A 38-year-old with the history of fever, cough, right sided weakness, slurring of speech, left sided reduced vision and left facial swelling. Steroid intake history for 20 days.
A 38-year-old with the history of fever, cough, right sided weakness, slurring of speech, left sided reduced vision and left facial swelling. Steroid intake history for 20 days.
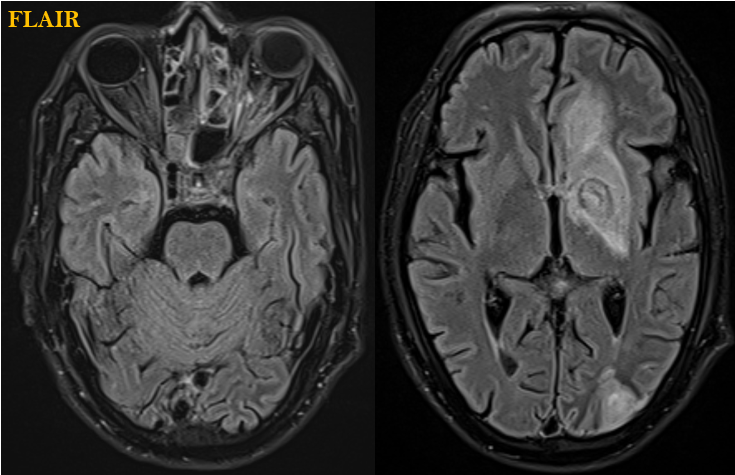
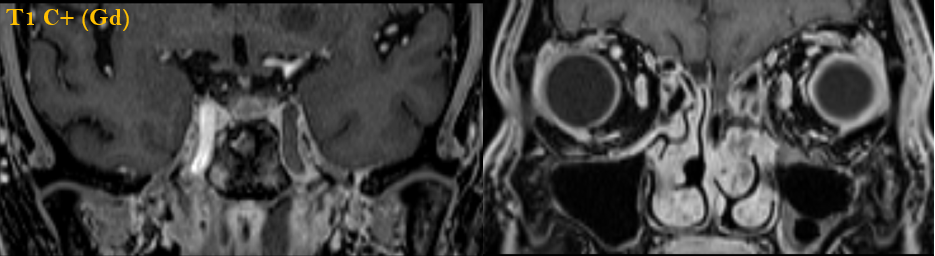
- Mild mucosal thickening of left maxillary sinus with no mucosal enhancement on post contrast images.
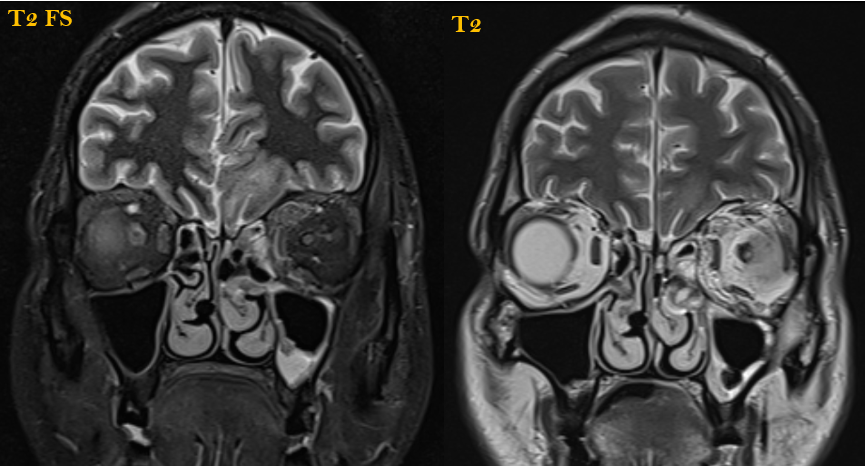
- Left orbital cellulitis, optic nerve ischemia and mild proptosis. Left side cavernous sinus involvement.
