A 39-year-old female with a history of chest discomfort and persisting breathlessness
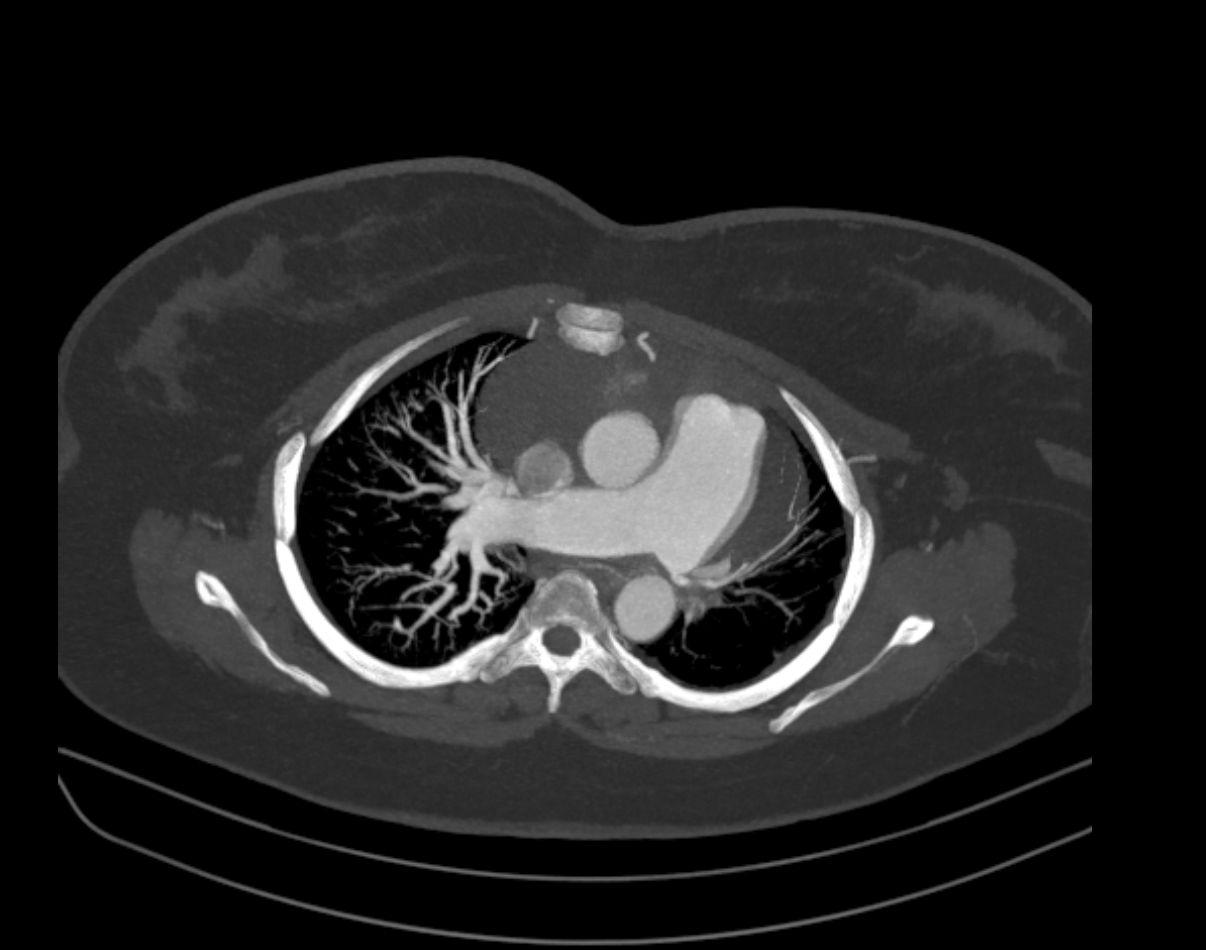
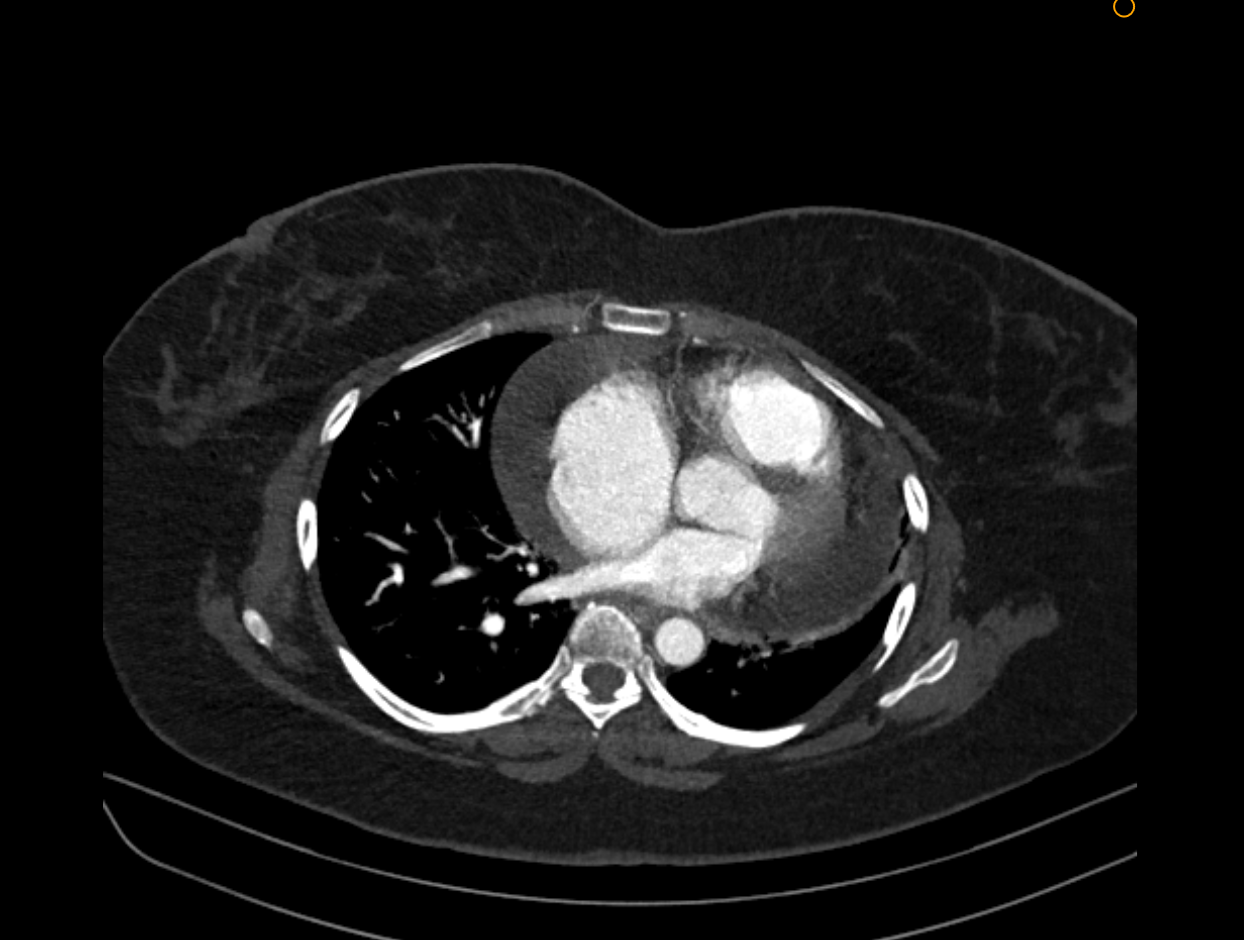
