C/O heavy and frequent bleeding post MTP last month, no pain abdomen
FINDINGS:
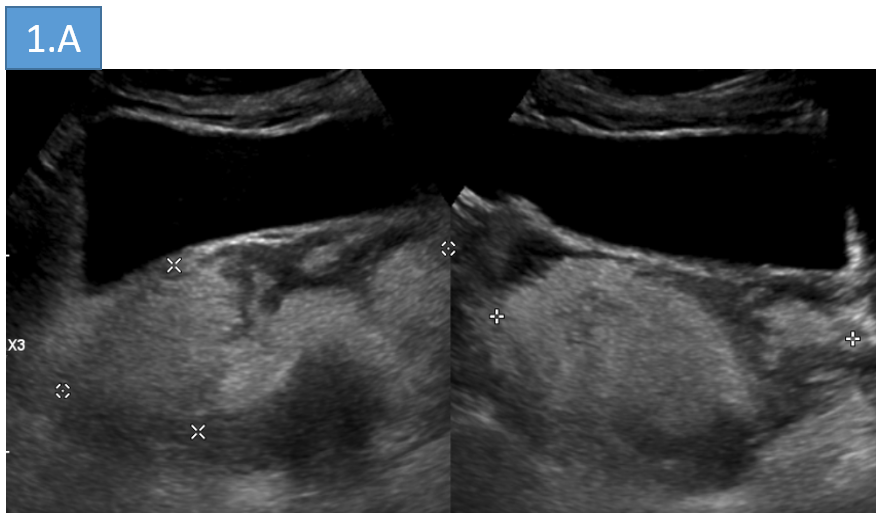
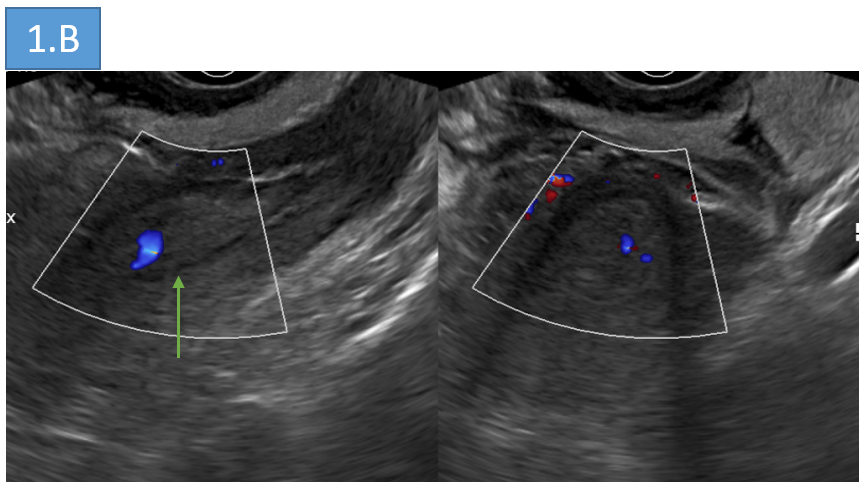
- 1: ULTRASOUND IMAGING
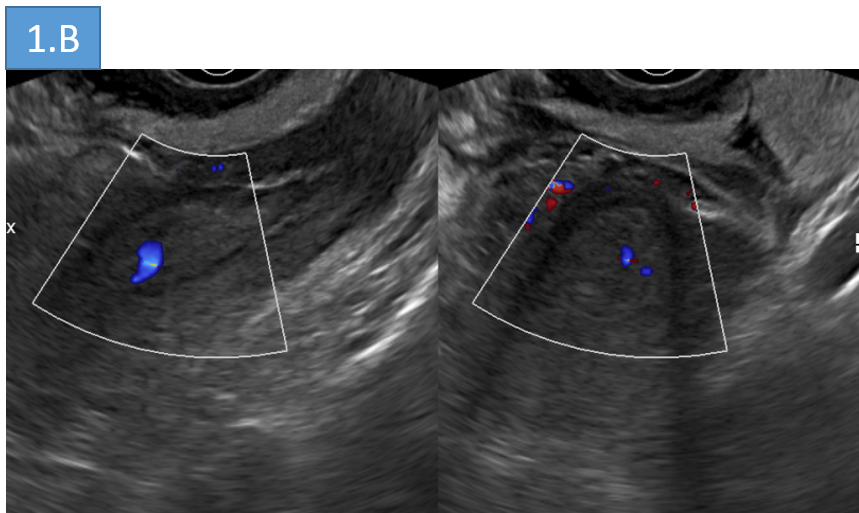
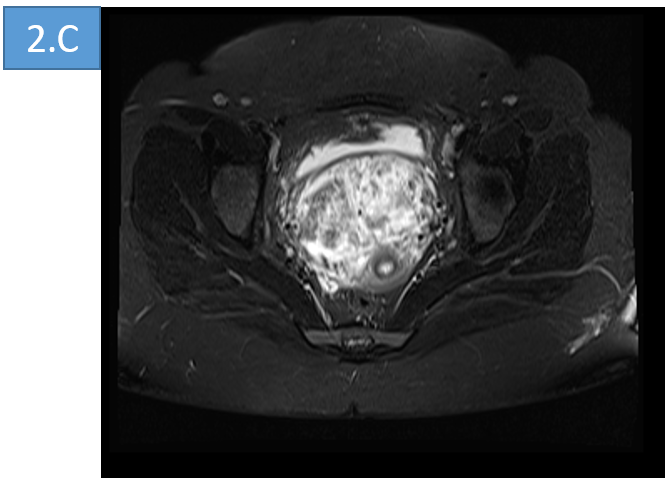
