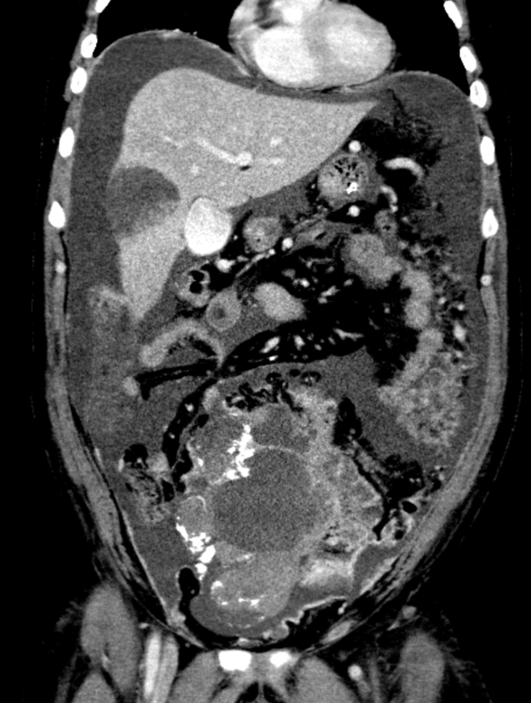
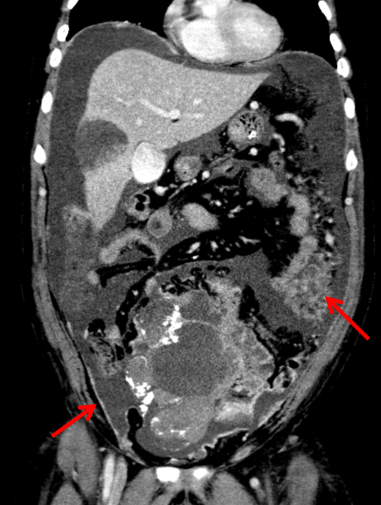
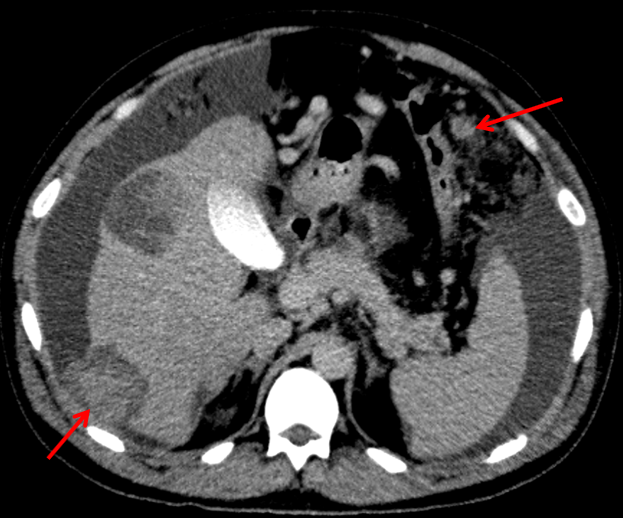
A 41 Year old gentleman with a large abdominopelvic mass and abdominal pain.
- Large solid cystic mass in the midline lower abdomen and pelvis, containing multiple clusters of curvilinear coarse calcification.
- Moderate ascites.
- Extensive omental caking and multiple large scattered peritoneal deposits and abnormal nodular peritoneal enhancement.
- Abnormal nodular enhancement along the surfaces of the small bowel suggests serosal deposits.