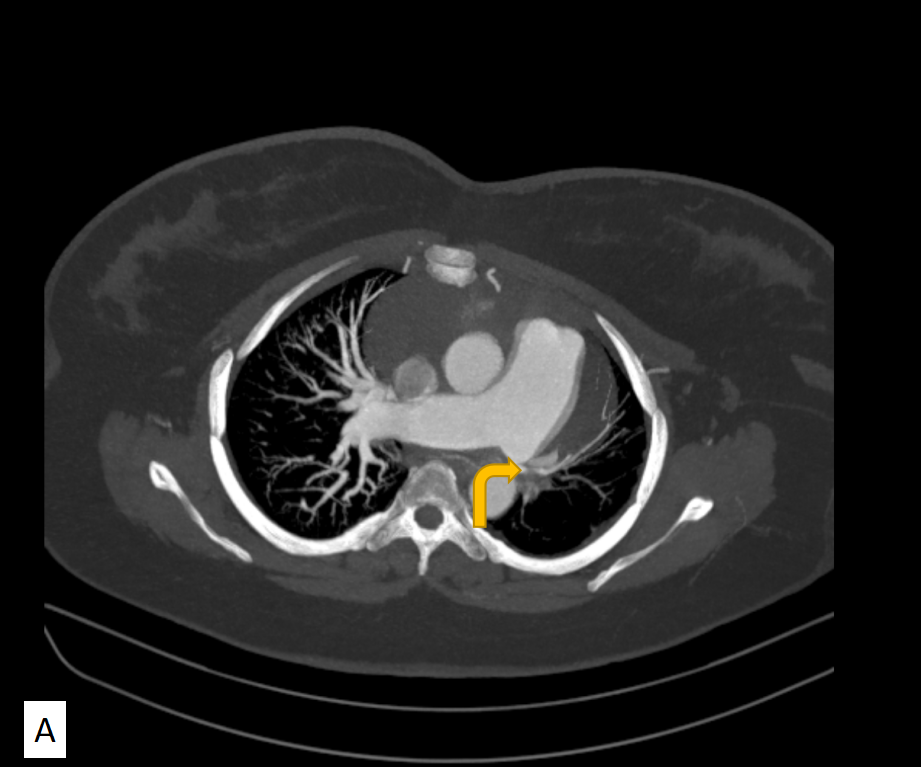
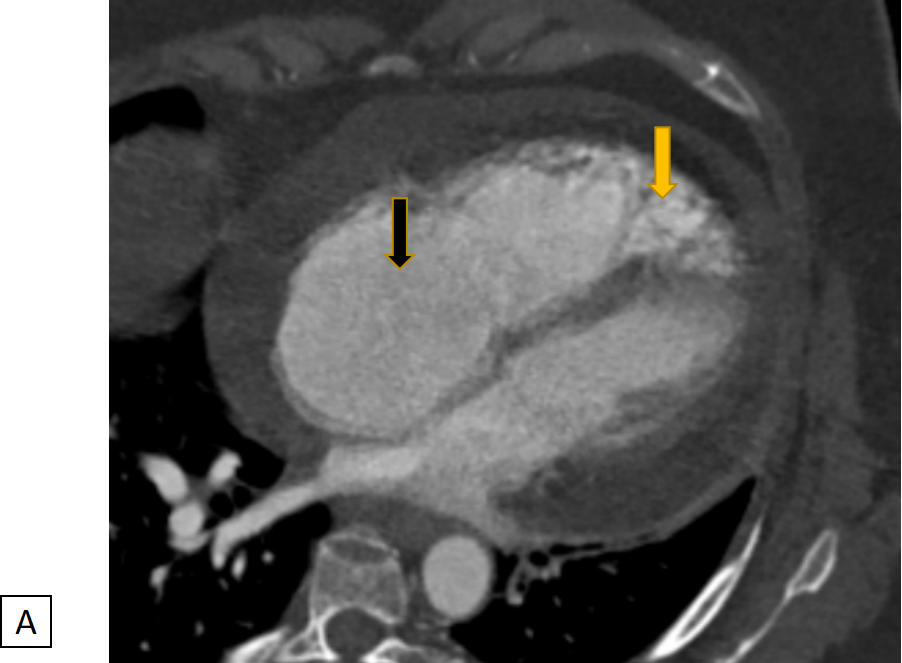
- A) MIP image displaying an abrupt cut-off of the left pulmonary artery with mild soft tissue thickening (yellow bent arrow).
