History of gradually increasing pain and swelling in distal end of femur
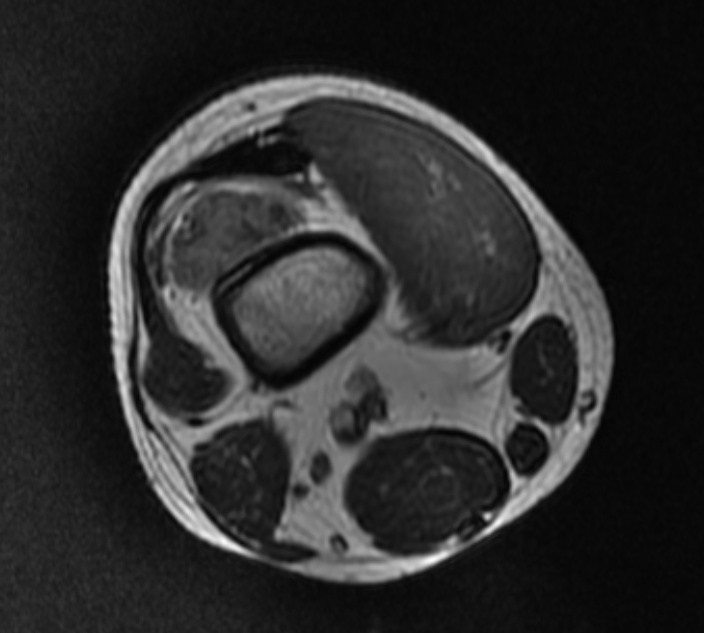
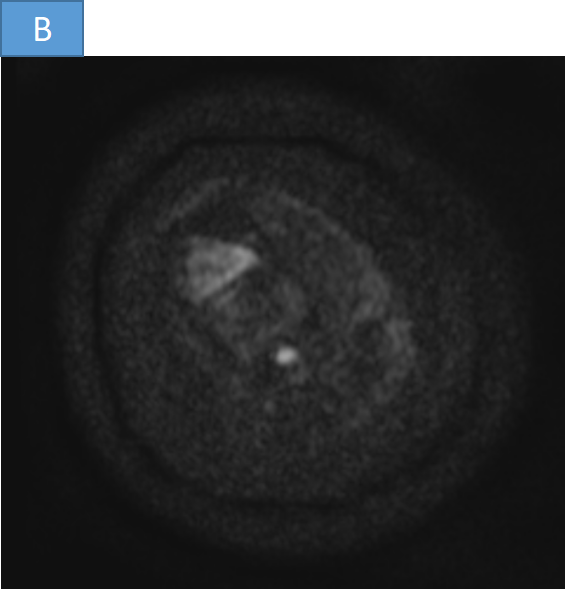
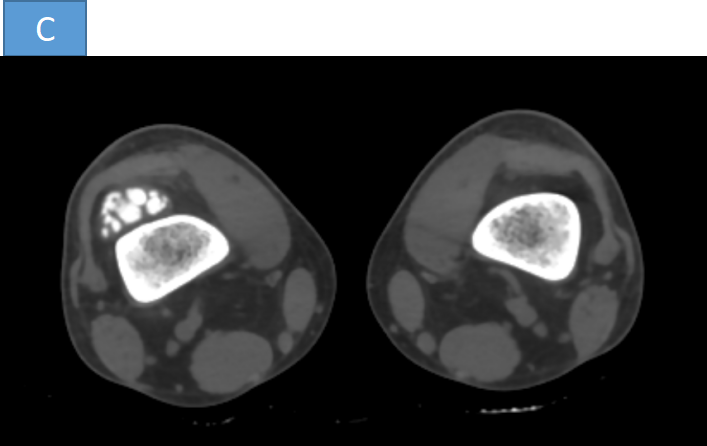
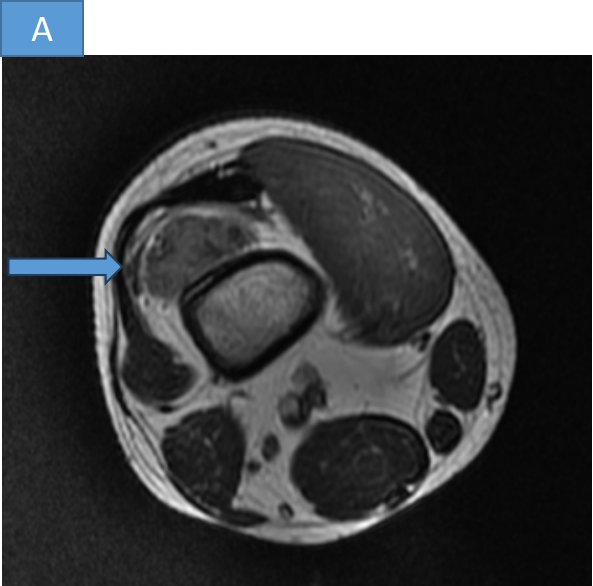
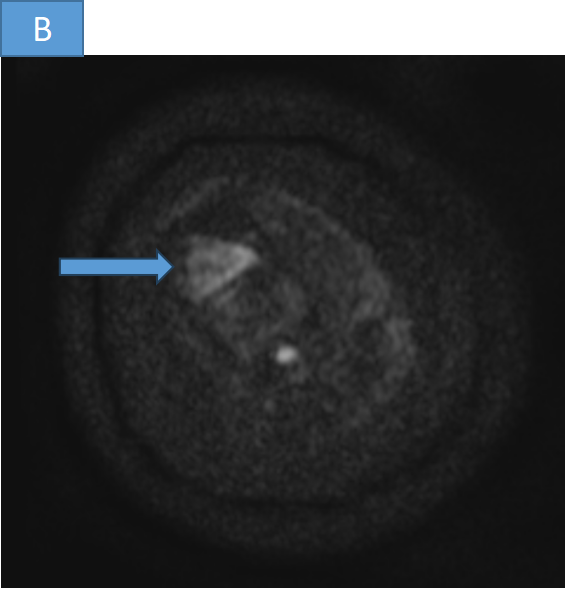
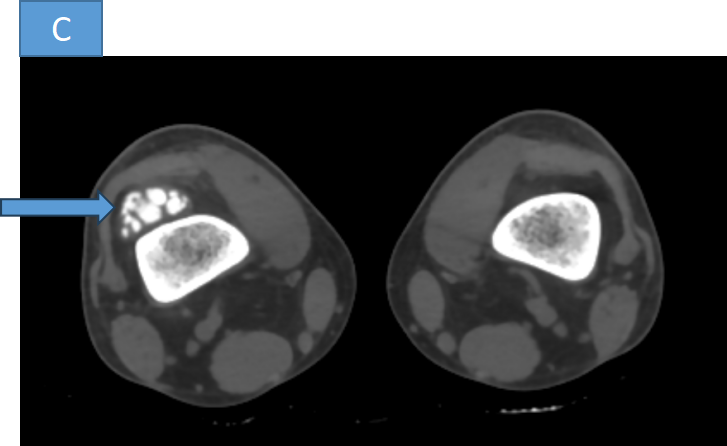
- A well circumscribed T2 isointense lesion ( Fig A) located anterior to the distal metaphysis of femur showing dense coarse calcification on corresponding CT ( Fig C). The lesion is broad base towards the cortex, no evident periosteal reaction in the underlying cortex. The lesion shows minimal restricted diffusion ( Fig B).
