A 68 year old, female presented with complaints of decreased salivation and painless facial swelling (bilateral cheek region)
FINDINGS:
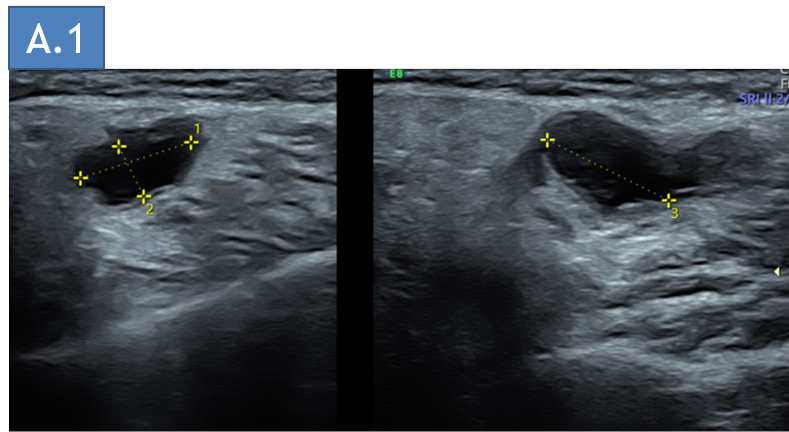
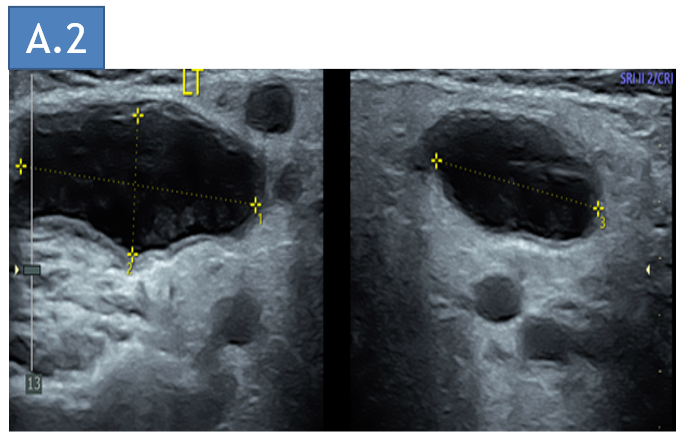
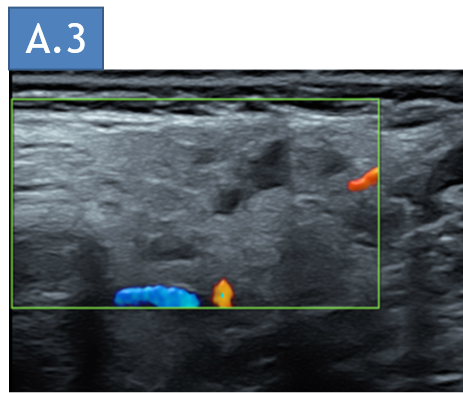
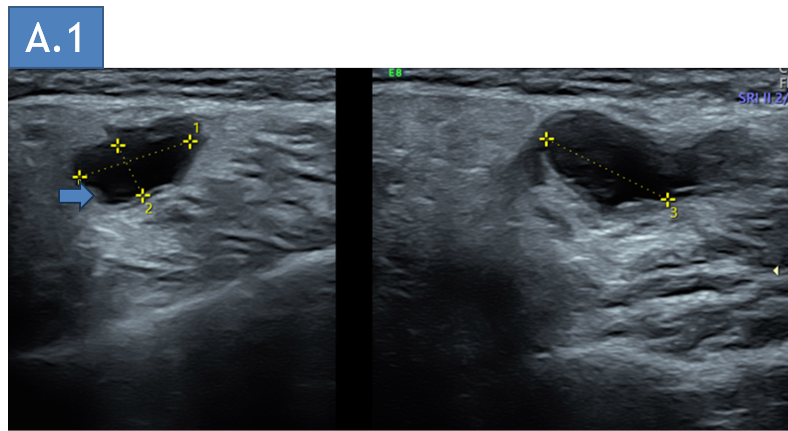
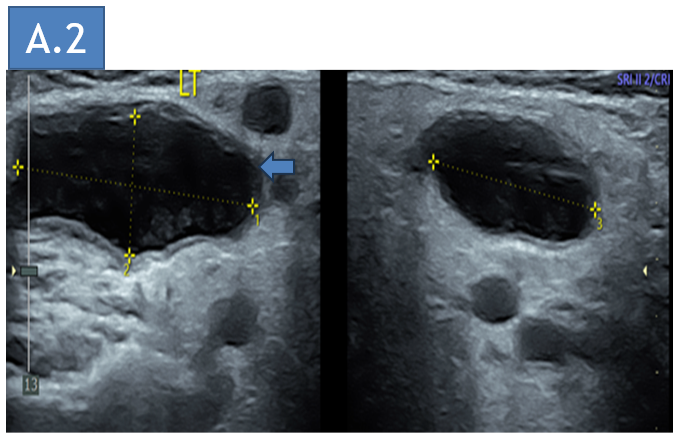
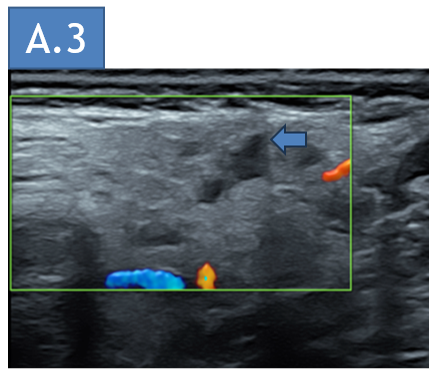
- A. USG Neck – Right and left parotid glands
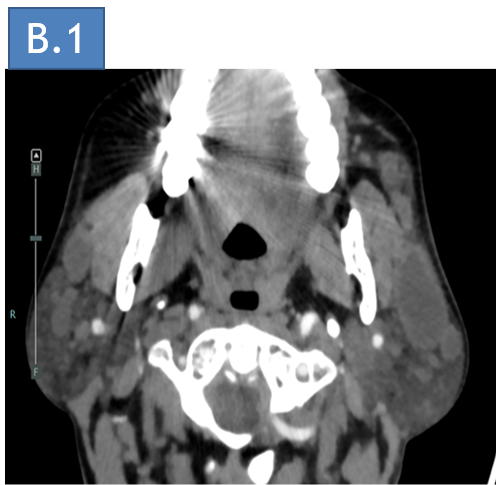
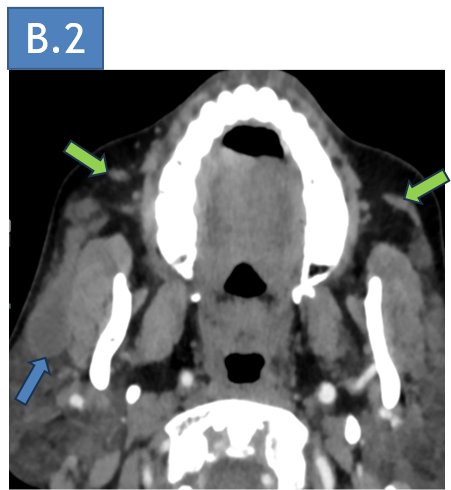
- B. CECT Neck: axial and coronal images at the level of parotid glands
- A. USG Neck – visualized right and left parotid glands show multiple intra-parenchymal cystic spaces within the glands.
- B. CECT Neck, axial and coronal images at the level bilateral parotid glands, show marked dilatation of the proximal parotid ducts (Blue arrow). Few other small cystic areas in bilateral parotid glands (Yellow arrow). The extra-parotid/ distal parotid ducts are normal in caliber with mild apparent wall thickening (Green arrow).
DIAGNOSIS:
- Giant sialectasis of bilateral parotid ducts with small sialoceles in bilateral parotid glands.
DISCUSSION:
- Bilateral dilatation (sialectasis) of the main parotid ducts is very rare. It is associated with ascending infections and gland destruction.
- The most common cause is duct obstruction by sialolith.
- Etiology: idiopathic, Sjogren syndrome, post-infectious, recurrent sialadenitis, salivary duct strictures, congenital (rare).