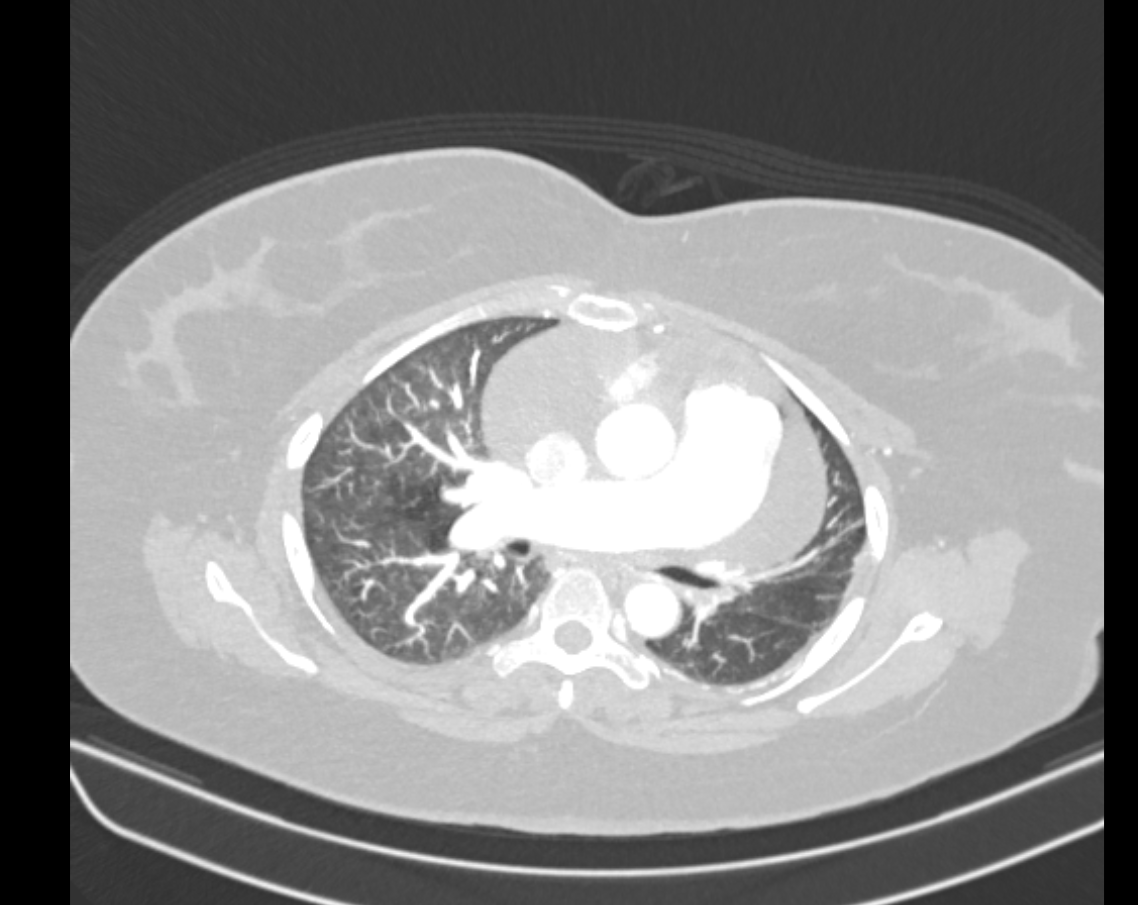
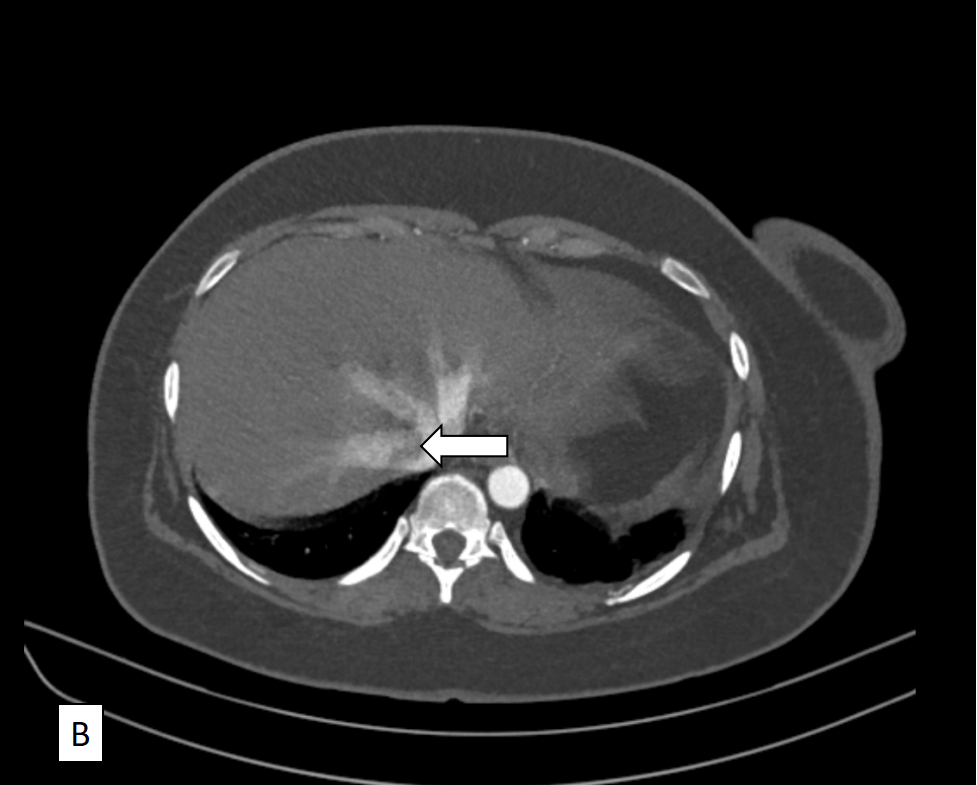
- B) Plain CT image revealing calcification (white bent arrow) corresponding to the noted soft tissue thickening.