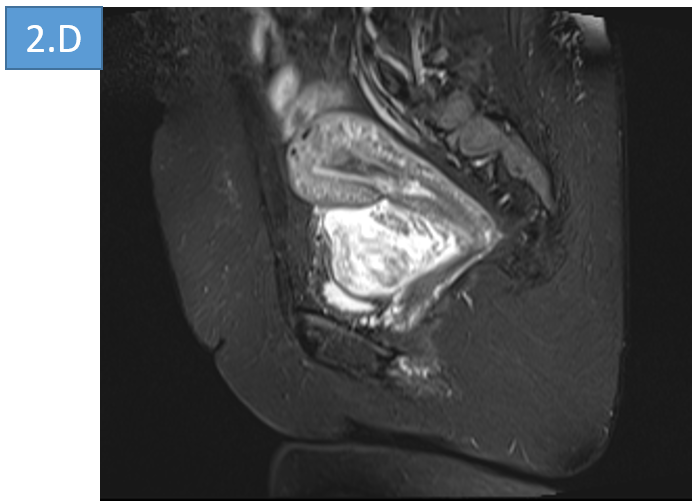
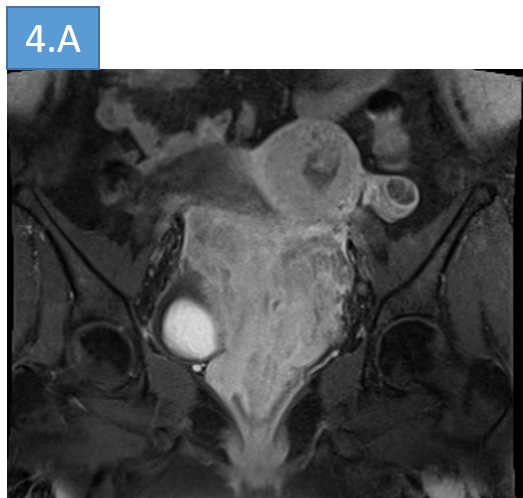
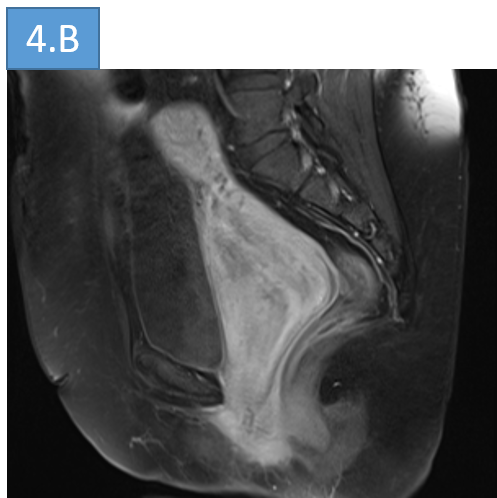
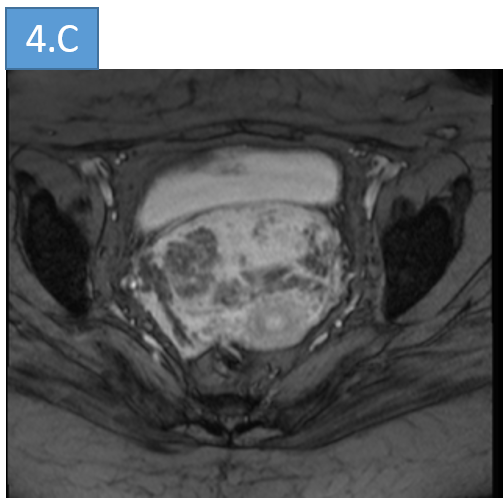
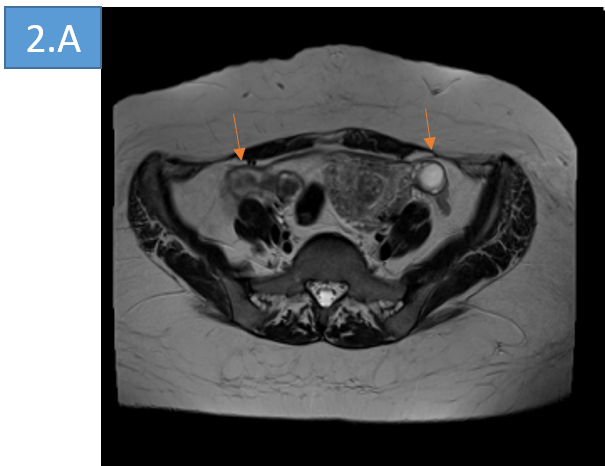
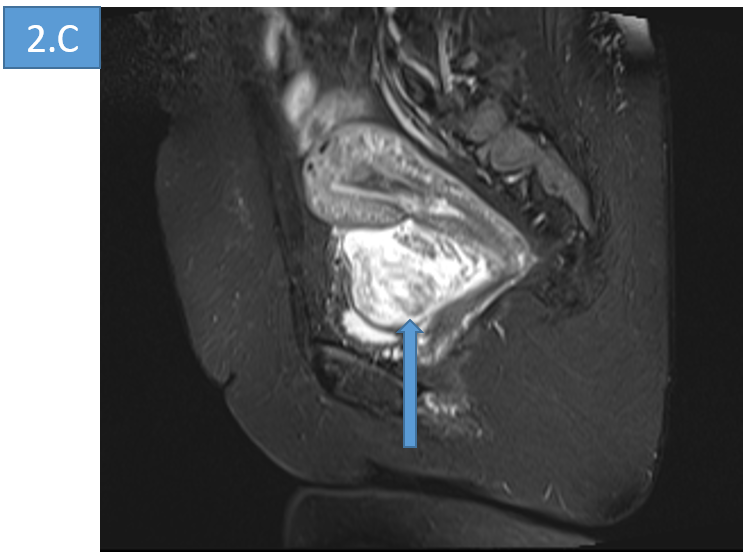
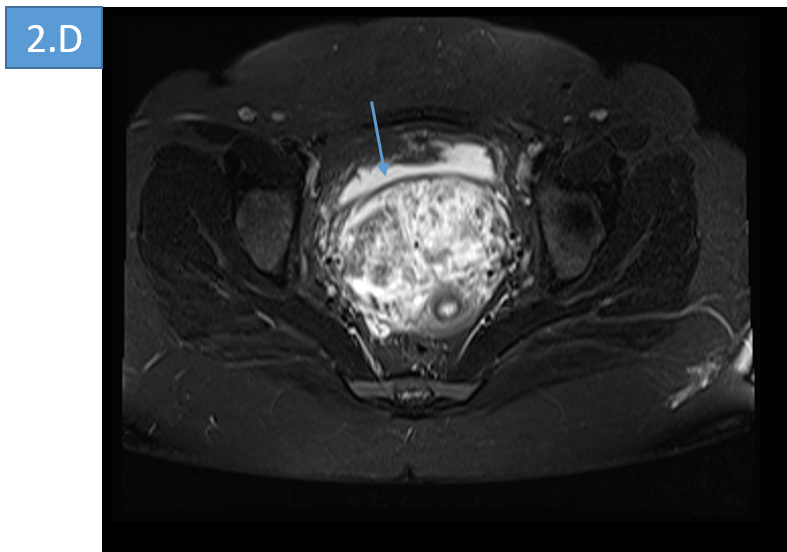