- Imaging has an important role in excluding differential diagnosis and potential complications (sialoliths and/or infection).
IMAGING :
- Ultrasound, CT or MRI can all be used to evaluate the parotid glands’ parenchyma, the dilated ducts, and to assess the cause of obstruction.
- CT is indicated to map lithiasis and if complications (abscess or tumour) are suspected.
- MRI, particularly MR sialography, has the advantage of being a non-invasive technique that does not use ionizing radiation and can better characterize duct morphology and stenosis.
- Sialogram: useful to identify stones - best definition of intraductal architecture; occasionally proves therapeutic as well as diagnostic (duct dilation, 'flushing out gland’).
- Imaging techniques can confirm the final diagnosis by demonstrating bilaterally dilated Stensen’s ducts with smooth margins, an absence of obstructive causes, and normal parotid gland parenchyma.
- Therapeutic options include conservative measures in the initial phase - regularly milking the swelling; good oral hygiene; hydration.
- Catheterization and Ostia enlargement/stenting and ultimately Surgical management such as duct dilatation or incision maybe considered.
- Being a rare condition, no treatment has proven effective.
Dr. Ashwini C
Consultant Radiologist
Department of Radiology
Manipal hospital, Hebbal.
Dr. C. Vaishali Raj
Cross Section Fellow
Manipal hospital, Yeshwanthpur.