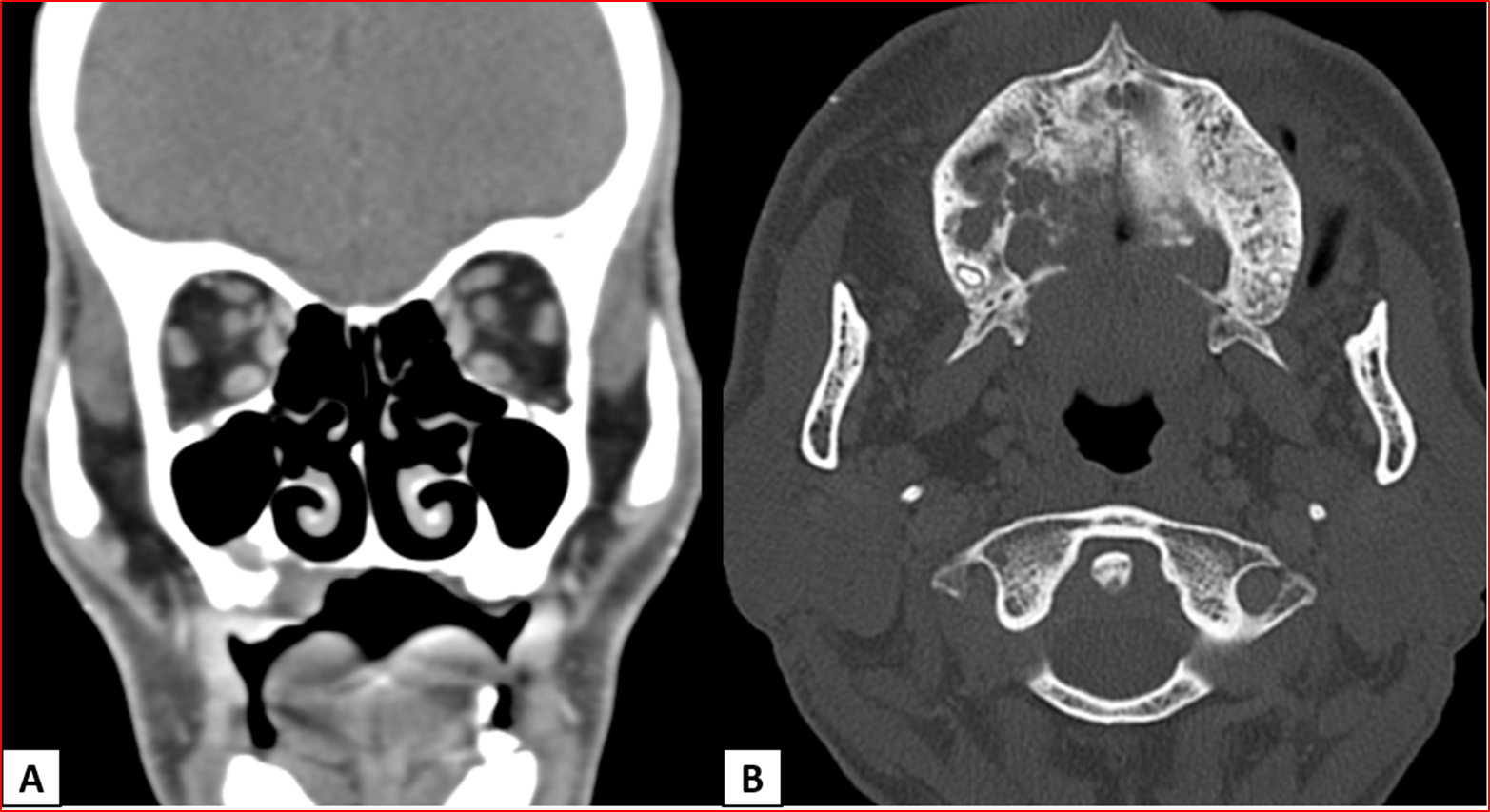
A 65-year-old with the history of right upper alveolus ulcer.