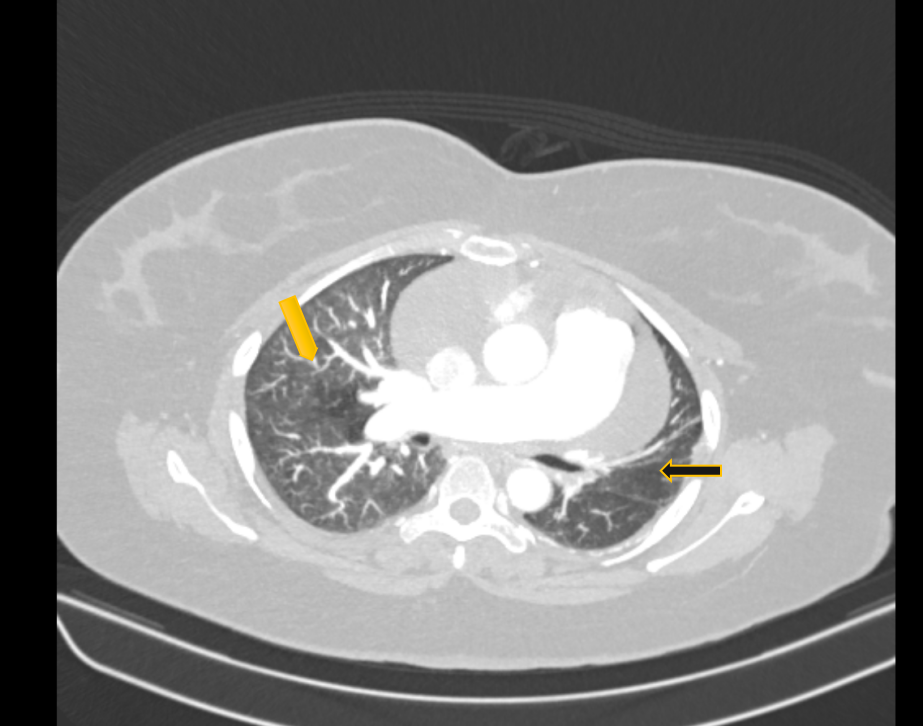
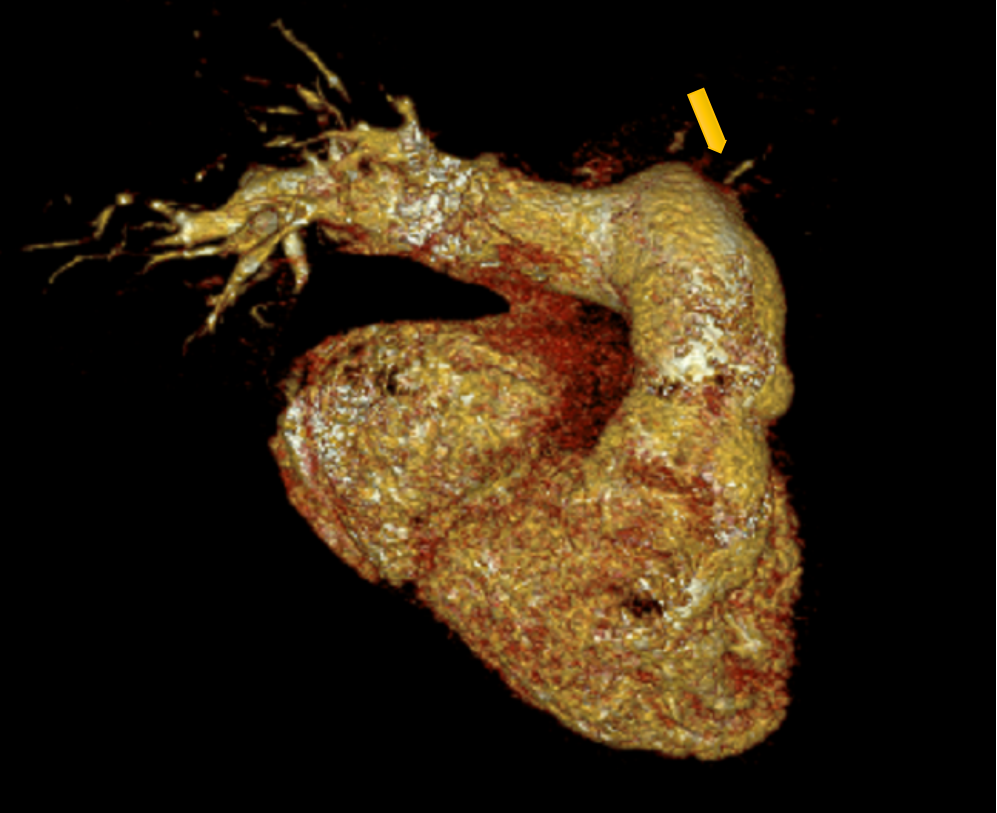
- Non-visualization of segmental and sub-segmental branches of the descending interlobar artery (yellow arrow).
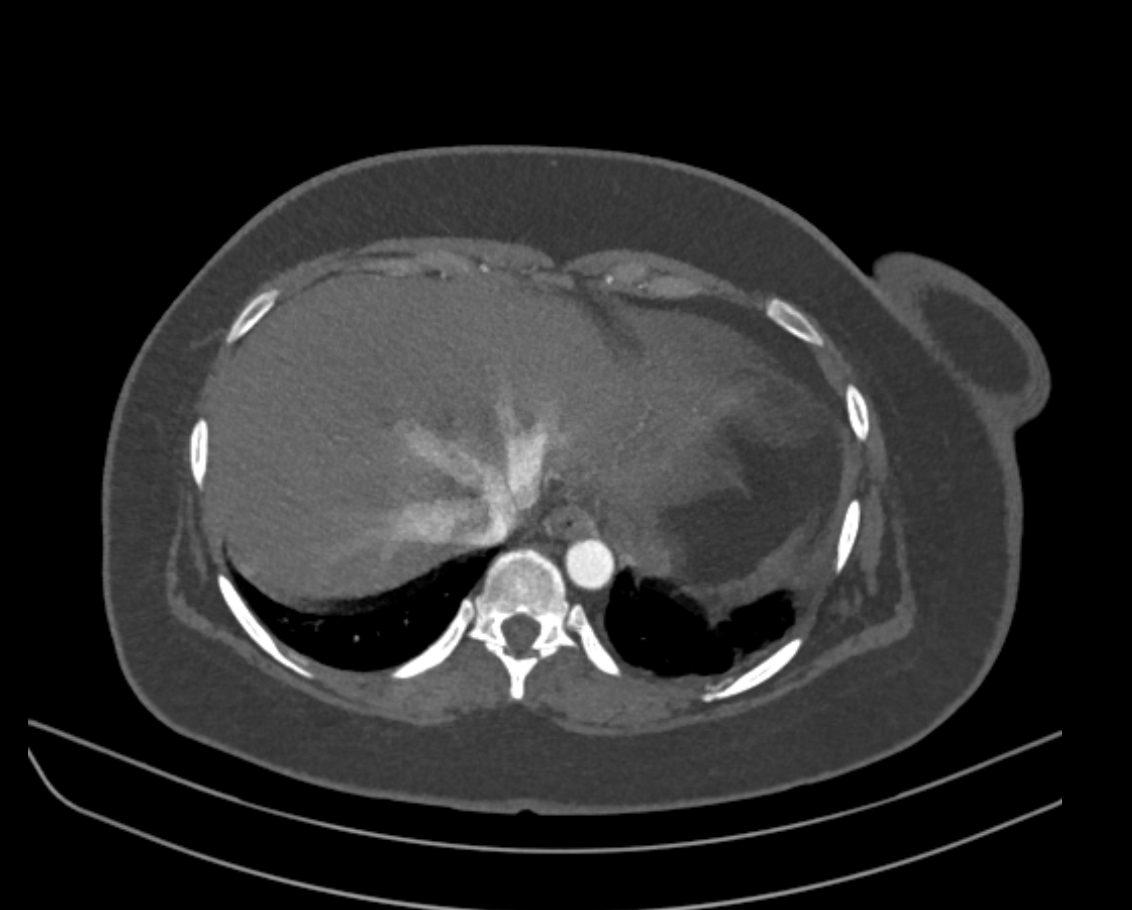
