A 51-year-old lady (Para 2, Living 2) with history of hysterectomy and left salpingo
FINDINGS:
- oophorectomy was found to have a large pelvic cyst on ultrasound.
- CA – 125 and CEA levels were within normal limits.
- Contrast enhanced MRI Pelvis was performed.
IMAGES :
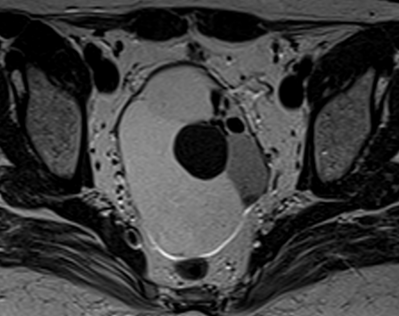
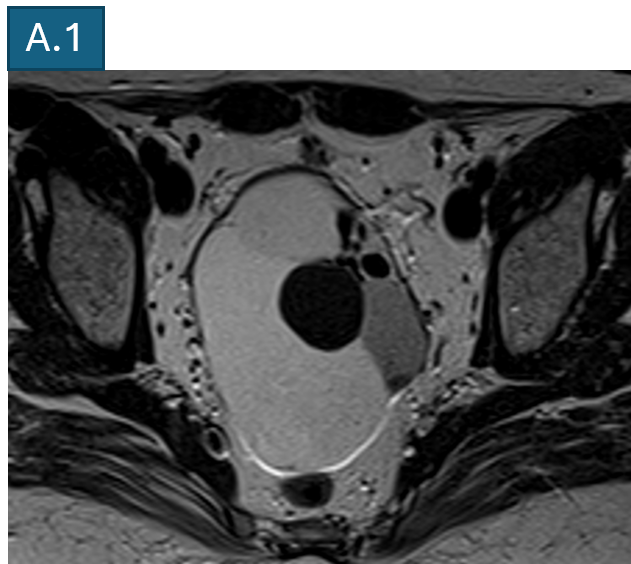
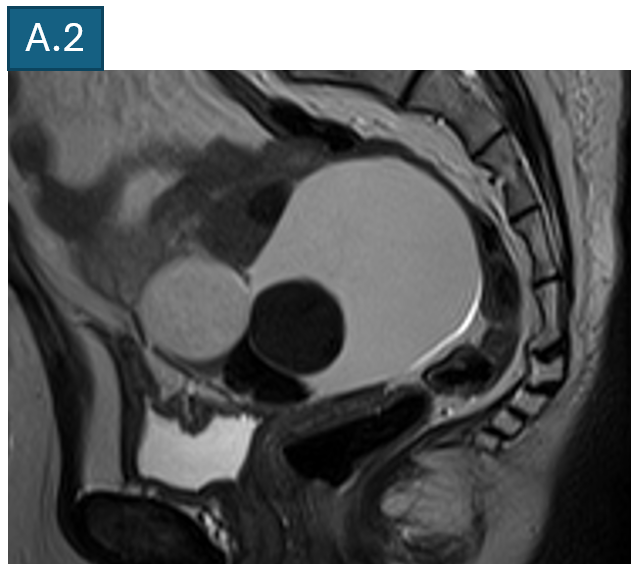
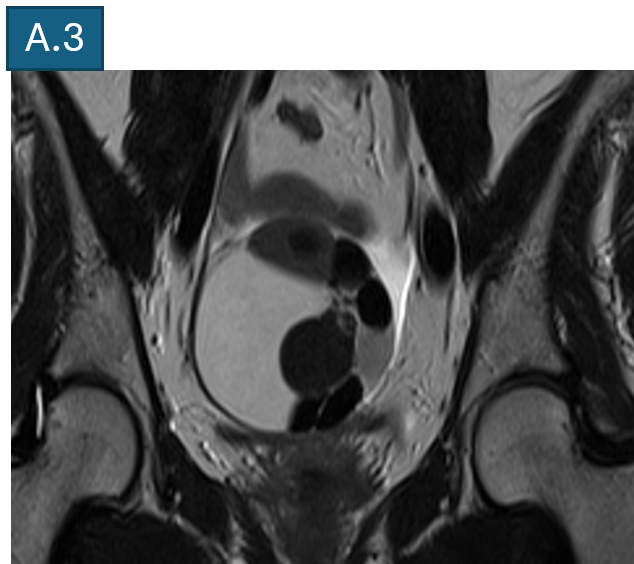
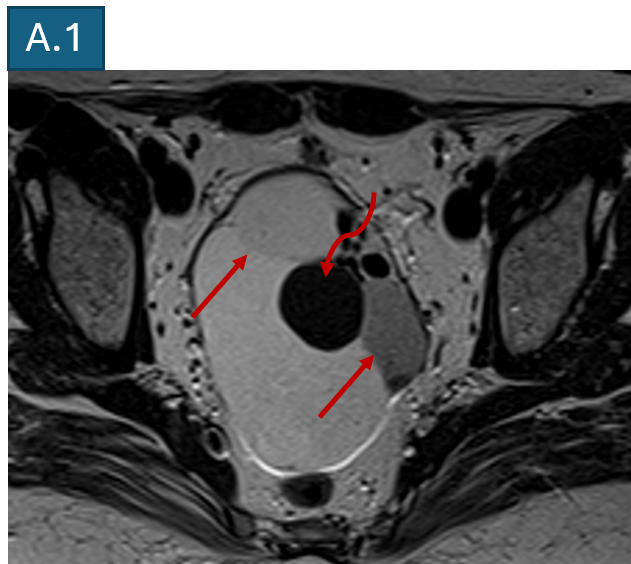
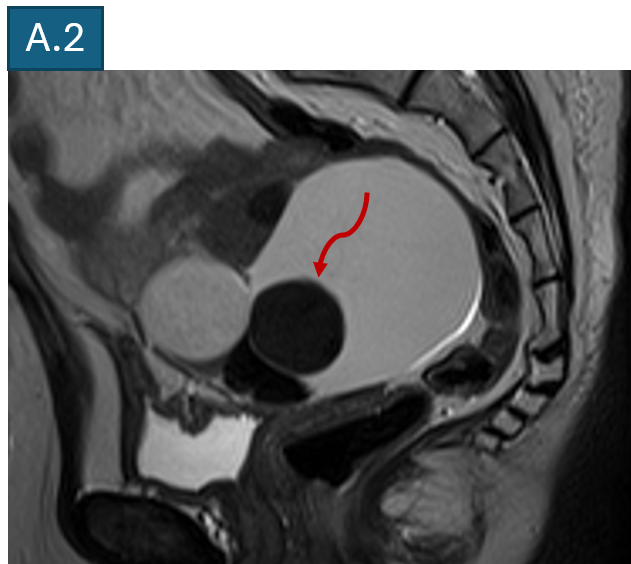
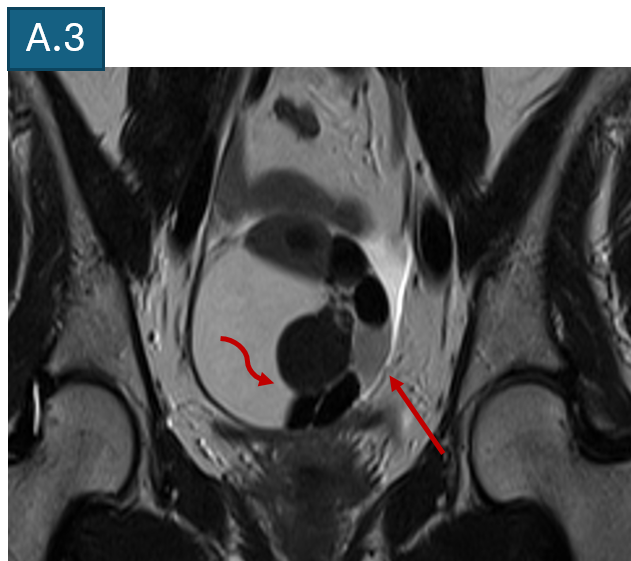
- A : T2 TSE axial, sagittal and coronal images.
