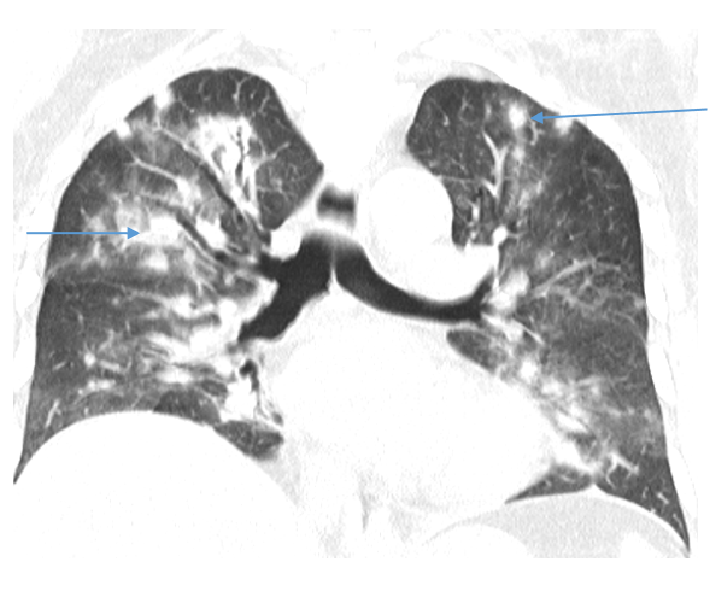
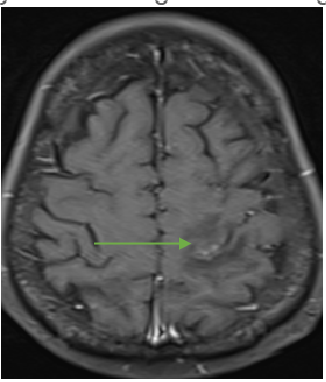
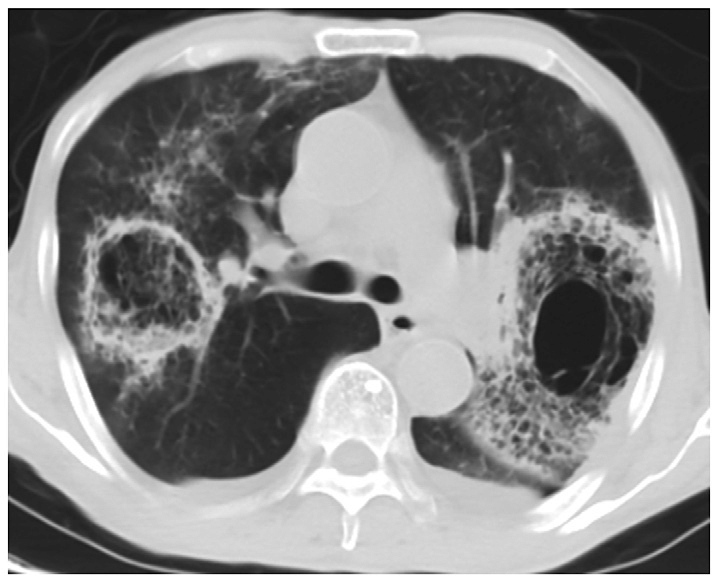
Fig C
Follow up scan after 2 weeks
- Blue arrow - Diffusely scatter areas of nodular consolidation and ground glass densities of varying sizes are seen in both lungs in all segments.
- Green arrow - Few of these nodules also show central cavitation peri nodular ground glass halo ( cavitating consolidation).