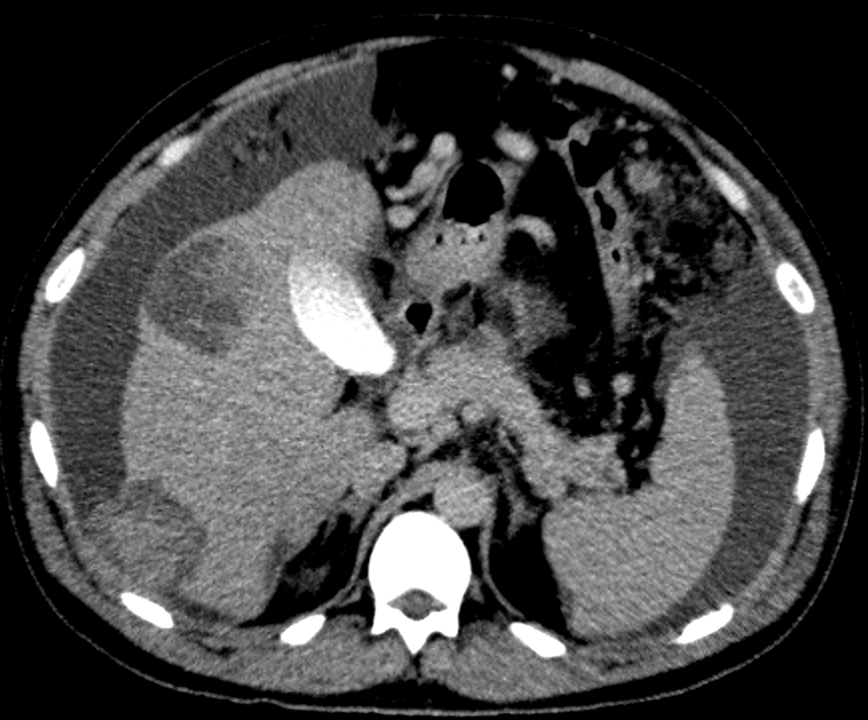
- Multiple scattered solid cystic abnormally enhancing lesions of varying sizes in the liver, compatible with hepatic metastases.
- The metastasis in segment VI demonstrates focal rupture into the perihepatic region.
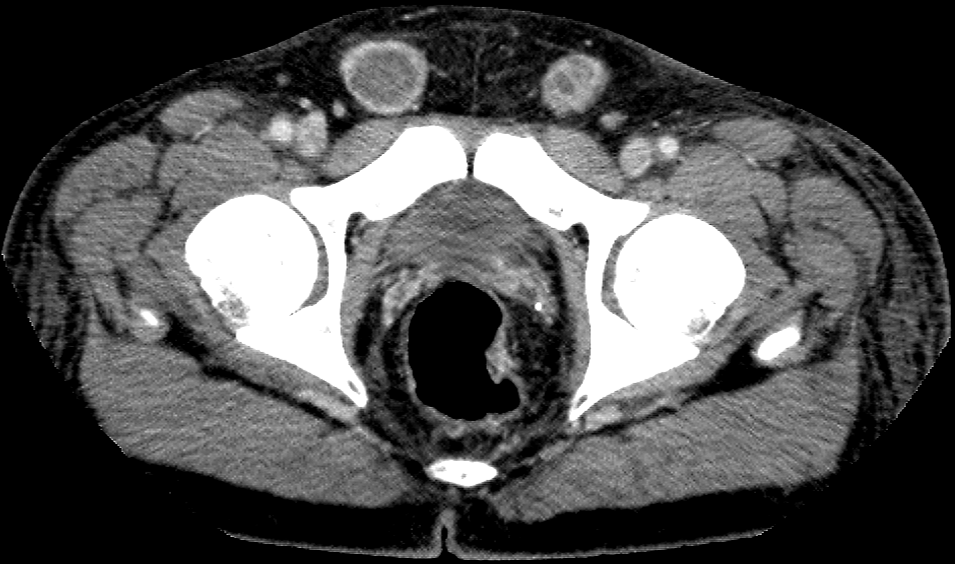