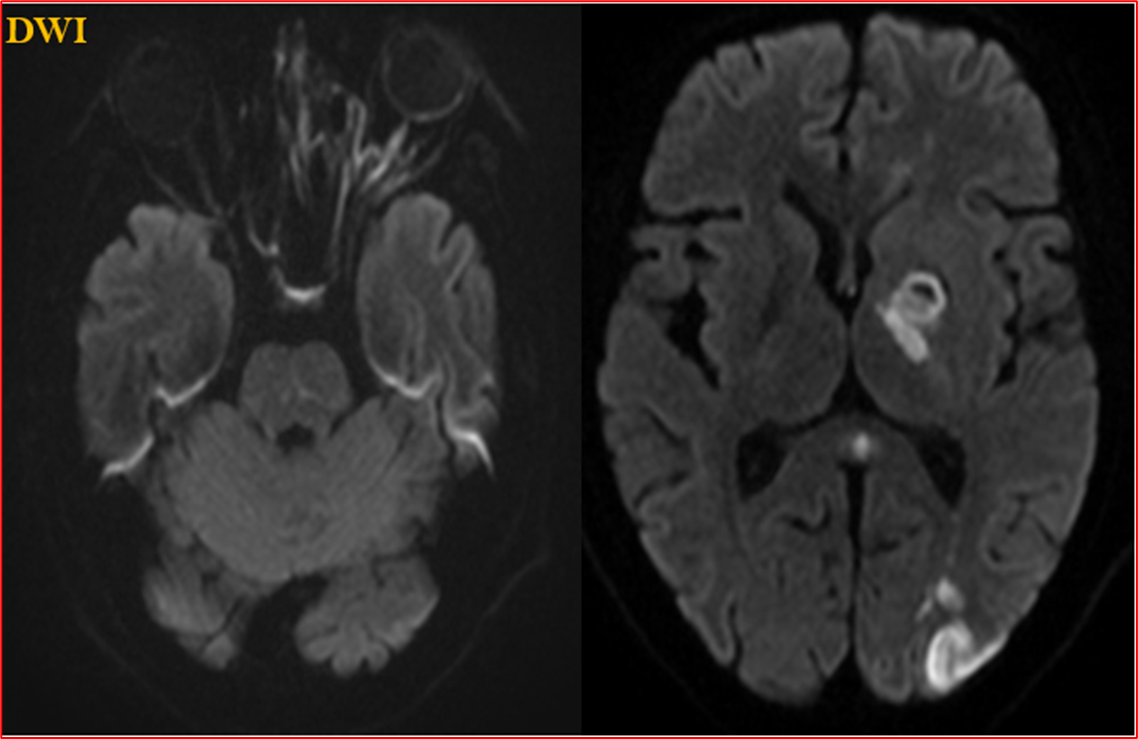
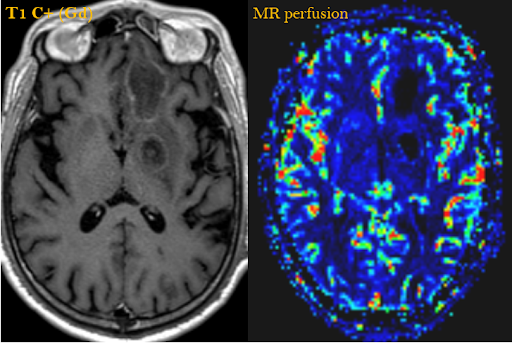
- Left internal carotid artery thrombosis with multiple left side external and deep watershed zone infarcts. Fungal abscesses in left basal ganglia and basifrontal lobe.
DIAGNOSIS:
Rhino-orbital cerebral mucormycosis (ROCM).
DISCUSSION:
- Rhino-orbito-cerebral mucormycosis (ROCM) is considered as a rare invasive infection caused by class phycomycetes fungi involving immunocompromised patients, arising from nasal and sinus mucosa, spreads rapidly to orbit and brain.
- Extensive angioinvasion is considered as the main cause leading to vascular thrombosis and tissue necrosis. Vascular involvement is more common cause of high morbidity and mortality, infiltrating cavernous sinus and orbital apex leading to cellulitis of face, loss of vision.
- Intracranial involvement can cause narrowing of internal carotid artery leading to ischemic infarcts. Meningeal involvement can be seen.
- Imaging helps in diagnosis of ROCM to evaluate the extent of disease plays a crucial role in early diagnosis and timely intervention.
- CT scan demonstrates nodular mucosal thickening with absence of fluid levels and hyperdense content leading to erosions of bony sinus walls.
- MRI provides better evaluation of intracranial and soft tissue involvement, skull base invasion, perineural spread and vascular obstruction.
- MRI demonstrates variable signal intensity depending on the sinus contents, due to iron and manganese in the fungal elements.
- MRI contrast study shows invasion of orbital soft tissues, skull base infiltration, perineural spread, intracranial complications and vascular obstruction involving internal carotid artery. T2 slow flow or loss of flow voids can suggest internal carotid artery invasion by the fungus.
- Perineural spread is most commonly seen in head and neck malignancies more often seen in adenoid cystic carcinoma. Fungal hyphae tend to involve nerves and vessel wall leading to perineural spread and cavernous sinus invasion.
- ROCM is considered as an emerging rapidly disseminating fungal infection when associated with immunocompromised conditions and carry fatal prognosis with cavernous sinus and cerebral involvement.
- Radiologists should evaluate the extension and involvement of invasive fungal sinusitis which can lead to early diagnosis and timely management with antifungal agents and surgical debridement further helping to reduce morbidity and mortality.
REFERENCES:
- Safder S, Carpenter JS, Roberts TD, Bailey N. The “black turbinate” sign: an early MR imaging finding of nasal mucormycosis. American journal of neuroradiology. 2010 Apr 1;31(4):771-4 (PMID: 19942703).
- Parsi K, Itgampalli RK, Vittal R, Kumar A. Perineural spread of rhino-orbit cerebral mucormycosis caused by Apophysomyceselegans. Annals of Indian Academy of Neurology. 2013 Jul;16(3):414 (PMID: 24101833).
- Lone PA, Wani NA, Jehangir M. Rhino-orbit-cerebral mucormycosis: Magnetic resonance imaging. Indian Journal of Otology. 2015 Jul 1;21(3):215, (DOI: 10.4103/0971-7749.159700).
- Mehta S, Pandey A. Rhino-Orbital Mucormycosis Associated With COVID-19. Cureus. 2020 Sep;12(9).
Dr. Bhupendar Singh
Radiology Resident,
Manipal Hospitals Radiology Group
Dr. Ashwini C
MD, FRCR
Consultant Radiologist,
Manipal Hospitals Radiology Group.