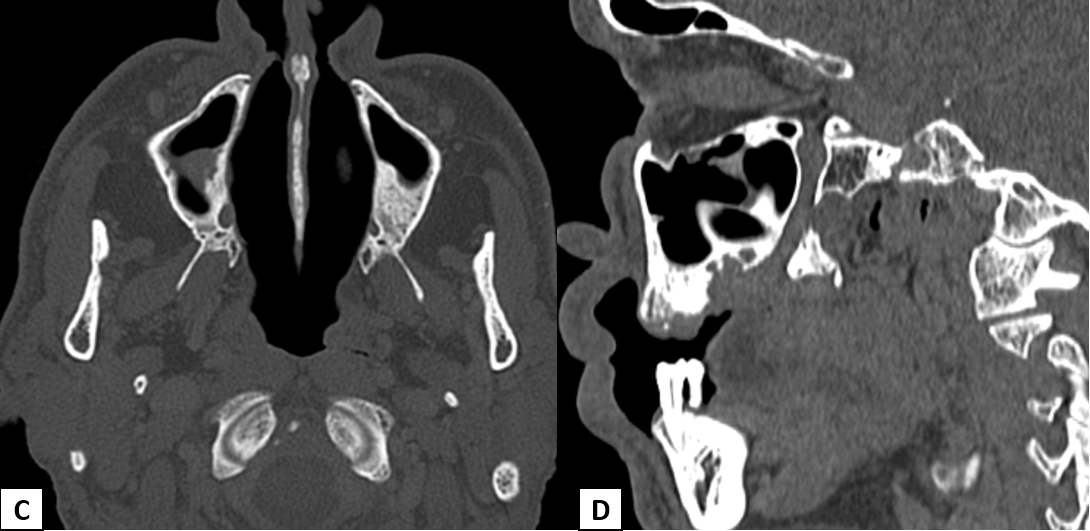
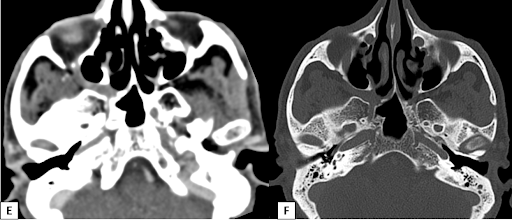
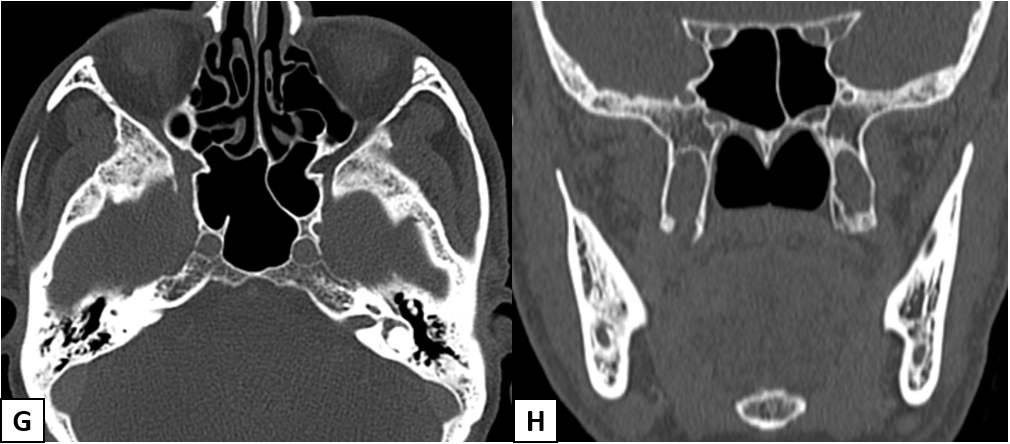
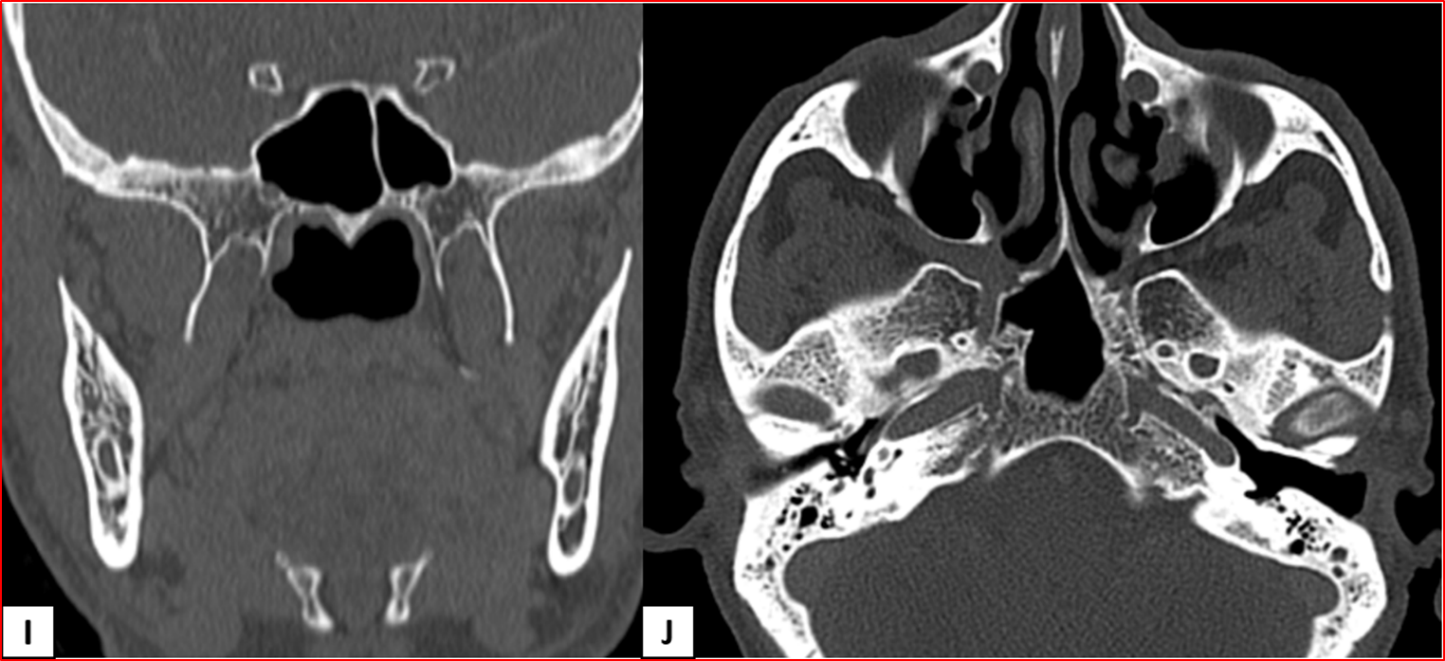
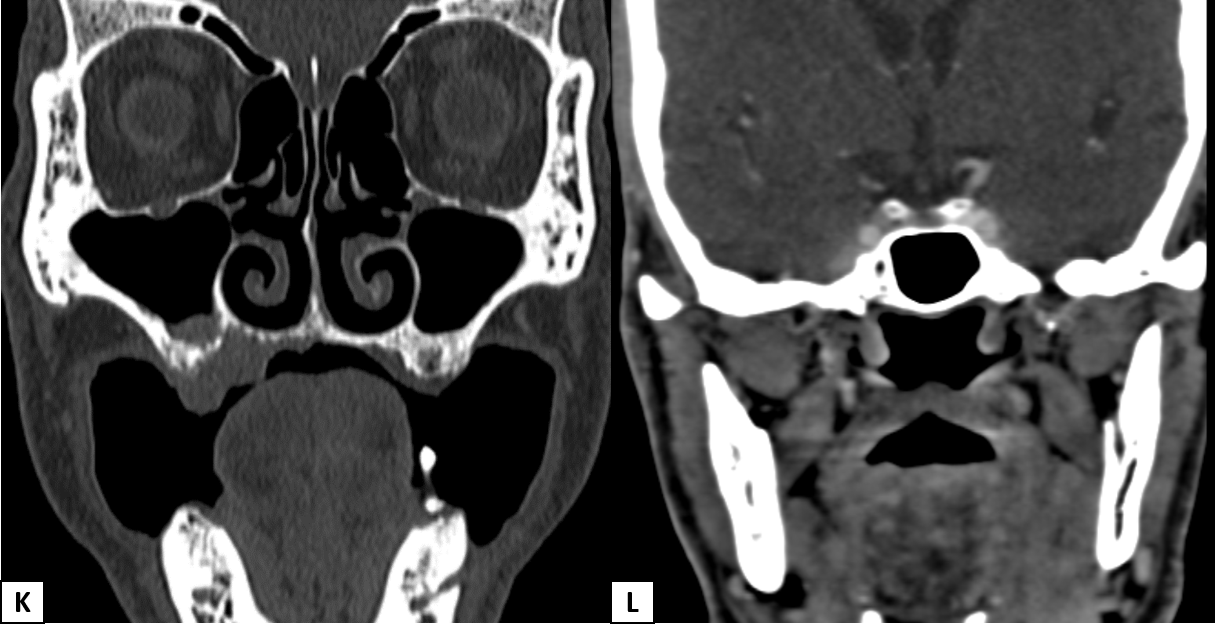
- Heterogeneously enhancing destructive mass lesion centered at right superior maxillary alveolus with involvement of ipsilateral superior gingiva-buccal sulcus and hard palate.