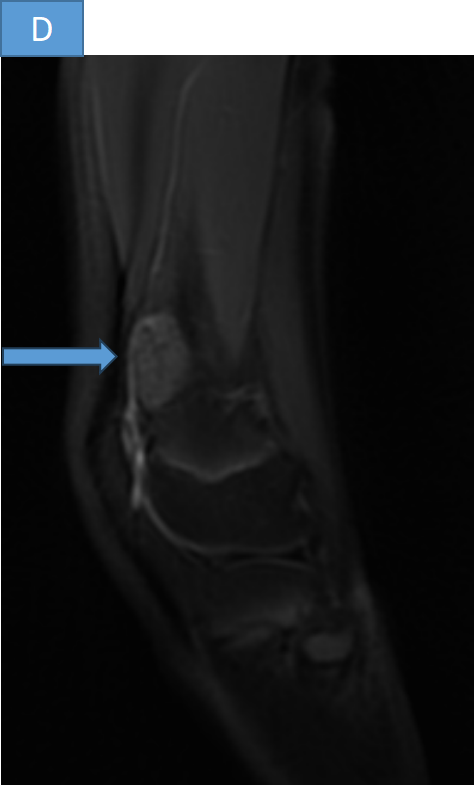
- T2FS shows mildly hyperintense lesion ( Fig C) and T1 shows hypointense lesion ( Fig D) located anterior to the distal metaphysis of femur
DIAGNOSIS
- Parosteal osteosarcoma.
DISCUSSION
Parosteal osteosarcoma
- Parosteal Osteosarcoma is a malignant, low-grade, osteosarcoma that occurs on the surface of the metaphysis of long bones.
- Patients typically present between ages 30 and 40 with a pain less mass.
- It is the most common type of juxta cortical or surface osteosarcoma and accounts for ~4% of all osteosarcomas.
- Occurs on surface of metaphysis of long bones.
- Most common sites include posterior distal femur, proximal tibia, and proximal humerus
- 80% cases occur in the femur
- Marrow invasion occurs in 25% of cases
Diagnostic criteria according to the WHO classification of soft tissue and bone tumors (5th edition) :
- Imaging features of a bone tumor
- Parosteal location with the origin on the cortical surface of the bone
- Histology of a low-grade spindle cell tumor with woven bone formation.
Radiographic features
- Large lobulated exophytic, cauliflower-like mass with central dense ossification adjacent to the bone.
- String sign: thin radiolucent line separating the tumor from the cortex, seen in 30% of cases
- Tumor stalk: grows within the tumor in late stages and obliterates the radiolucent cleavage plane
- Cortical thickening without aggressive periosteal reaction is often seen tumor
- Extension into the medullary cavity is frequently seen
- Parosteal osteosarcomas might progress to a high-grade sarcoma including other osteosarcoma variants, undifferentiated spindle cell sarcoma or rhabdomyosarcoma
- Treatment - Operative wide local surgical excision
Parosteal osteosarcoma
- Low grade
- Sclerotic lesion over the surface of bone.
- Thickening of the cortex and presence of a periosteal line between the tumor and the normal bone (string sign).
Periosteal osteosarcoma.
- Intermediate grade
- Broad based soft tissue mass
- Destruction of underlying bone with perpendicular periosteal reaction going into the soft tissue mas
References
- Bonar SFM, Klein MJ, O’Donell PG. Periosteal osteosarcoma. In: WHO Classification of Tumours Editorial Board. Soft tissue and bone tumours. Lyon (France): International Agency for Research on Cancer; 2020. (WHO classification of tumours series, 5th ed.; vol. 3). https://publications.iarc.fr
- MD/PhD, P. O. (n.d.). Periosteal osteosarcoma - Pathology - orthobullets. https://www.orthobullets.com/pathology/8016/periosteal-osteosarcoma
- Fox M & Trotta B. Osteosarcoma: Review of the Various Types with Emphasis on Recent Advancements in Imaging. Semin Musculoskelet Radiol. 2013;17(2):123-36. doi:10.1055/s-0033-1342969 - Pubmed
- Harper K, Sathiadoss P, Saifuddin A, Sheikh A. A Review of Imaging of Surface Sarcomas of Bone. Skeletal Radiol. 2021;50(1):9-28. doi:10.1007/s00256-020-03546-1 - Pubmed
- Murphey M, Jelinek J, Temple H, Flemming D, Gannon F. Imaging of Periosteal Osteosarcoma: Radiologic-Pathologic Comparison. Radiology. 2004;233(1):129-38. doi:10.1148/radiol.2331030326 - Pubmed
DR DEEPTI H V
Senior consultant ,MHRG
DR ANKIT KATARIA
Cross sectional fellow, MHRG