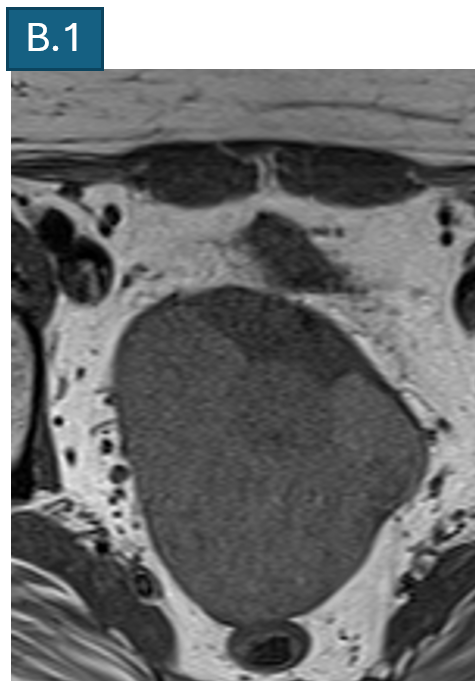
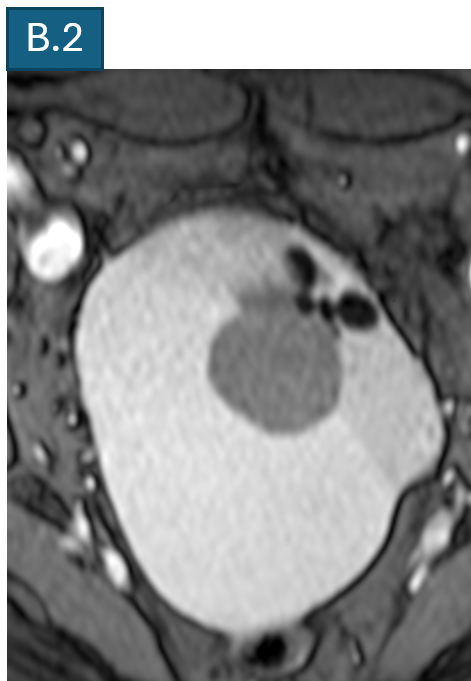
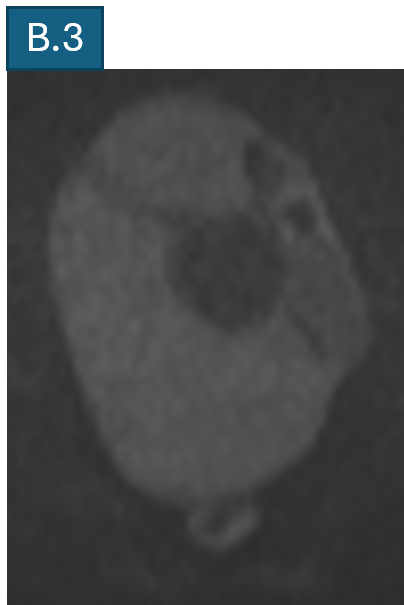
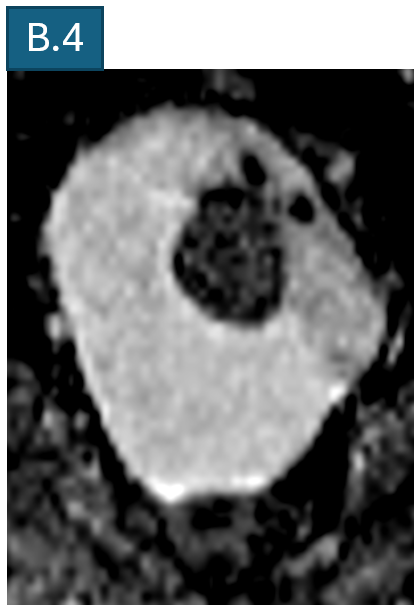
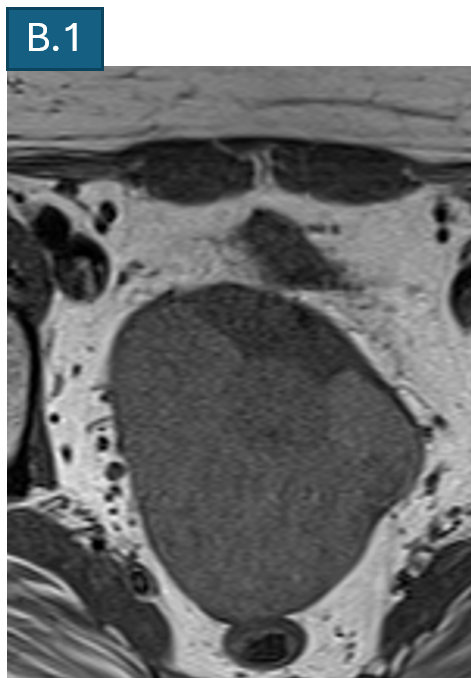
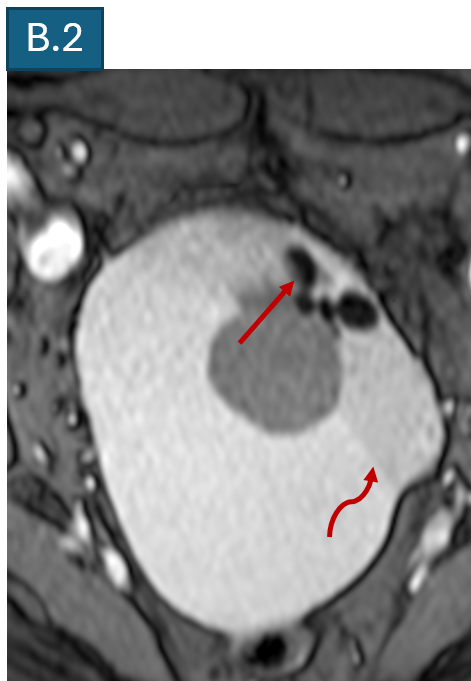
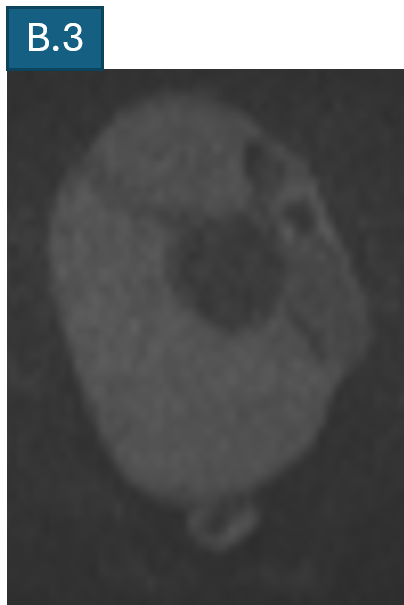
- B : Axial T1 TSE, T2 GRE, DWI and ADC images.
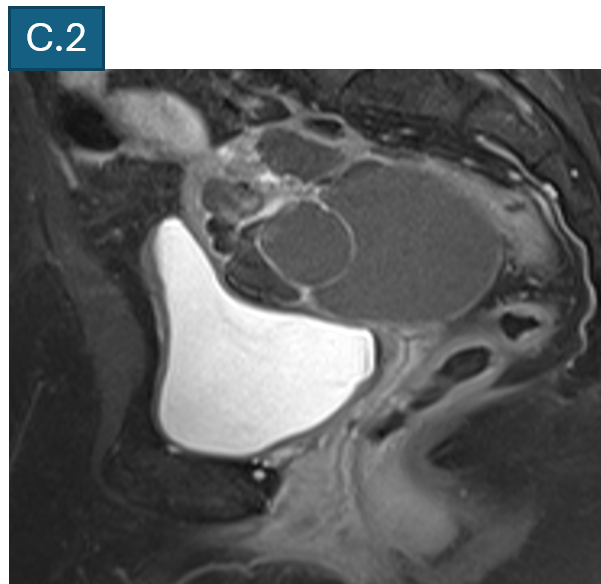
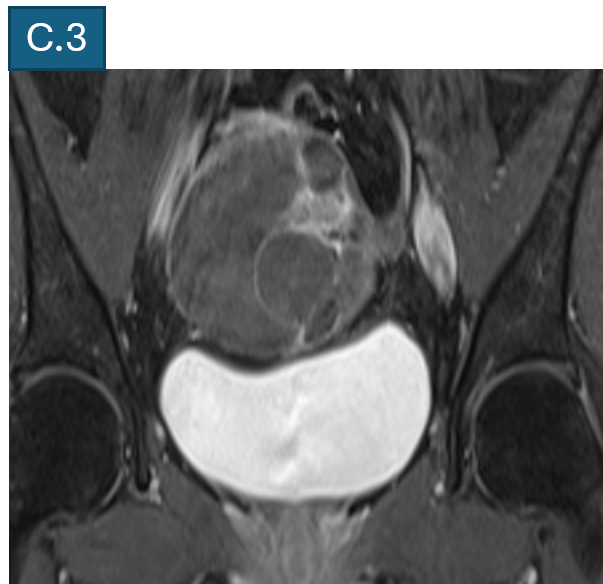