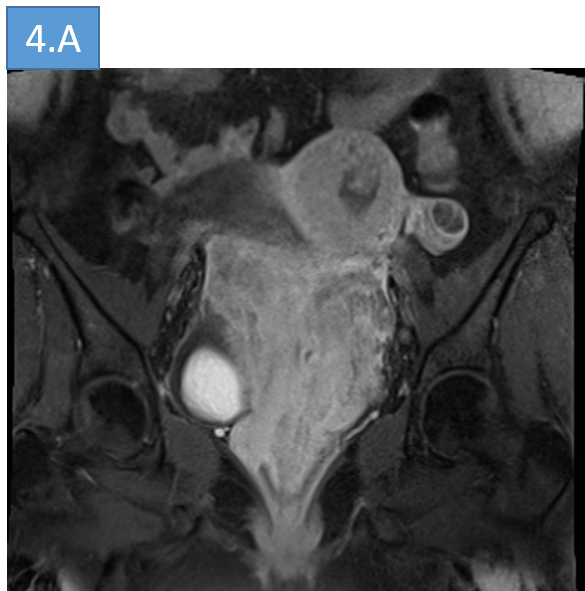
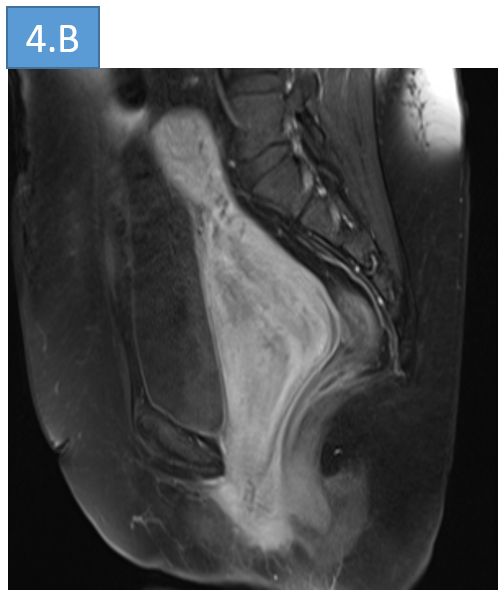
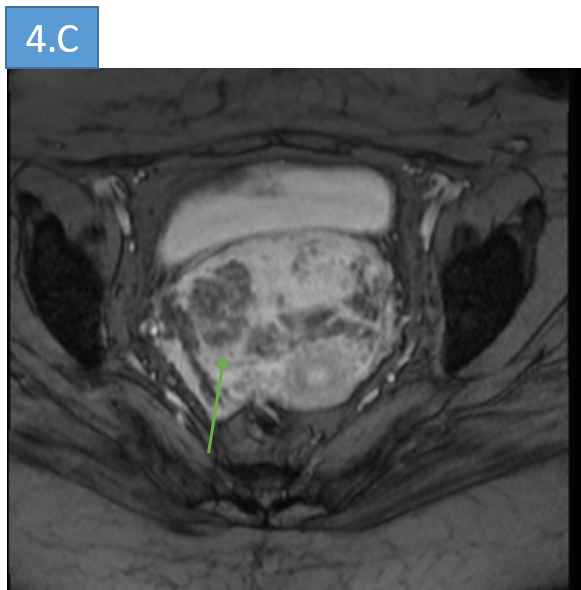
- 2: Axial (A) and sagittal (B) T2 imaging; Fat suppressed T2 axial (c) and sagittal (D)
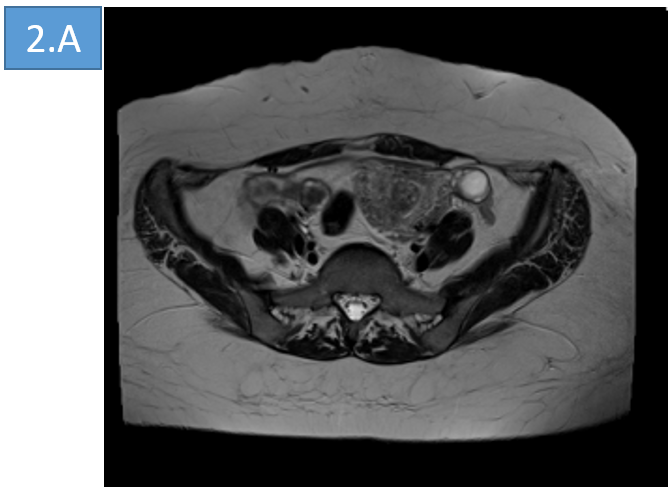
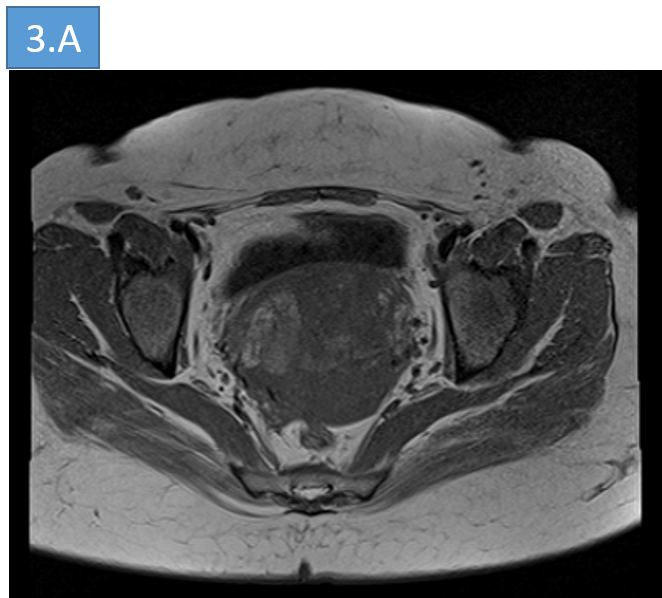
