A 27-year-old female presented with complaints of headache
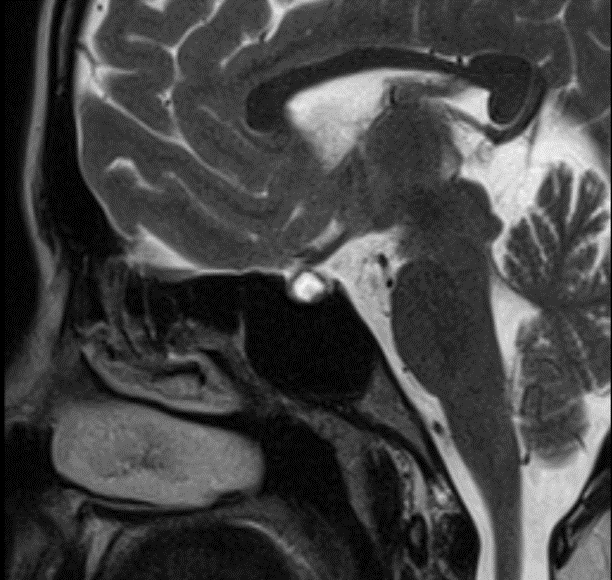
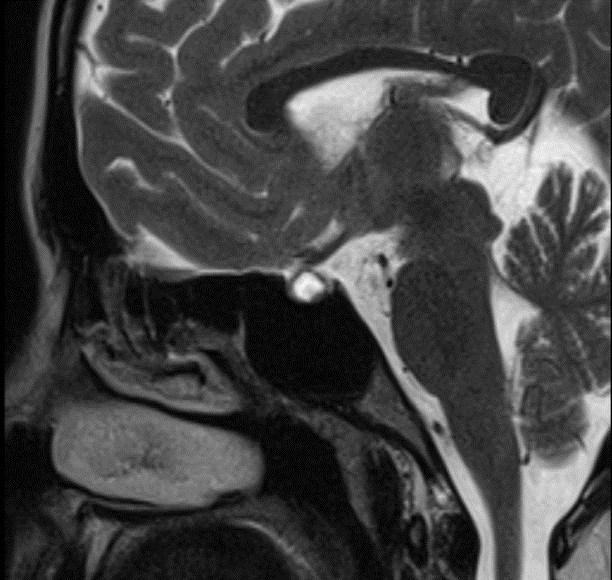
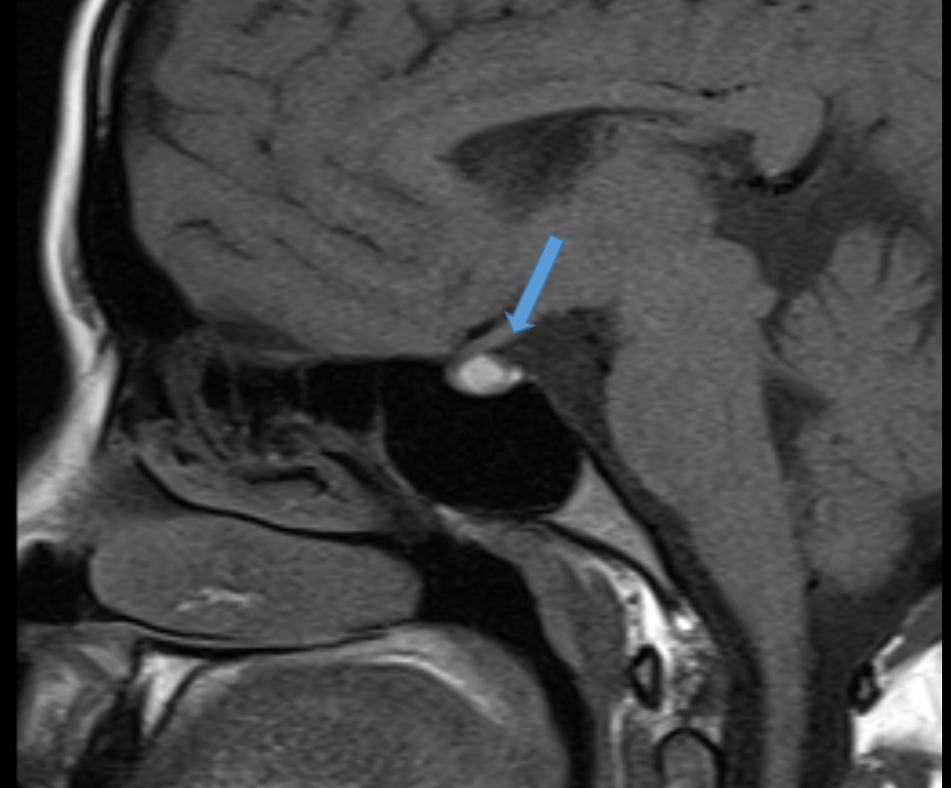
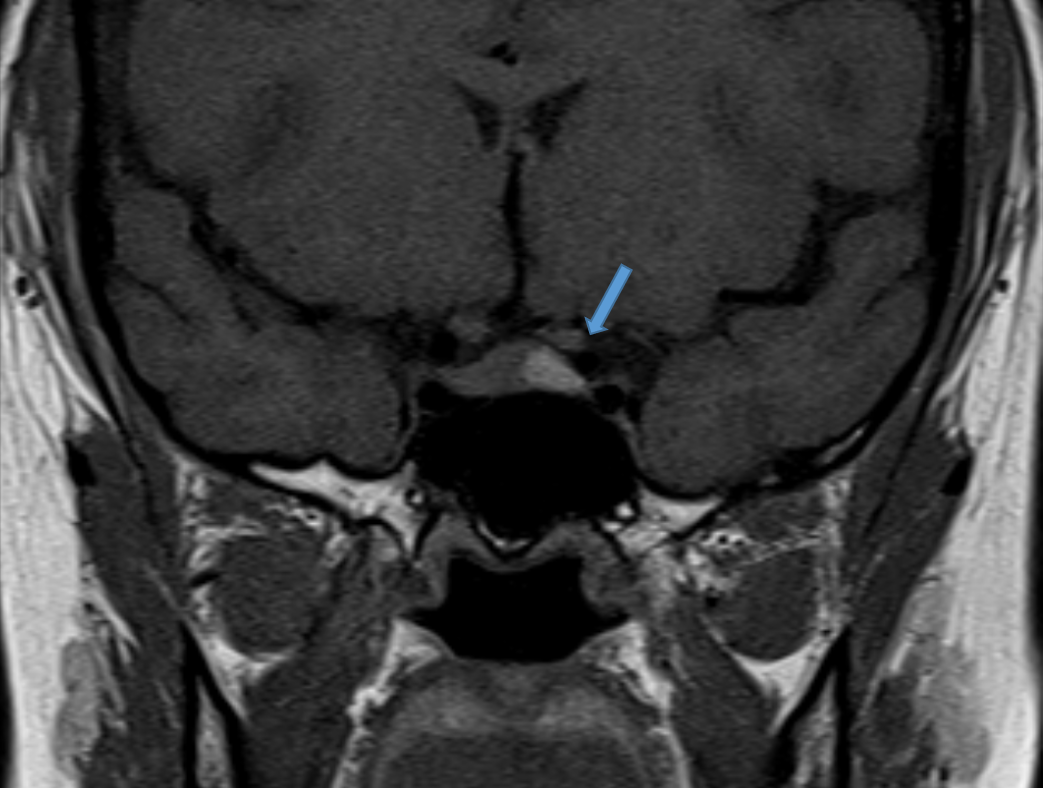
1. Sagittal and Coronal T1 weighted images of sella
Shows a well-defined intrasellar T1 hyperintense lesion
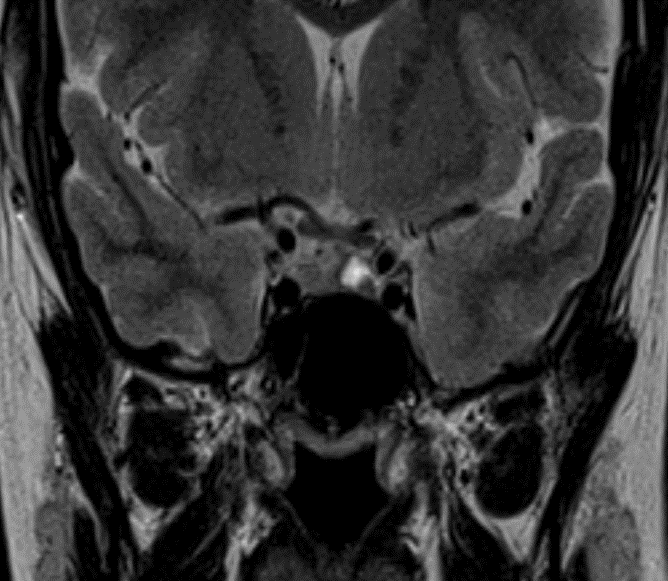
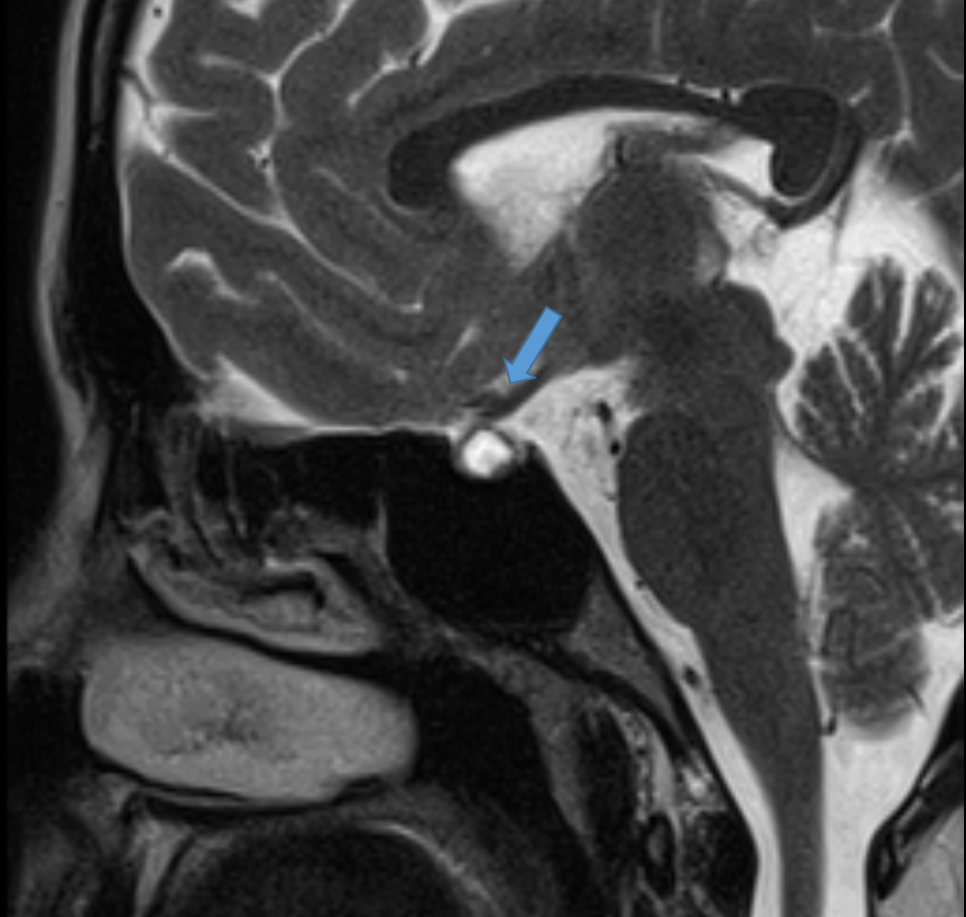
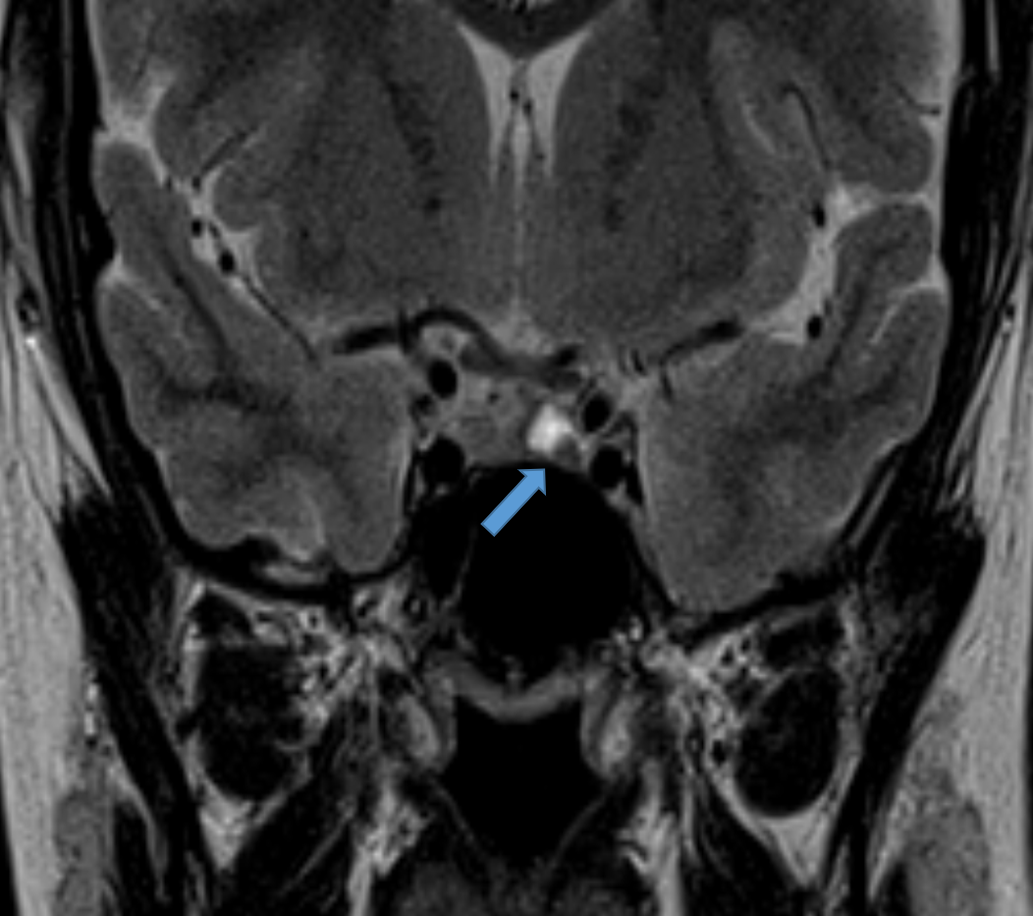
2. Sagittal and coronal T2 weighted images of sella
Shows a T2 hyperintense intrasellar cystic lesion with a peripheral T2 hypointense intra-cystic nodule within
DIAGNOSIS:
Rathke’s cleft cyst
DISCUSSION:
Rathke pouch forms during the 4th week of embryologic development as a rostral outpouching from the roof of the primitive oral cavity. The anterior wall of the pouch gives rise to the anterior lobe of the pituitary (pars distalis). The posterior wall of the pouch does not proliferate and remains as the intermediate lobe of the pituitary (pars intermedia). The lumen of the pouch narrows to form a cleft (Rathke cleft) that normally regresses. Persistence of this cleft with the expansion is believed to be the origin of a Rathke cleft cyst.