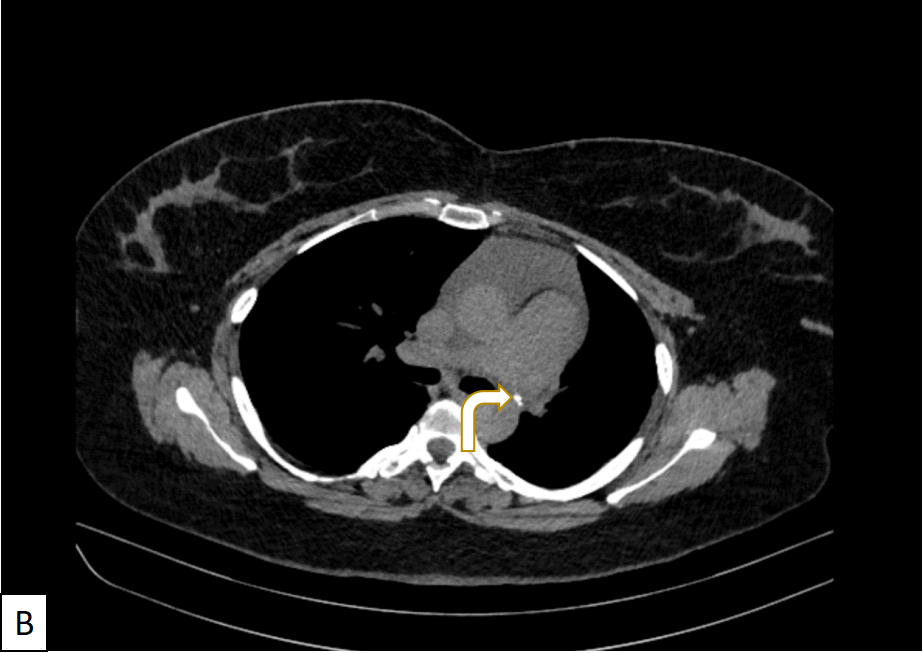
- Diffuse mosaic attenuation (yellow arrow) observed in both lungs. Additionally, there is volume loss of the left lung (black arrow) with associated crowding of ribs.
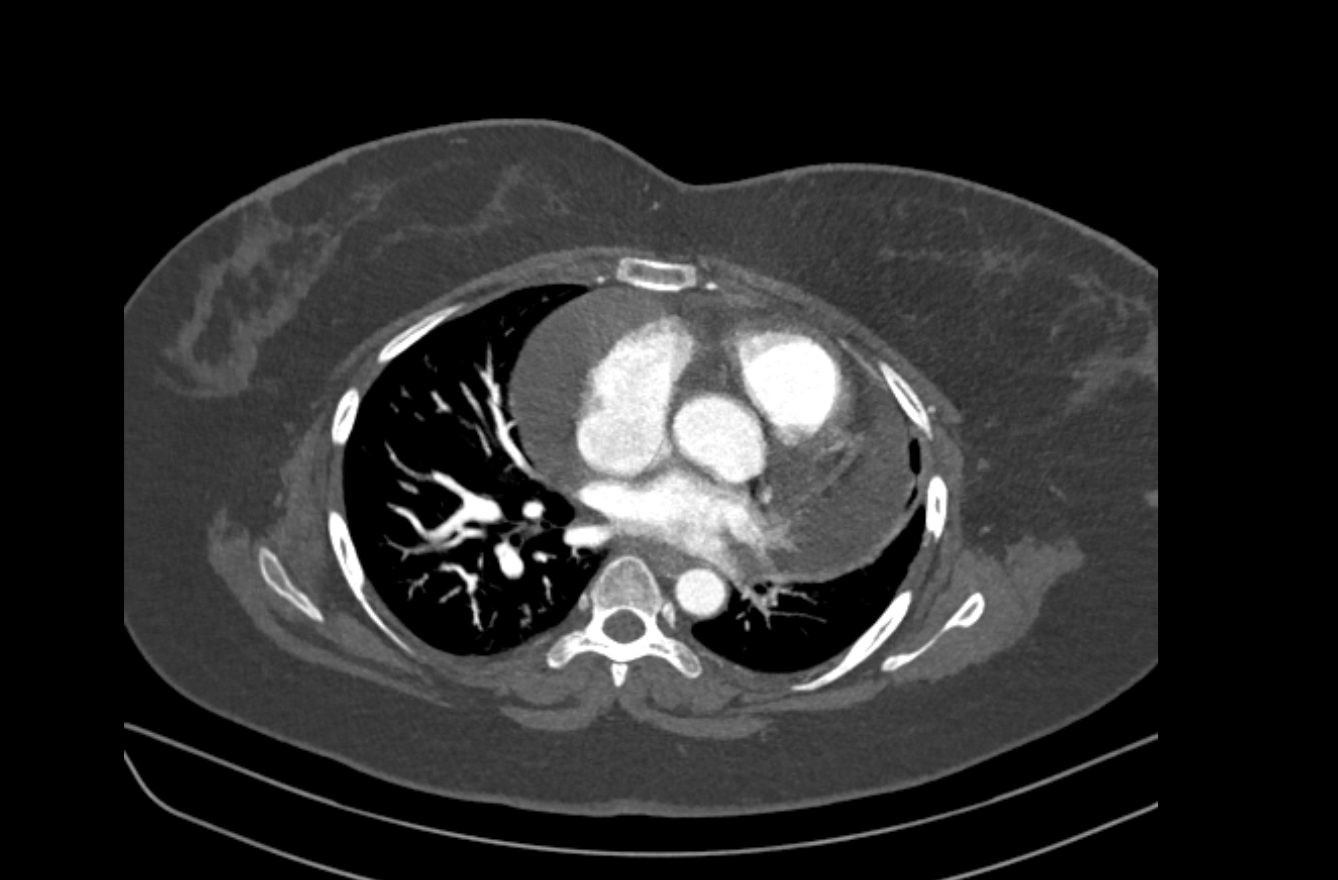