- Orange arrow – Bilateral pleural effusion(Interval increase)
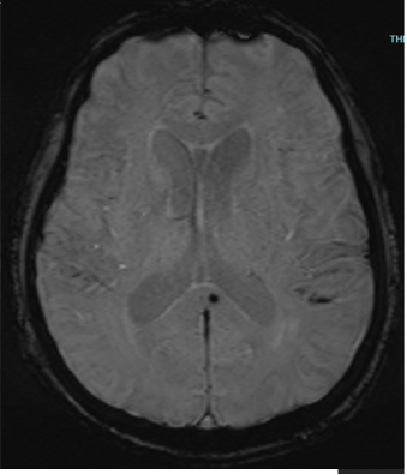
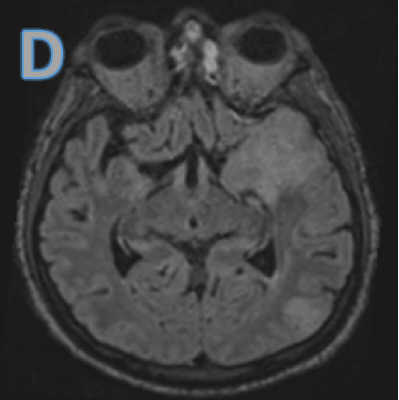
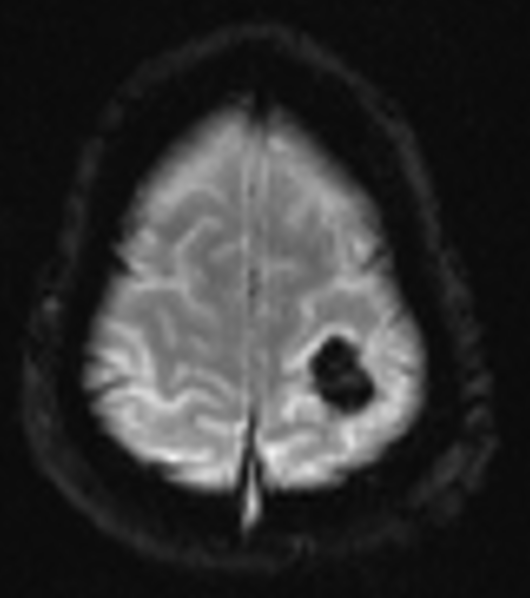
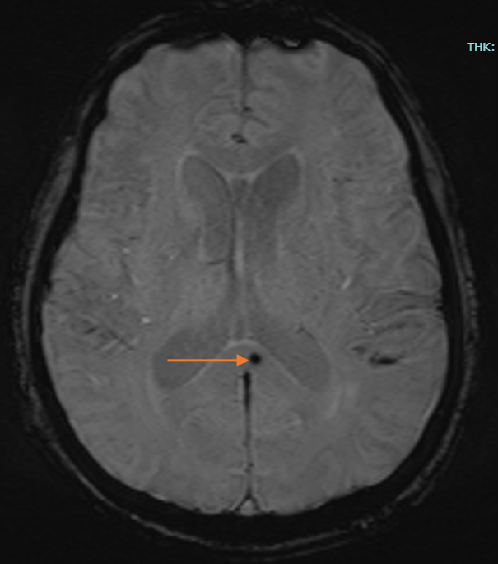
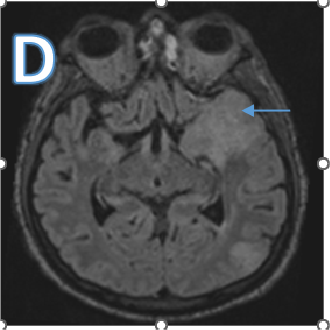
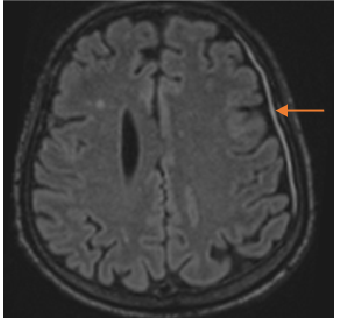
Fig D
Follow up after 3 days
- Blue arrow - Interval new finding of FLAIR hyperintensities in bilateral high parietal and left posterior temporal cortex and sub cortical white matter.
- Green arrow - Focus of post contrast enhancement in the left high parietal region. Microhaemorrhages within the lesions.
- Orange arrow - Diffuse enhancing pachymeningeal thickening in the left fronto-parietal and temporal convexities.
CASE SUMMARY
- Patient with diagnosed acute promyelocytic leukaemia presented with Sudden onset of breathlessness and restlessness with 3-4 episodes of seizures.
- Provisional diagnosis on CT chest at admission was pneumocystis jiroveci induced pneumonia in view of ground glass opacities and tiny pulmonary cysts.
- Follow up CT showed multiple nodular consolidation with cavitation.
- MRI brain at admission and follow up showed multifocal embolic infarcts.
- LP and CSF analysis was done which confirmed fungal etiology.
FINAL DIAGNOSIS - In a Known case of APML, pulmonary septic emboli and septic brain embolic infarcts and meningitis of fungal etiology.
DISCUSSION
- Hematologic malignancies are a heterogeneous group of diseases including myeloid neoplasms, lymphoid neoplasms (leukaemia and lymphoma), lymphoproliferative disorders, and plasma cell disorders.
- Treatment modalities : Chemotherapeutic agents , hematopoietic stem cell transplantation (HSCT).
- They are at risk for various acute pulmonary complications including
- Infections
- Drug induced pneumonitis
- Pulmonary infiltration by disease process.
