A 75-year-old female with a history of dyspnoea and intermittent fever
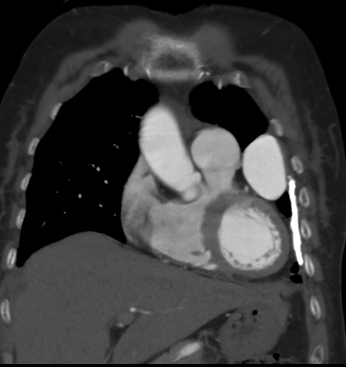
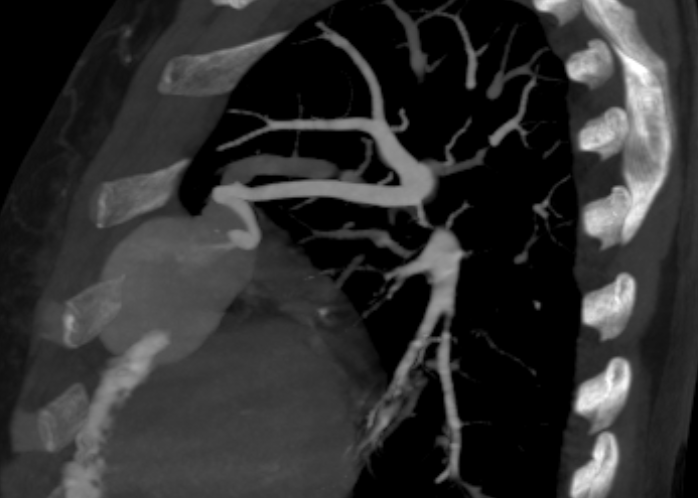
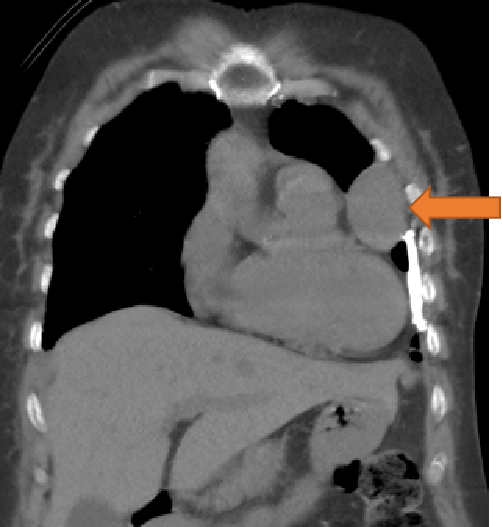
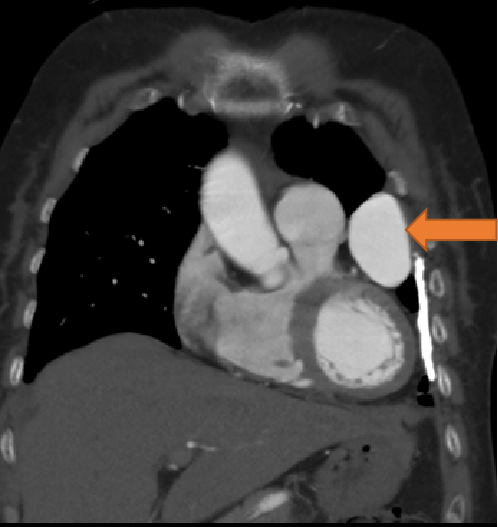
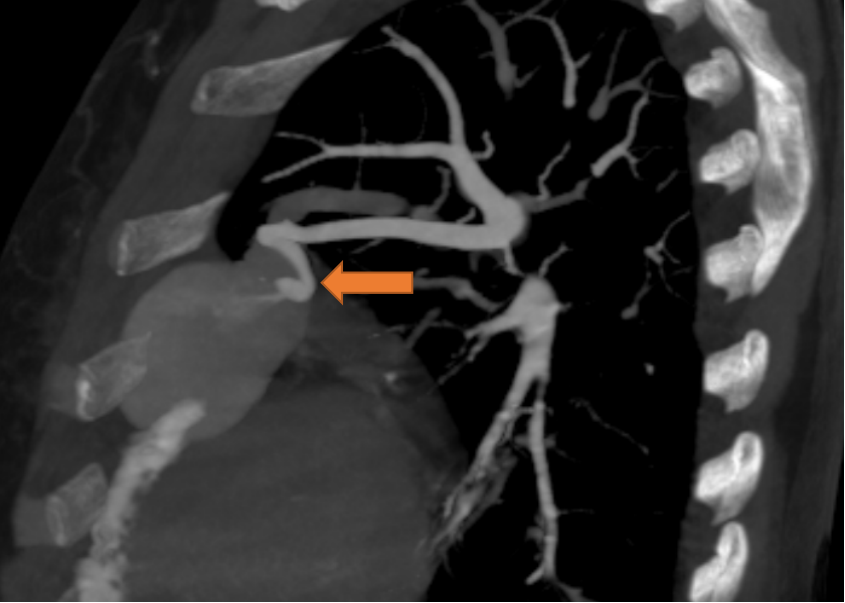
- Well defined mass lesion with smooth margin in the lingular segment of left upper lobe abutting the mediastinal and coastal pleura showing progressive enhancement.
- Engorged tortuous branch from left pulmonary artery supplying the lesion.
DIAGNOSIS
- Pulmonary arteriovenous Malformation
DISCUSSION
Pulmonary arteriovenous malformations (PAVMs) are uncommon and predominantly congenital in nature. They are direct fistulous connections between pulmonary arteries and pulmonary veins. PAVMs bypass the normal pulmonary capillary bed resulting in a right-to-left shunt. A nidus is usually present.
Although the majority of patients with PAVMs are asymptomatic, undiagnosed patients can present later in life with serious complications such as paradoxical embolism, stroke, myocardial infarction, cerebral abscesses, and massive hemoptysis.
PAVMs can be classified into three types:
- Simple type: commonest, up to 80%, with a single segmental artery feeding the malformation
- Complex type: with multiple segmental feeding arteries
- Diffuse type: rare, with hundreds of malformations
- Approximately 80% of PAVMs are associated with hereditary hemorrhagic telangiectasia (HHT). Conversely, 50% of patients with HHT have PAVMs, which are often multiple in nature.