- Smooth widening of the right greater palatine foramen. Enhancing soft tissue thickening with the widening of the right pterygopalatine fossa (PPF).
- Smooth expansion of the right vidian canal, foramen rotundum, and infraorbital canal with enhancing soft tissue in the inferior aspect of the right cavernous sinus.
DIAGNOSIS:
Right maxillary alveolus carcinoma with perineural spread along V2 and its branches.
DISCUSSION:
Head and neck malignancies showing propensity for perineural spread include:
- Squamous cell carcinoma.
- Adenoid cystic carcinoma.
- Malignant desmoplastic melanoma.
- Basal cell and adenocarcinoma.
Modalities for diagnosis:
- CT has low sensitivity. Bony foramina better evaluated.
- MRI is the preferred modality due to superior soft tissue contrast.
- Gadolinium-MR makes the diagnosis by showing enlargement and abnormal contrast enhancement, which cannot be depicted with CT.
Indicators of perineural spread:
- Effacement of perineural, foraminal and/or juxtaforminal fat
- Asymmetric nerve or foraminal enlargement
- Asymmetric, irregular or nodular nerve enhancement
- Secondary features of denervation injury including acute edema and chronic atrophy.
Key anatomic landmarks:
- V1: Supraorbital foramen.
- V2: Infraorbital foramen, pterygopalatine fossa, vidian canal, foramen rotundum, greater and lesser palatine foramen (As in our case).
- V3: Mental foramen, mandibular canal, mandibular foramen, foramen ovale.
- Geniculate ganglion: Enlargement and obliteration of the geniculate fossa.
- Facial nerve: Mastoid segment and stylomastoid foramen.
- Hypoglossal nerve: Hypoglossal canal.
- Perineural spread of malignancy is a potential and important route of spread of head and neck malignancies; its presence indicates a poor prognosis. Perineural spread often has tumor recurrence and poor long-term survival.
- A checklist approach and thorough inspection of potential sites on contrast-enhanced fat-suppressed images should be routinely undertaken.
- Presence of focal neurological deficits and cranial nerve palsies in patients with head and neck malignancies should prompt a detailed search to exclude perineal spread of malignancy.
Differential diagnosis:
- Primary neural tumours such as schwannomas.
- Invasive fungal infections such as aspergillosis or mucormysosis (in severely immunocompromised individuals).
- Meningeal inflammatory disorders such as sarcoidosis or histiocytosis.
REFERENCES:
- Perineural spread of malignant head and neck tumors: a review of the literature and analysis of cases treated at a teaching hospital. Mauro César Silveira Moreira, Antonio Carlos dos Santos, Murilo Bicudo Cintra. Radiol Bras. 2017 Sep-Oct; 50(5): 323–327.
- Perineural Tumor Spread in Head and Neck Malignancies, Seminars in Roentgenology, Volume 54, Issue 3, 2019, Mohit Agarwal, Pattana Wangaryattawanich, Tanya J. Rath.
- Perineural spread in head and neck malignancies, Radiation Medicine volume 24, pages1–8(2006). Ojiri, H.
- Ong CK, Chong VH. Imaging of perineural spread in head and neck tumors. Cancer Imaging. 2010;10(1A):S92.
Dr. Bhupendar Singh
Radiology Resident,
Manipal Hospitals Radiology Group
Dr. Anita Nagadi
MD, MRCPCH (UK), FRCR (UK), CCT (UK)
Senior Consultant Radiologist
Manipal Hospitals Radiology Group.