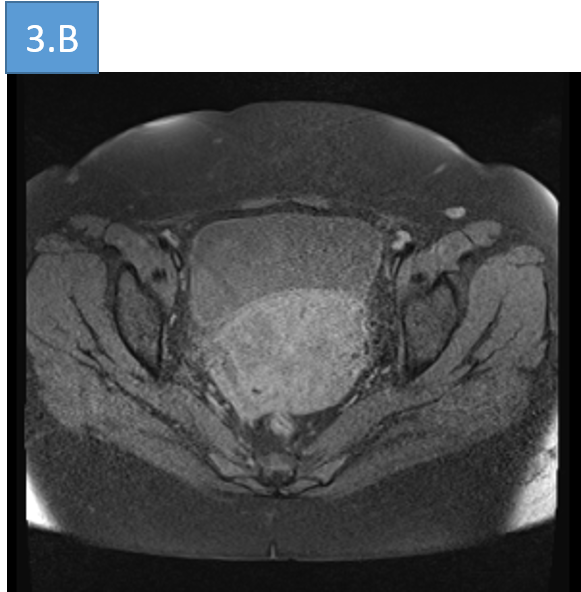
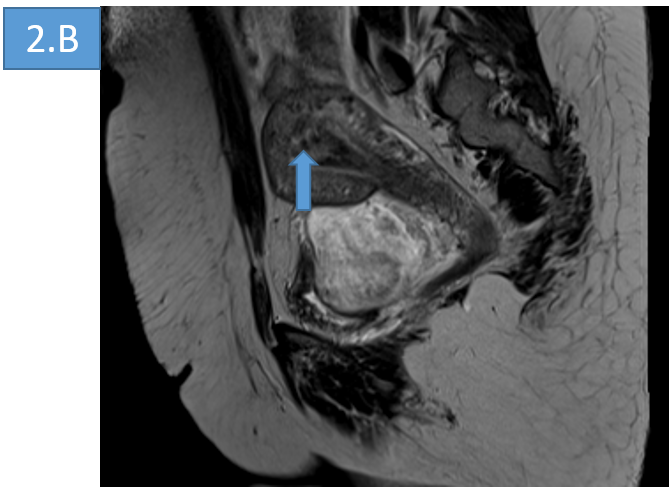
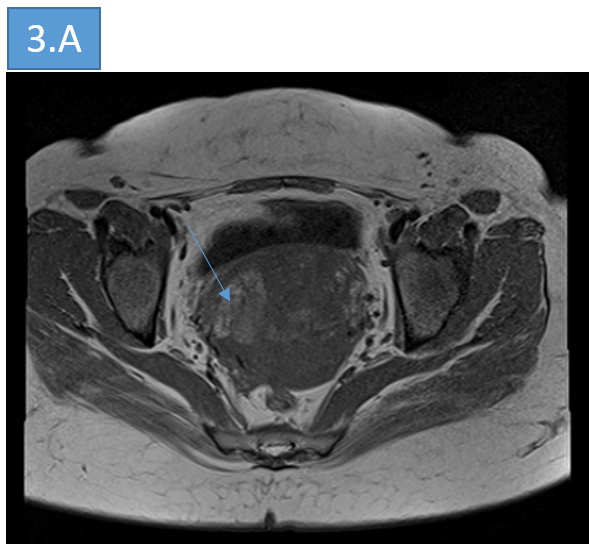
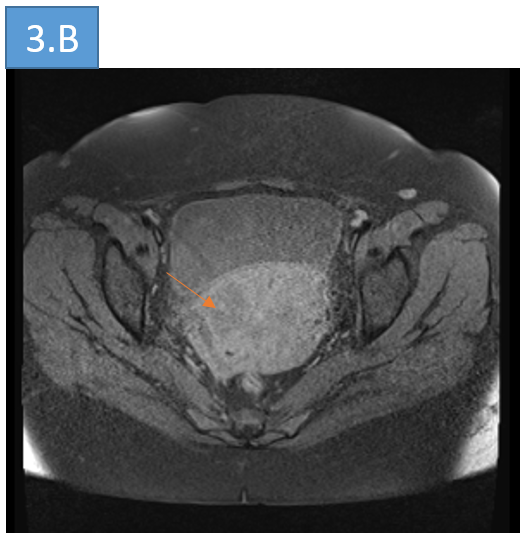
- 3: Axial T1 (A) and fat suppressed T1(B)
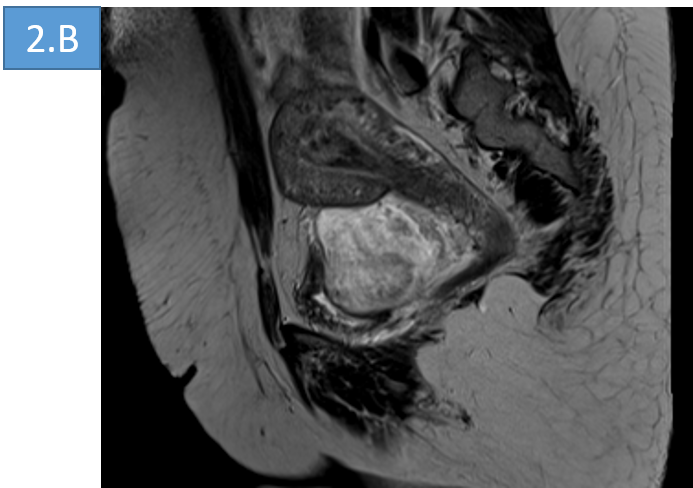