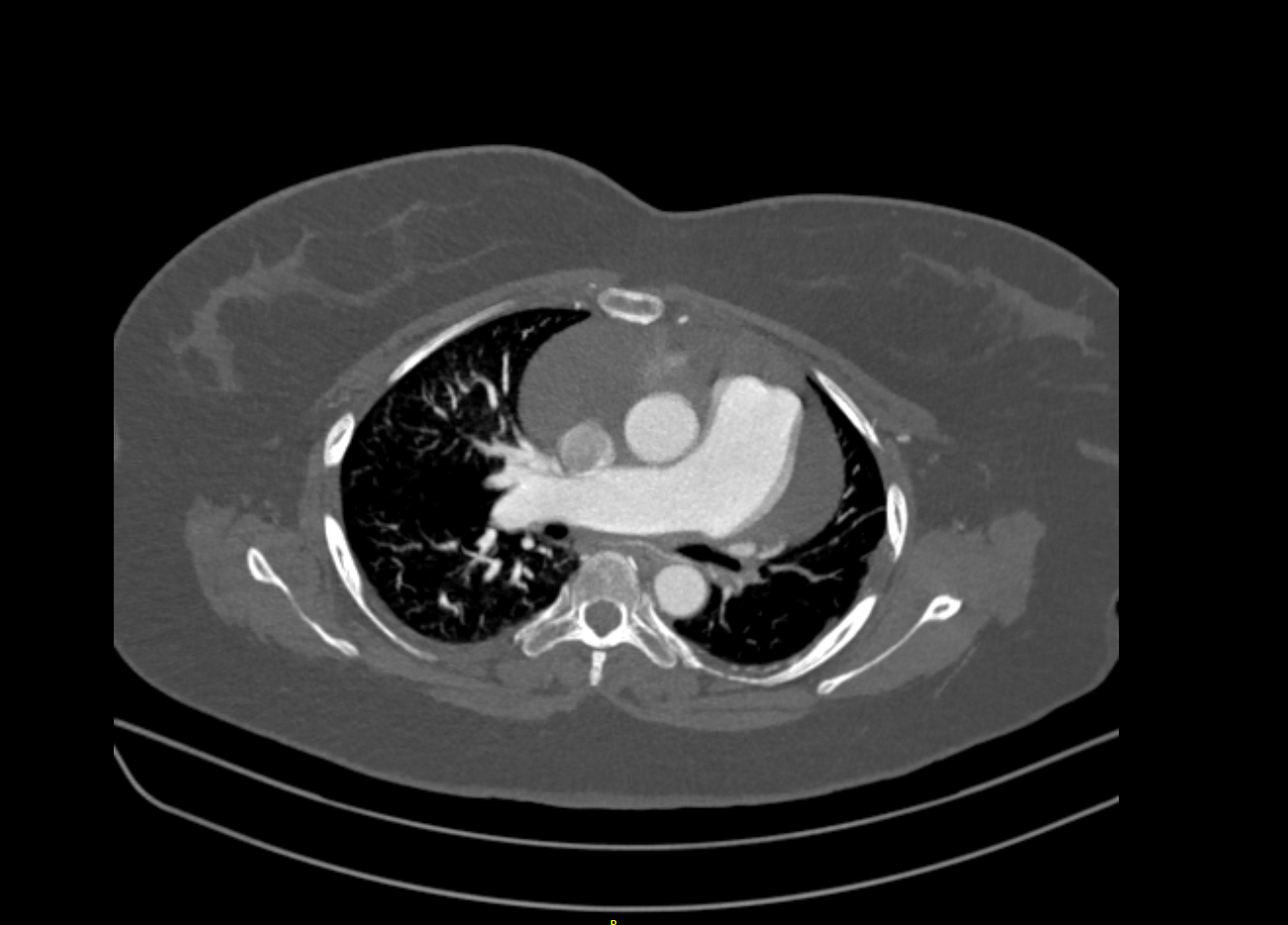
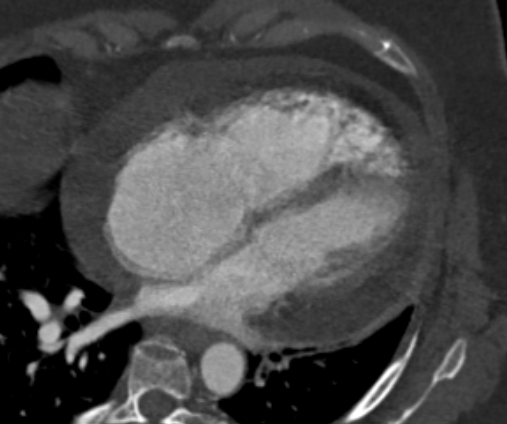
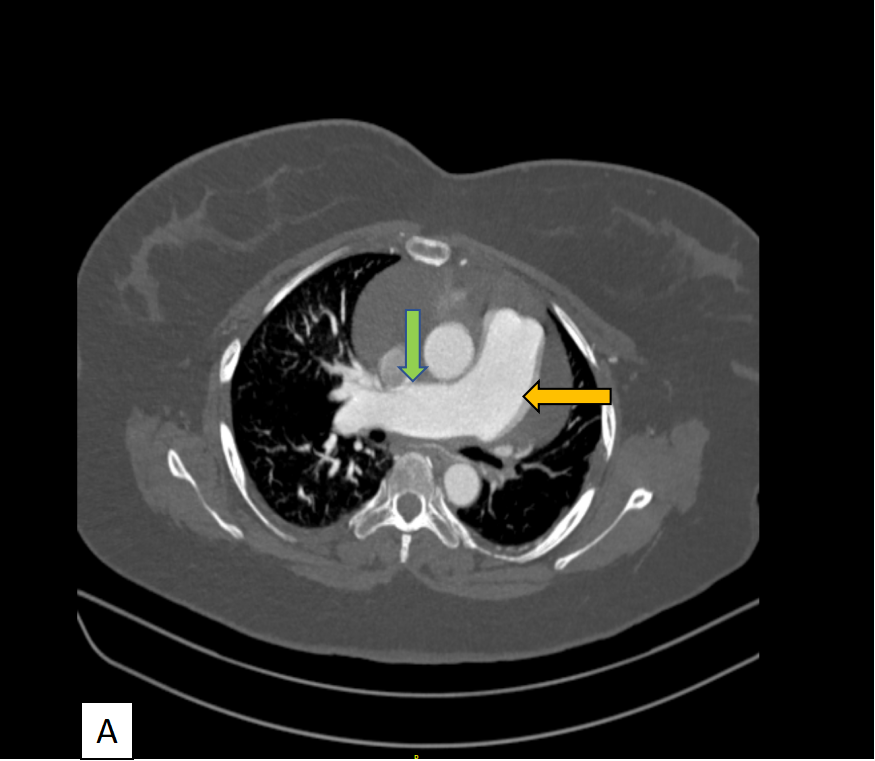
- A) Dilated main pulmonary artery (yellow arrow) and right pulmonary artery (green arrow) are observed.