CLINICAL PRESENTATION:
The vast majority of Rathke cleft cysts are asymptomatic and incidentally found.
- If large, they may cause:
- visual disturbances: due to compression of the optic chaisma
- pituitary dysfunction
- due to compression of adjacent pituitary tissue and distortion of the pituitary stalk
- present in up to 69% of symptomatic cases
- headaches
RADIOGRAPHIC FEATURES
On lateral skull x-ray, it can rarely cause sellar enlargement if reaches large size
CT
- non-contrast
- typically non-calcified and of homogeneous low attenuation
- uncommonly it may be of mixed iso- and low-attenuation, or contain small curvilinear calcifications in the wall (seen in 10-15% of cases)
- postcontrast
- typically non-enhancing
MRI
- Rathke cleft cysts are usually in the midline, unicameral (without septations) and homogeneous in signal intensity . Fluid fluid levels are uncommon and are more suggestive of a pituitary adenoma .
- The signal characteristics vary according to the cyst composition, which may be mucoid or serous.
T1
- 50% are hyperintense (high protein content)
- 50% are hypointense
T2
- 70% are hyperintense
- 30% are iso or hypointense
- 20 % have a hypointense rim (this is more common in adenomas)
T1 C+ (Gd)
- no contrast enhancement of the cyst is seen; however, a thin enhancing rim of surrounding compressed pituitary tissue may be apparent
- An intracystic nodule (sometimes referred to as intracystic dot) is present in 65-75% of cases . When present it is usually hyperintense on T1 and hypointense on T2 compared to surrounding fluid, although, depending on the signal of the surrounding fluid, it may be inapparent on one sequence or the other
DIFFERENTIALS
- Shows peripheral enhancement
- fluid-fluid level or hemorrhagic debris
- off midline location
- septations
- no gender difference
- similar age group
- usually suprasellar or have a suprasellar component
- tend to calcify
REFERENCES
- Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239 (3): 650-64. doi:10.1148/radiol.2393050823– Pubmed citation
- Swearingen B, Biller BM. Diagnosis and management of pituitary disorders. Humana Pr Inc. (2008) ISBN:1588299228. Read it at Google Books– Find it at Amazon
- Byun WM, Kim OL, Kim D. MR imaging findings of Rathke’s cleft cysts: significance of intracystic nodules. AJNR Am J Neuroradiol. 2000;21 (3): 485-8. AJNR Am J Neuroradiol (full text)– Pubmed citation
- Kucharczyk W, Peck WW, Kelly WM et-al. Rathke cleft cysts: CT, MR imaging, and pathologic features. Radiology. 1987;165 (2): 491-5. Radiology (abstract)– Pubmed citation
- Shin JL, Asa SL, Woodhouse LJ et-al. Cystic lesions of the pituitary: clinicopathological features distinguishing craniopharyngioma, Rathke’s cleft cyst, and arachnoid cyst. J. Clin. Endocrinol. Metab. 1999;84 (11): 3972-82. doi:10.1210/jc.84.11.3972– Pubmed citation
Dr. SRIRAM PATWARI
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. SHARNITHA JOHNSON
Fellow in Radiology
Manipal Hospital, Yeshwanthpur, Bengaluru.