- 4: Post contrast coronal (A) and sagittal (B) images and GRE (C)
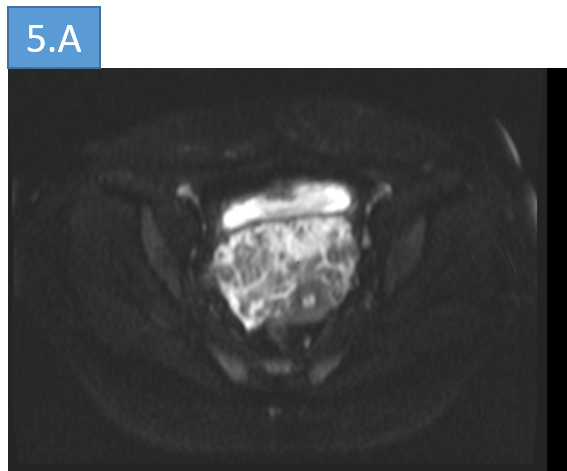
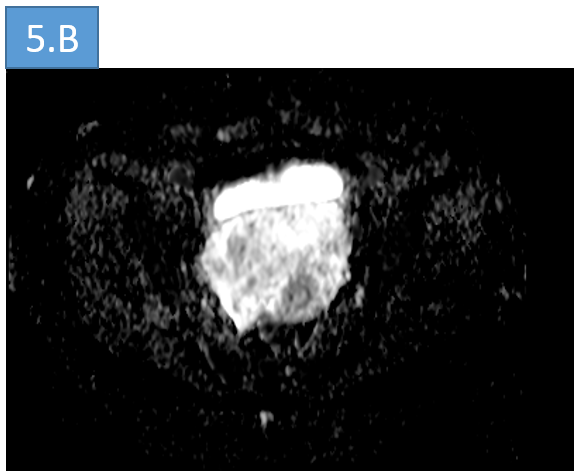
- 5: DWI AND ADC IMAGES
- 1.
- Endometrial thickness: 13.6 mm - thickened & hyperechoic with internal vascularity - suggestive of retained products of conception (Green arrow).
- Fairly defined hyperechoic areas (yellow arrow) with posterior acoustic shadowing;
- 2.
- Bilateral ovaries (orange arrow) appears normal. The endometrium shows heterogeneous T2 hypo intense contents - suggestive of retained products of conception (blue arrow).
- A large well circumscribed lobulated heterogeneous mass lesion (blue arrow) noted arising from anterior wall of vagina, extending exophytically between urinary bladder and vagina;
- The lesion appears heterogeneously hyper intense on STIR with swirled pattern, suggesting myxoid matrix.