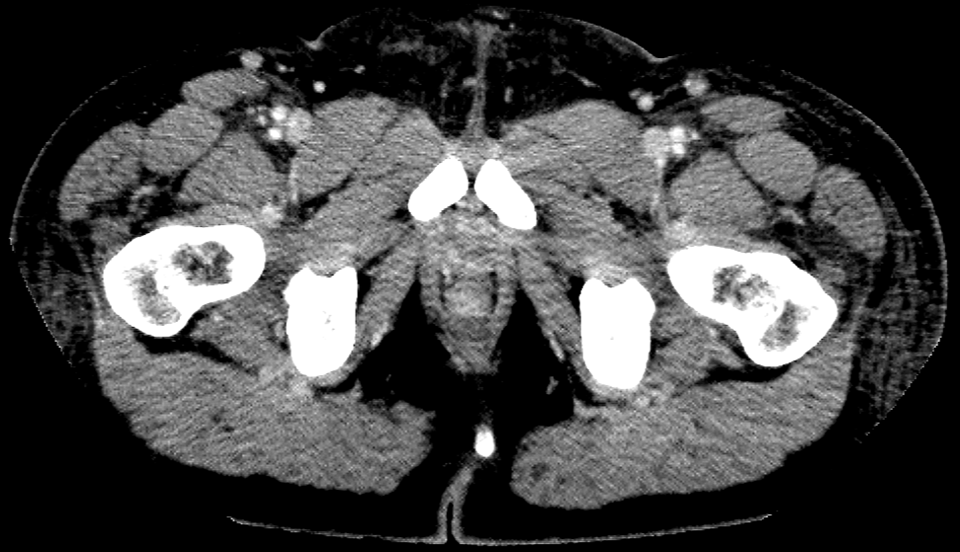
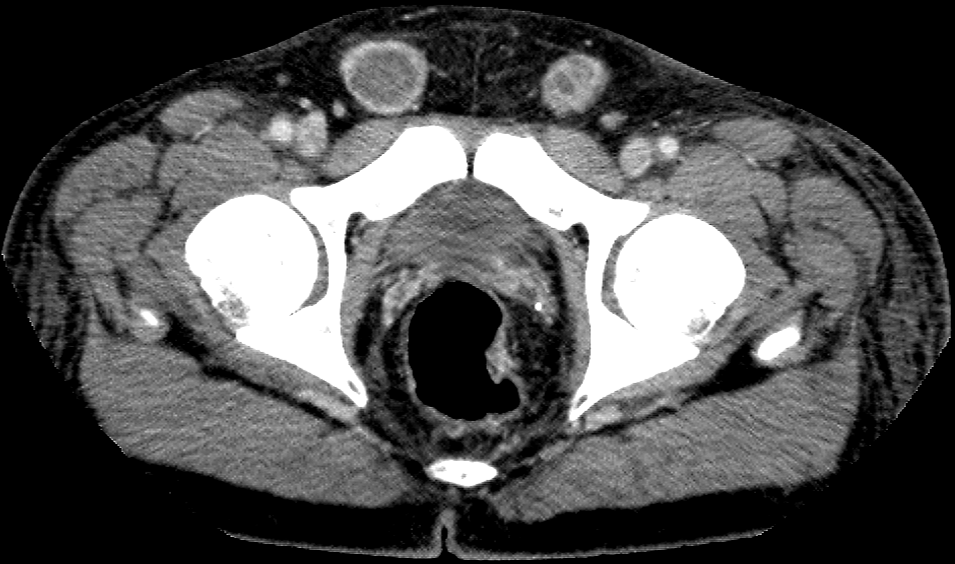
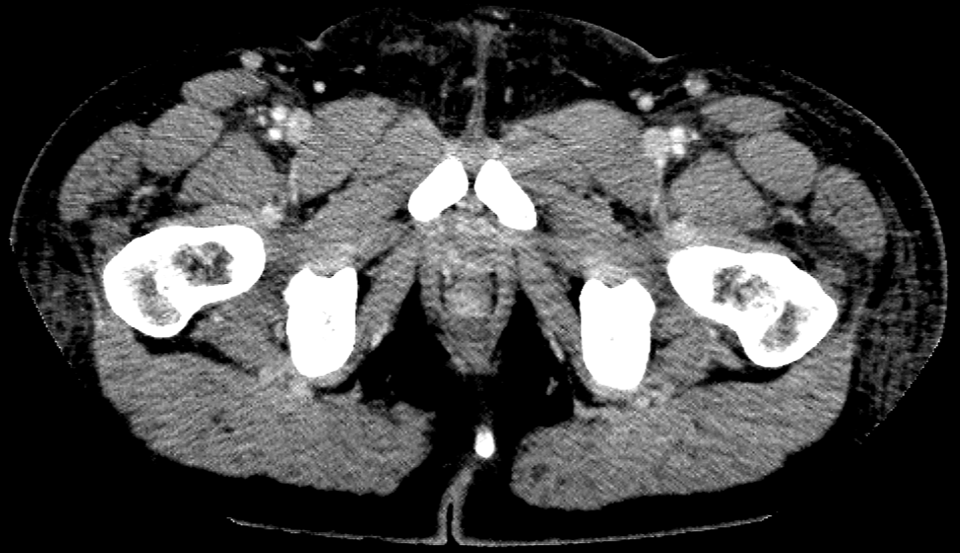
- Bilateral inguinal hernias containing ascites and abnormal peritoneal enhancement. The spermatic cords are not visualized in the groin region on either side.