- B) Moderate pericardial effusion is visible (black arrow).
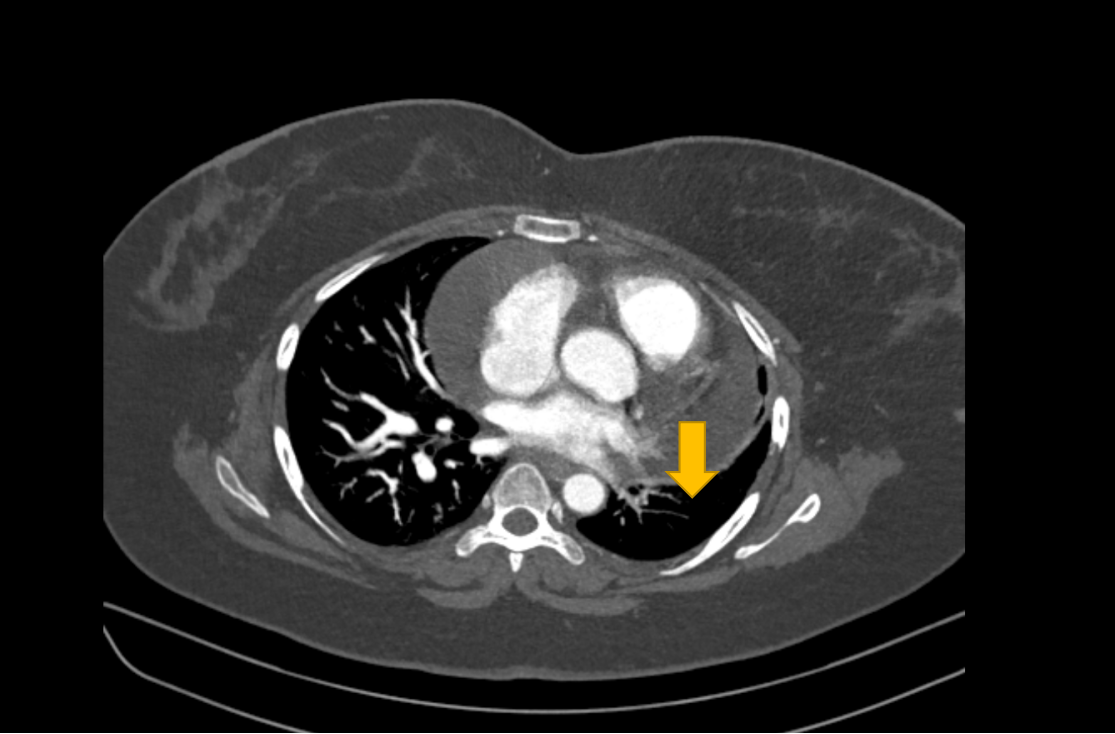
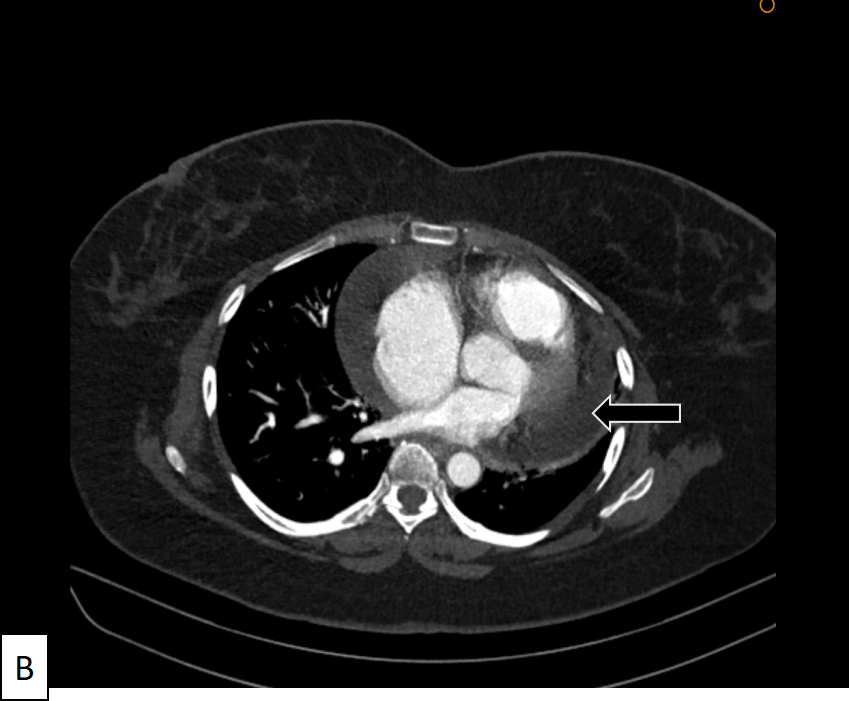
- A) Dilated right ventricle (yellow arrow) with prominent trabeculation, straightening of the interventricular septum, and a moderately dilated right atrium (black arrow) are evident.