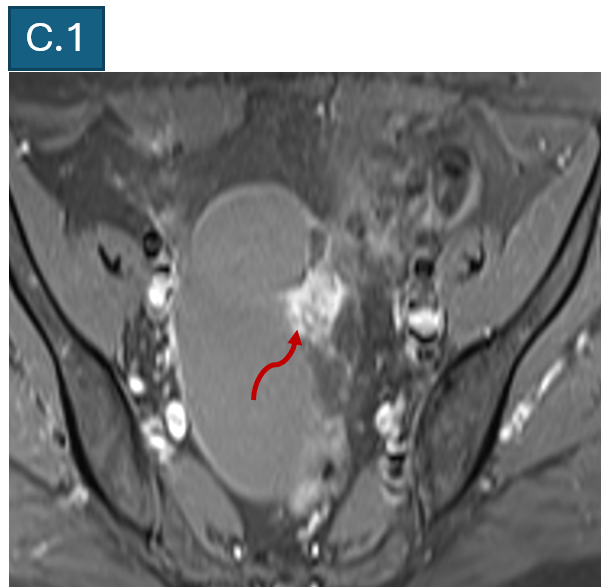
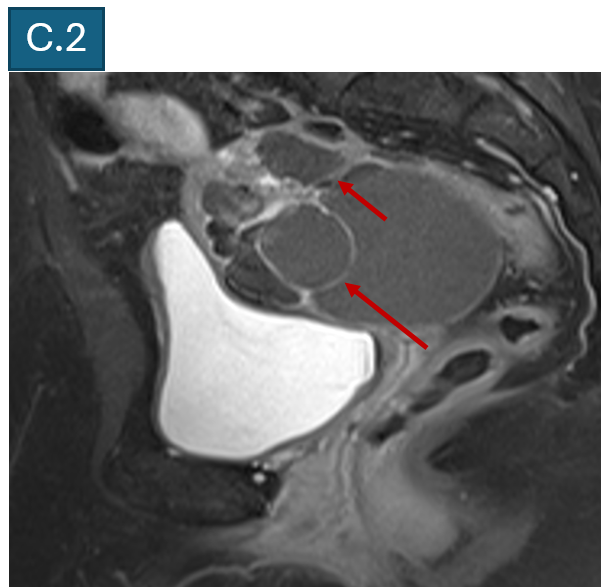
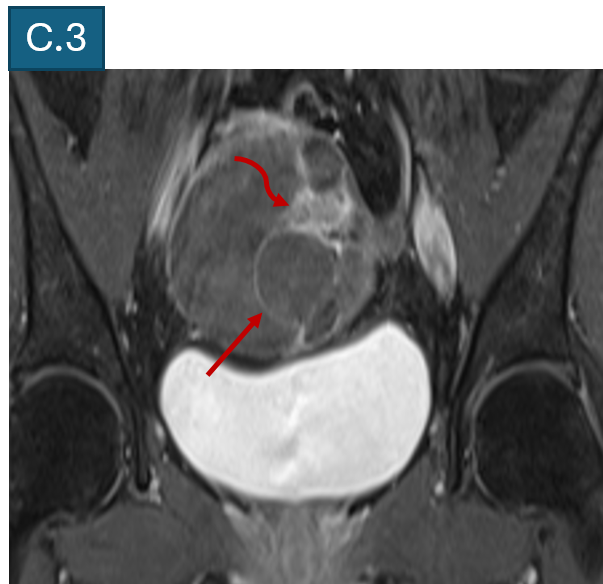
- C : T1FS axial, sagittal and coronal post contrast images.
- A: A large, multiloculated cyst in the pelvis, measuring 9.6 x 7.3 x 6.2 cm showing predominantly T2 hyperintense signal while few of the locules demonstrate T2 shading (straight arrow) and T2 hypointense signal (curved arrow).
- B: The lesion demonstrates hyperintense T1 signal with few of the locules demonstrate blooming foci (straight arrow), suggestive of blood products. No diffusion restricting area within. T2 shading noted (curved arrow).
- C: The lesion demonstrates enhancement of internal septae (straight arrow) on post contrast images and an enhancing nodular (curved arrow) area, measuring 2.1 x 1.7 x 1 cm.
- D: Trace free fluid seen in pelvis.
- E: No significant lymphadenopathy seen.
