A 42 year old, male patient, presented with Fatigue, Blurring of vision, fever, weight loss , H/o Upper GI Bleeding (bleeding PR and hematemesis).
- Comorbidities: Splenomegaly with Mild Thrombocytopenia - ? Tropical Splenomegaly Syndrome, Iron Deficiency Anemia; Bilateral Optic Neuropathy
- Previous Surgeries - Nil
CECT Abdomen study
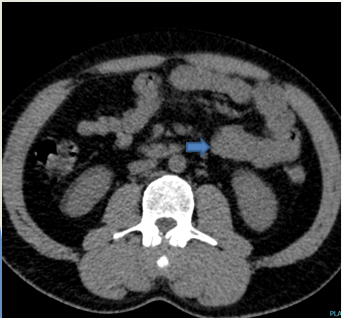
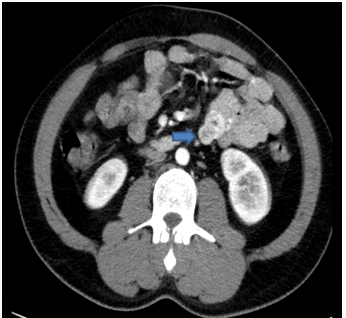
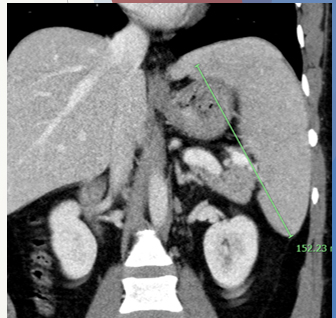
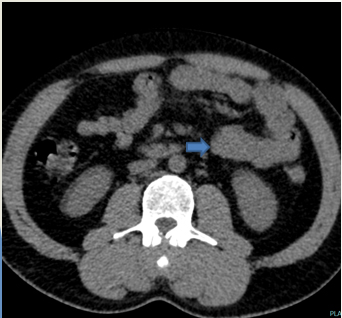
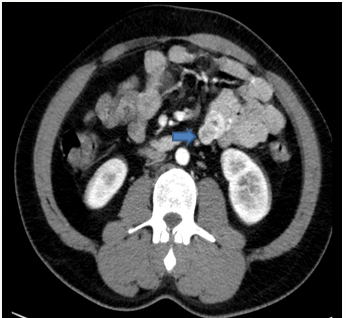
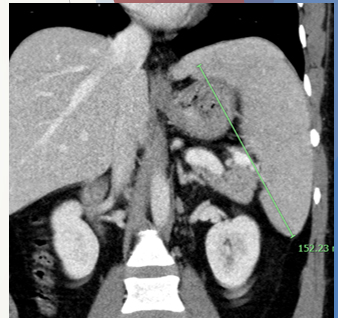
A. Axial and coronal images at the level of jejunal loops
A. LEGENDS
Axial and coronal images at the level of jejunal loops
A relatively well-defined, lobulated, isodense lesion on NCCT, showing heterogeneous post-contrast enhancement (blue arrow). The lesion measures 3.0 x 2.7 cm and is noted arising exophytically from the wall of the jejunal loop. The lesion shows few heterogeneously non-enhancing necrotic areas. There is also mild splenomegaly noted.
Diagnosis:
- SMALL BOWEL GASTRO-INTESTINAL STROMAL TUMOUR (GIST).
Discussion:
- Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors to arise from the gastrointestinal tract.
- They are characterized by expression of a tyrosine kinase growth factor receptor, also called kit receptor or CD117. This expression allows unchecked growth of tumor and resistance to apoptosis.
- The average patient with GIST is 40–70 years old.
- Male to female incidence is now considered to be equal.
- Despite being the most common mesenchymal tumor, GISTs only account for 1–3% of all gastrointestinal tumors.
- Stomach is considered to be the most common site, accounting for 60–70%. Approximately one-third occur in the small bowel, with rare occurrence in the colon and rectum (5%), esophagus (< 2%), and appendix. Some GISTs primarily arise in the omentum, mesentery, or retroperitoneum and are unrelated to the tubular gastrointestinal tract.
- Clinical presentation is often vague. Abdominal pain or distention is the most common presentation. Gastrointestinal bleeding or unexplained anemia is the next most common presentation. Duodenal tumors present with obstructive jaundice and may be confused with pancreatic cancer. Surprisingly, despite the large size of duodenal tumors, bowel obstruction is rare. The exophytic and cavitary nature of the tumor may delay luminal constriction.
Imaging
- Specific appearances will vary according to location and size, but in general, these tumors appear as rounded soft tissue masses, arising from the wall of a hollow viscus (most commonly the stomach) with an endoluminal or exophytic growth.
- The usual growth pattern in the small bowel is exoenteric, with a large extraluminal component.
- Small GISTS tend be round while larger GISTs tend to be lobulated. Bowel obstruction is rare even with large tumors.
- Mucosal ulceration is present in 50% of cases with large necrotic cavities communicating with the lumen also seen.
- Differentiating a benign from a malignant GIST radiologically is difficult. The diagnosis of malignant GIST requires histopathologic analysis, but certain characteristics suggest malignancy:
- exogastric growth
- diameter >5 cm
- Central Necrosis
- extension to other organs
Plain radiograph
When large, secondary signs of the tumor may be visualized by radiograph, e.g. soft tissue density displacing bowel loops.
Fluoroscopy
On Fluoroscopy, a filling defect projecting from the wall of the stomach/bowel loop may be seen, with overlying ulceration or cavitation. The tumor margins are normally seen as smooth and may form right or obtuse angles with the adjacent mucosa due to its intramural origin.
CT
- Typically the mass is of soft tissue density with central areas of lower density when necrosis is present (usually in larger tumors) that occasionally appear as fluid-fluid levels.
- They can show deep crescent-shaped ulceration demonstrating an internal air-fluid level - Toricelli- Bernoulli sign.
- Enhancement is typically peripheral (due to central necrosis). Calcification is uncommon.
MRI
The presence of necrosis, hemorrhagic and cystic change make appearances variable with small (<5 cm) and large (>5 cm) lesions have differing imaging characteristics:
- T1: low signal intensity solid component
- T2: high signal intensity solid component
- T1 C+: mild heterogeneous gradual enhancement in larger lesions and homogeneous strong arterial enhancement that persists in smaller lesions
- DWI/ADC: typical high DWI/low ADC signal; lower ADC values have been associated with high-risk tumors
Treatment:
- In the absence of metastatic disease, complete surgical excision is undertaken and offers the best hope of cure.
- GISTs ≥ 2 cm in size should be resected completely, and smaller GISTs (< 2 cm) may be endoscopically monitored every 6–12 months
- Unlike carcinomas, resection of GISTs does not require wide bowel excision. Lymphadenectomy is usually not required because these tumors do not show lymph node metastases.
- However, despite apparently complete resection with clear margins, the recurrence rate is high - may be partly due to tumor rupture leading to mesenteric implants; hence, the risk of recurrence emphasizes the importance of having meticulous surgical technique. For this reason, percutaneous biopsy is best avoided.
- The GIST Guideline Subcommittee in Japan recommends CT to be performed every 6–12 months for very low-, low-, and intermediate-risk GISTs and every 4–6 months for high-risk GISTs
Dr. Vikhyath Shetty
Consultant
Department of Radiology
Manipal hospital, Yeshwanthpur, Bengaluru
Dr. C. Vaishali Raj
Cross Section Fellow
Manipal hospital, Bengaluru