- 3. The lesion appears iso intense (to muscle) on T1 with areas of hyper intensities (blue arrow) which suppress on fat saturated pre contrast T1 sequences (orange arrow), suggestive of fatty component
- 4. Coronal and sagittal post contrast study showing enhancement and areas of blooming on GRE (green arrow)
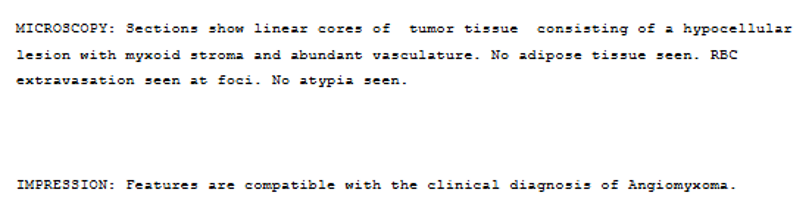
DIAGNOSIS:
- Angiomyxoma of the pelvis
- Retained products of conception.
DISCUSSION :
- Angiomyxoma is a slow growing mesenchymal tumour. It affects women of reproductive age and usually involves the deep soft tissues of the vulvovaginal region, pelvis and perineum of women as well as the inguinoscrotal region in men (less likely).
- It is essentially a benign tumor and the term "aggressive" is due to a predilection for local recurrence. Only rarely does it metastasize.
Imaging:
Transvaginal sonography (US):
- There is no specific feature,
- The key findings are:
- Localisation (usually paravaginal, paracervical or pelvic)
- Tubular/fusiform morphology
- Lipoma-like appearance
- Doppler: Internal vascularization
CT findings:
- A mass hypodense or isodense to muscle
- Well-defined margins
- Variable contrast enhancement
MRI findings:
- High signal intensity on T2WI (myxoid stroma)
- Swirled/laminated appearance: hypointense strands of fibrovascular tissue.
- Contrast enhanced sequences: progressive and heterogeneous enhancement.
- Mild restriction on DWI with characteristic high mean values in ADC maps.
- MR report should include precise anatomical description (relationship with the vagina, urethra, anal sphincter, rectum or extension above/below pelvic diaphragm) when describing these tumours.
TREATMENT :
- Wide surgical resection (complete excision) is the treatment of choice. Incomplete resection is considered acceptable if followed by long-term follow-up.
- Most of these tumours show oestrogen and progesterone receptor positivity. Hormonal treatment is thought to be a viable treatment as well as an interesting option for pre-operative shrinking of these tumours.
- High rate of local recurrence in the first years after surgery (more than 35% of patients).
Differential Diagnosis:
- Myxoma
- Myxoid lipoma
- Myxoid liposarcoma
Reference :
- Surabhi VR, Garg N, Frumovitz M, Bhosale P, Prasad SR, Meis JM (2014) Aggressive Angiomyxomas: A Comprehensive Imaging Review With Clinical and Histopathologic Correlation. AJR Am J Roentgenol Jun;202(6):1171-8 (PMID: 24848813)
- Miguez Gonzalez , Dominguez Oronoz R, Lozano Arranz P, Calaf Forn F, Barrios Sanchez P, Garcia Jimenez A. (2015) Aggressive Angiomyxoma: Imaging Findings in 3 Cases With Clinicopathological Correlation and Review of the Literature. J Comput Assist Tomogr Nov-Dec;39(6):914-21 (PMID: 26529675)
- Sun Y, Zhu L, Chang X, Chen J, Lang J. (2016) Clinicopathological Features and Treatment Analysis of Rare Aggressive Angiomyxoma of the Female Pelvis and Perineum - a Retrospective Study. Pathol Oncol Res Aug 29 (PMID: 27571990)
Dr Rashmi M N
MBBS, DMRD, DNB
Senior Consultant Manipal Hospitals Radiology Group Mysore.
Dr Sanjana.N
MBBS, M.D.
Cross section imaging fellow - MHRG