DIAGNOSIS:
IMAGING IMPRESSION:
- A multiloculated partially haemorrhagic multiloculated cystic mass in the pelvis, demonstrating enhancing septations, solid enhancing area and other features as described - O-RADS MRI 4 (~ 50%; intermediate risk)
FINAL DIAGNOSIS:
- Patient underwent right salpingo – oophorectomy.
- Final histopathology showed an abundance of mature thyroid follicles intermixed with smooth muscle and epithelial tissue (squamous, cartilage, bronchial) and was suggestive of Mature cystic teratoma/ struma ovarii without any evidence of immature neuro epithelium or malignancy.
DISCUSSION:
INTRODUCTION:
- Struma ovarii is a mature ovarian teratoma composed entirely or predominantly (>50%) of thyroid-tissue components. It constitutes 0.3 to 1% of all ovarian tumours and is the most common type of mesenchymal teratoma.
- They are commonly seen in middle aged females, with a peak incidence in 5th decade.
- Most cases are asymptomatic and incidentally detected. Hyperthyroidism occurs in 5%- 8% of patients. They have been associated with increased CA 125 levels.
- Imaging findings of struma ovarii may be atypical depending on the cyst size and concentration of the contents. Given the rarity of struma ovarii, atypical imaging features can sometimes be misleading.
- Majority (~95%) of struma ovarii are benign.
IMAGING:
- On ultrasound, struma ovarii usually manifests as non-specific heterogeneous multilocular cystic ovarian mass with solid components and septae. Ascites maybe present.
- On CT these lesions show a solid - cystic appearance usually demonstrate high attenuation on noncontrast images. This phenomenon is attributed to the thyroid follicles containing gelatinous colloid materials rich in thyroid hormones and iodine compounds.
- MRI is helpful in further characterization.
- On MRI the lesion usually appears as a unilateral multilocular mass with solid components and thick septations, resulting in a "lacy appearance".
- Heightened contrast enhancement is attributed to the presence of thyroid tissue, which thickens the septa or nodules.
- Signal intensity of struma ovarii varies based on the proportion of gelatinous colloid material containing thyroid hormones. The presence of hemorrhage, necrosis, or fibrosis within the cystic components may further influence the signal intensity of the cysts.
DIFFERENTIAL DIAGNOSIS AND CONCLUSION:
- The usual imaging differential diagnosis of struma ovarii include ovarian adenocarcinomas (serous, mucinous) and endometriomas.
- Although MR features of struma ovarii overlap with those of other epithelial ovarian lesions, when MR imaging shows a unilateral complex mass with thickened septa, is composed of multiple cysts of variable signal intensity (in keeping with thick viscous colloid fluid) and demonstrates intensely or moderately enhancing solid components with a “lace appearance”, struma ovarii should be included in the differential diagnosis with high probability.
TREATMENT:
- Benign struma ovarii typically have a good prognosis, and treatment necessitates excision with unilateral salpingo oophorectomy (with resultant fertility preservation).
- Malignant struma ovarii are less common, with no standardized treatment or well evaluated prognosis. Given the similarities with thyroid cancer, the general consensus is to treat malignant struma ovarii like thyroid cancer—with surgical tumor resection and adjuvant radioactive iodine therapy.
- Preoperative radiological imaging diagnosis of struma ovarii is important to avoid unnecessary surgery because 95% of struma ovarii are benign and occur in premenopausal women, although the MRI findings are similar to those of malignant ovarian tumors.
REFERENCES:
- Kaiji Inoue, Eri Hoshino, Taira Shiratori, Atsushi Sasaki, Takeshi Kajihara, Eito Kozawa, A large benign struma ovarii with atypical imaging findings, Radiology Case Reports, Volume 19, Issue 11, 2024, Pages 5447-5451, ISSN 1930-0433, https://doi?org/10?1016/j?radcr?2024?08?048.
- Dujardin MI, Sekhri P, Turnbull LW. Struma ovarii: role of imaging? Insights Imaging. 2014 Feb;5(1):41-51. doi: 10.1007/s13244-013-0303-3. Epub 2013 Dec 20. PMID: 24357453; PMCID: PMC3948908.
- https://eurorad.org/case/17177.
Dr Anita Nagadi
Senior Consultant Radiologist
MHRG, Manipal Hospital, Yeshwanthpur.
Dr Kanupriya Grover
Cross Sectional Imaging Fellow
MHRG, Manipal Hospital, Yeshwanthpur.