ACUTE INFECTIOUS PULMONARY COMPLICATIONS
- BACTERIAL PNEUMONIA
- FUNGAL PNEUMONIA
- PNEUMOCYSTIS JIROVECI INDUCED PNEUMONIA
- CMV INDUCED PNEUMONIA
FUNGAL PNEUMONIA
- Risk Factor : Neutropenia, relapse/ refractory disease, pervious history of invasive fungal infection , and receiving high doses of corticosteroids.
- Neutropenia (<100/µL) lasting for more than 10 days is considered as prolonged neutropenia and is a serious risk for IFIs.
Aspergillus (Most common)
Aspergillus infection commonly occurs in the neutropenic phase during the first 30 days after HSCT.
Radiographic features:
- Angioinvasive aspergillosis: “halo” sign, segmental or subsegmental pleura-based consolidation, cavitation during convalescence.
- Airway-invasive aspergillosis: centrilobular nodules, peribronchial or peribronchiolar consolidations.
Diagnosis
- Aspergillus galactomannan antigen test, detection of Aspergillus in BAL fluid or lung tissue samples.
Septic emboli Pathogenesis
Results from obstruction of a blood vessel, typically by an infected thrombus that has traveled through the bloodstream from a distant infectious source and blocked a blood vessel.
Two insults –
a)Early embolic/ischemic insult due to vascular occlusion that may lead to infarction
b)The infectious insult that leads to inflammation and possible abscess formation. Fungi, mostly Candida and Aspergillus, may be found in septic emboli (E. Rubinstein et al., 1995).
Differential diagnosis:
Other fungal infections
- Candidiasis produces multiple focal patches of consolidation, cavitation, and pulmonary nodules with surrounding ground glass opacities
- Mucormycosis is indistinguishable from invasive aspergillosis at CT, a reversed halo sign is seen more frequently in mucormycosis than in invasive pulmonary aspergillosis. ‘Bird’s nest’ is a typical appearance
PNEUMOCYSTIS JIROVECI INDUCED PNEUMONIA
- In patients who have undergone HSCT, P jiroveci–induced pneumonia usually occurs between 30 and 100 days after transplantation.
- Radiological findings:
Widespread perihilar ground-glass opacities with a mosaic pattern. - Crazy paving:
Other atypical and variable radiographic patterns, including lung nodules, masses, lobar consolidation, bronchiectasis, and bronchiolitis.
Bacterial pneumonia
- Risk factor : Neutropenia and severely immunocompromised patients.
- The most common pathogen - Pseudomonas; other organisms include Nocardia, Legionella, H influenzae, and Enterobacter .
- The standard test for diagnosing the cause of a pulmonary infection - Microscopic examination of BAL fluid sampled with bronchoscopy.
- Radiologic findings :
Airspace consolidation, segmental or lobar consolidation.
Small airway plugging and branching centrilobular nodules (tree-in-bud appearance).
CMV pneumonia
- CMV infection is the most common cause of viral pneumonia among immunocompromised patients.
- Other respiratory viruses - Rhinoviruses, adenoviruses, influenza viruses, parainfluenza viruses, respiratory syncytial virus, metapneumovirus.
- CMV : occurs within 31–100 days after transplantation.
- Radiographic findings : Multifocal, are mostly bilateral ground-glass opacities, micronodules, airspace consolidation, reticular opacities.

References
- Choi, M. H., Jung, J. I., Chung, W. D., Kim, Y., Lee, S., Han, D. H., Ahn, M. I., & Park, S. H. (2014). Acute Pulmonary Complications in Patients with Hematologic Malignancies. Radiographics, 34(6), 1755–1768. https://doi.org/10.1148/rg.346130107
- Elsaghir, H., & Khalili, Y. A. (2023, June 26). Septic emboli. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK549827/
- Walker, C. M., Abbott, G. F., Greene, R. E., Shepard, J. O., Vummidi, D., & Digumarthy, S. R. (2014). Imaging Pulmonary infection: Classic signs and patterns. American Journal of Roentgenology, 202(3), 479–492. https://doi.org/10.2214/ajr.13.11463
- Wang, Junwei & Zhang, Chuanyu & Lin, Jizheng & Zhang, Liang & Li, Jie & Yang, Fangfang. (2019). Clinical diagnostic value of spiral CT in invasive pulmonary fungal infection. Experimental and Therapeutic Medicine. 17. 10.3892/etm.2019.7412.
Dr Deepti H.V.
MBBS, DMRD, DNB , EDiR , Fellowship (Fetal Medicine)
Senior Consultant ,MHRG
Dr Ankit Kataria
MBBS,MD
Cross section fellow MHRG