- Catheter pulmonary angiogram is the gold standard diagnostic modality. It is prudent to obtain a prior CT pulmonary angiogram in order to vessel map for the purposes of treatment planning.
- Embolization is recommended for asymptomatic patients in view of the complications related to right-to-left shunts, such as paradoxical emboli, as well as to improve oxygenation and effort tolerance.
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) recommends treatment for PAVMs if any one of three criteria is met:
- Any PAVM (solitary or multiple) with a feeding artery that is 2 mm or larger;
- Measurable increase in the size of the PAVM;
- Paradoxical emboli or symptomatic hypoxemia.
- Embolization is the preferred treatment given its high success rate.
Surgical treatment is generally reserved for cases involving:
- Diffuse lobar or segmental PAVMs
- Complex PAVMs not amenable to embolization
- PAVMs with large feeding arteries not amenable to embolization
- Patients with contraindication to iodinated contrast medium
Reference:
- Yap CW, Wee BB, Yee SY, Tiong V, Chua YX, Teo L, Lohan R, Tan A, Singh P, Rajendran PC, Yang C. The Role of Interventional Radiology in the Diagnosis and Treatment of Pulmonary Arteriovenous Malformations. Journal of Clinical Medicine. 2022 Oct 25;11(21):6282.
- Lee HN, Hyun D. Pulmonary arteriovenous malformation and its vascular mimickers. Korean Journal of Radiology. 2022 Feb;23(2):202.
DR PRAVIN KUMAR M
CONSULTANT RADIOLOGIST
MANIPAL HOSPITALS, BENGALURU.
DR VIKAS H P
DNB RESIDENT
MANIPAL HOSPITALS, BENGALURU.