Diagnosis:
Non-seminomatous germ cell tumors arising from undescended testes with disseminated metastases.
Discussion:
- The absence of spermatic cords in both inguinal regions clinches the diagnosis of bilateral cryptorchidism.
- With cryptorchidism, there is an increased risk of developing testicular germ cell tumors (incidence 1 in 2000). This risk is higher in bilateral cases and in abdominal cryptorchidism.
- In men with untreated cryptorchidism, a secondary malignancy in an undescended testes manifests as an intra-abdominal mass. The imaging clues include:
- An ipsilateral draining vein that empties into the inferior vena cava (if right sided) or the left renal vein (if left sided).
- An empty ipsilateral scrotal sac or absence of spermatic cord structures in the groin region are further pointers.
Testicular tumours
- 95 % of testicular tumours are germ cell tumours (GCT) and 5 % are sex cord stromal tumours.
- Approximately 50 % of GCTs are seminomas and 50 % are nonseminomatous germ cell tumors.
- Radiologically:
- Seminomas are homogenous, solid lobulated masses with intervening fibrovascular septae.
- Nonseminomatous GCTs are heterogenous with areas of necrosis and hemorrhage.
- Nonseminomatous GCTs grow more rapidly and are more likely to be metastatic at presentation when compared to seminomas.
- Sites of metastases from GCTs:
Retroperitoneal and mediastinal lymph nodes, lung, liver, brain, and bone. - Extragonadal sites of GCTs:
Anterior mediastinum, sacrococcygeal region, pineal gland, and neurohypophysis - The radiologist plays a key role in the initial staging of disease, identifying the prognostic factors and also in the assessment of treatment response and treatment related toxicity.
References:
- Coursey Moreno C, Small WC, Camacho JC et al. Testicular tumors: what radiologists need to know—differential diagnosis, staging, and management. RadioGraphics 2015;35(2):400–415.
- Monica J Wood, Richard Thomas, Stephanie A Howard, Marta Braschi-Amirfarzan. Imaging of metastatic germ cell tumors in male patients from initial diagnosis to treatment-related toxicities: A primer for radiologists. AJR 2020;214:24-33
- Para, Sajad & Pal, Dilip. (2016). Spontaneous Massive Hemoperitonium Secondary to Bleeding of a Hepatic from a Testicular Germ Cell Tumour-An Ususual Presentation. Scholars Journal Of Medical Case Reports. 4. 401-403. 10.21276/sjmcr/2016.4.6.12.
- Yu MH, Kim YJ, Park HS, Jung SI, Jeon HJ. Imaging Patterns of Intratumoral Calcification in the Abdominopelvic Cavity. Korean J Radiol. 2017;18(2):323?335. doi:10.3348/kjr.2017.18.2.323
- Dolapsakis C, Pavli P, Panagopoulos A, et al. Haemoperitoneum Due to Spontaneous Rupture of a Liver Metastasis. Eur J Case Rep Intern Med. 2019;6(7):001142. 2019 Jun 26. doi:10.12890/2019_001142
Dr. Anoop Mangalappilly
DNB Resident
Manipal Hospitals Radiology Group
Dr. Anita Nagadi
MD, MRCPCH, FRCR, CCT
Senior Consultant Radiology
Manipal Hospitals Radiology Group