- B) Early reflux of contrast in the hepatic veins is observed, indicative of right heart strain.
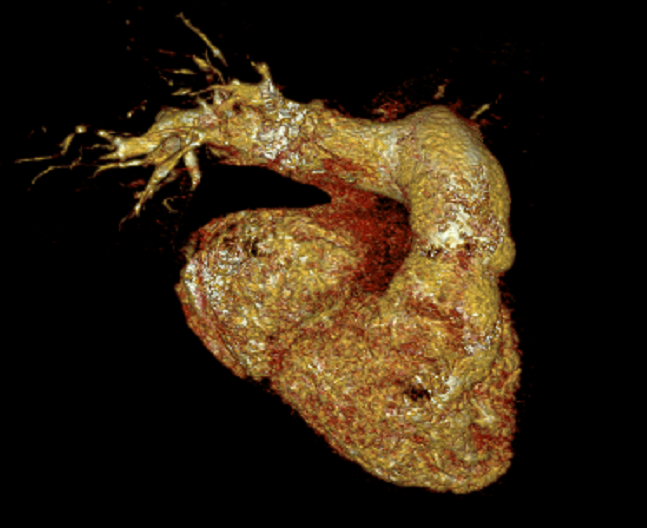
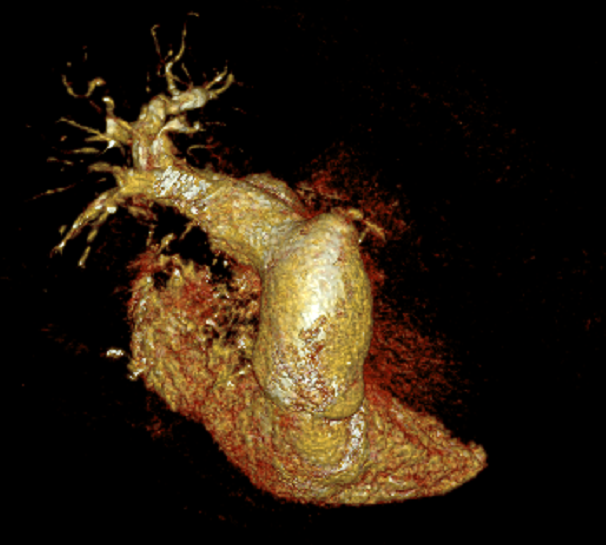
- Oblique Volume Rendering Technique (VRT) images confirming the abrupt cut-off of the left pulmonary and segmental arteries (yellow arrow) due to focal narrowing.
DIAGNOSIS:
- Chronic Pulmonary Thromboembolic Pulmonary Hypertension (CTEPH) with resultant right heart failure.
DISCUSSION:
- Chronic pulmonary thromboembolism (CPTE) represents the long-term consequences of pulmonary emboli, often manifesting as a complex interplay of vascular and parenchymal changes.
- A radiologist's comprehensive evaluation is crucial for recognizing both vascular and parenchymal signs.
Radiological Evaluation
1) Vascular signs:
a) Complete occlusion: vessel cut off.
b) Partial occlusion: look for
- Webs, bands, or focal stenosis
- Areas of irregular thickening of the vessel wall
- Calcified thrombus or crescent-shaped defect
c) Collateral vessels
- Bronchial artery dilation (> 2 mm) and tortuosity
- Non-bronchial arteries: In pleural, intercostal, phrenic, internal mammary areas
2) Signs of Pulmonary Hypertension (PH)
- Main pulmonary artery dilation (> 33 mm)
- Ratio of main pulmonary artery diameter to ascending aorta diameter >1.1:1
3)Right ventricular signs:
- Enlargement and hypertrophy
- Ratio of right ventricle diameter to left ventricle diameter >1:1
- Bowing of the interventricular septum toward the left ventricle
4) Lung parenchymal signs:
a. Scars from prior pulmonary infarctions
- Bands, irregular peripheral linear opacities
- Wedge-shaped opacities with pleural thickening
b. Mosaic lung attenuation
Treatment and Management:
- Pulmonary endarterectomy (PEA) is the treatment of choice in CTEPH patients.
- Understanding radiological features is crucial for diagnosis, severity assessment, and treatment planning.
- Clinic radiological correlation ensures accurate diagnosis, helps determine disease severity, and guides the selection of suitable treatments, be it surgical (PEA), medical, or interventional (Balloon Pulmonary Angioplasty).
- Regular follow-up imaging is essential for monitoring disease progression and treatment effectiveness.
DIFFERENTIAL DIAGNOSIS:
Chronic Pulmonary Thromboembolism (Without Pulmonary Hypertension):
- Marked by vascular changes like irregular vessel walls and webs.
- Distinguishing it from cases with associated pulmonary hypertension is crucial.
- Pulmonary endarterectomy, a potentially curative surgery, is reserved for CTPEH patients.
Pulmonary Vasculitis:
- Wegener's: Localized inflammation in a specific pulmonary artery or branches.
- Indicators: Inflammatory changes in the vessel wall, leading to irregularities and stenosis.
Congenital Anomalies in Pulmonary Arteries:
- Hypoplasia or agenesis, often coexisting with congenital cardiovascular disorders.
- Examples: Tetralogy of Fallot, septal defects.
REFRENCES:
- Nishiyama, K. H., Saboo, S. S., Tanabe, Y., Jasinowodolinski, D., Landay, M. J., & Kay, F. U. (2018). Chronic pulmonary embolism: diagnosis. Cardiovascular Diagnosis and Therapy, 8(3), 253–271. doi:10.21037/cdt.2018.01.09
- Castañer, E., Gallardo, X., Ballesteros, E., Andreu, M., Pallardó, Y., Mata, J. M., & Riera, L. (2009). CT Diagnosis of Chronic Pulmonary Thromboembolism. RadioGraphics, 29(1), 31–50. doi:10.1148/rg.291085061
Dr. Faizel Abdul Khader
Consultant Radiologist.
Manipal Hospital, Varthur road, Bengaluru.
Dr. Nanda Gopal
Cross sectional fellow.
Manipal Hospital, Varthur road, Bengaluru.