75 year, male, Complaints of bleeding per rectum
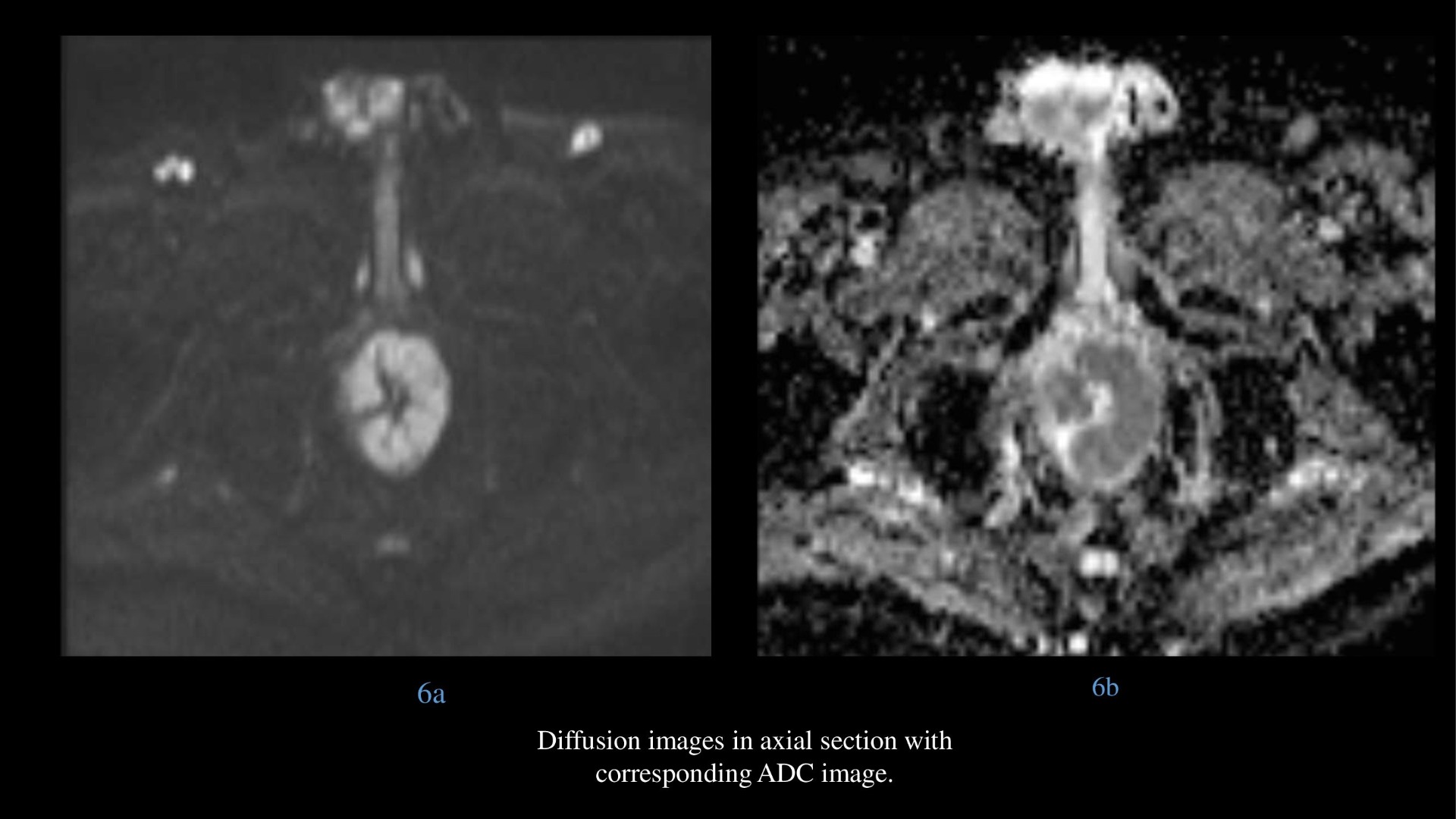
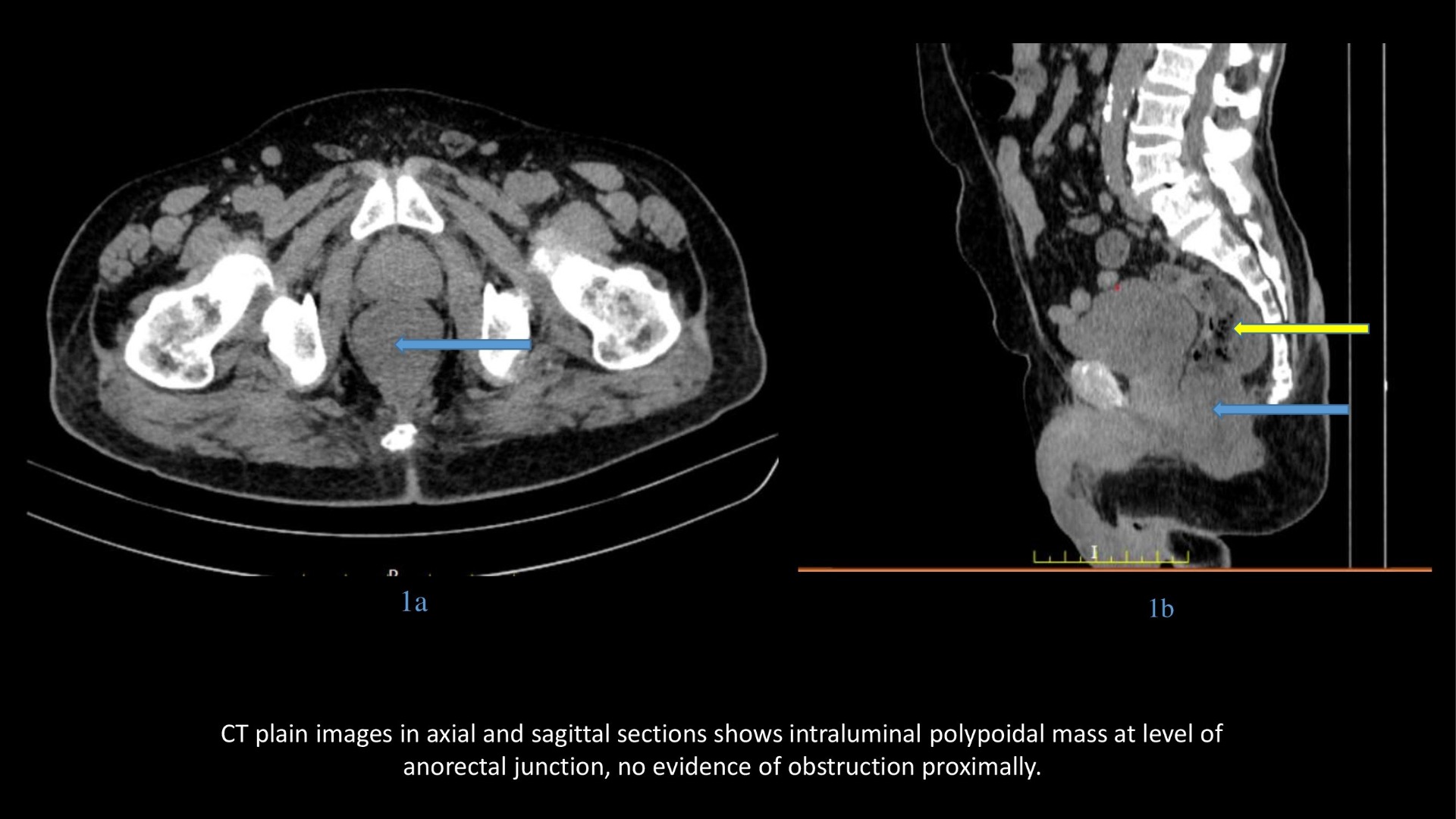
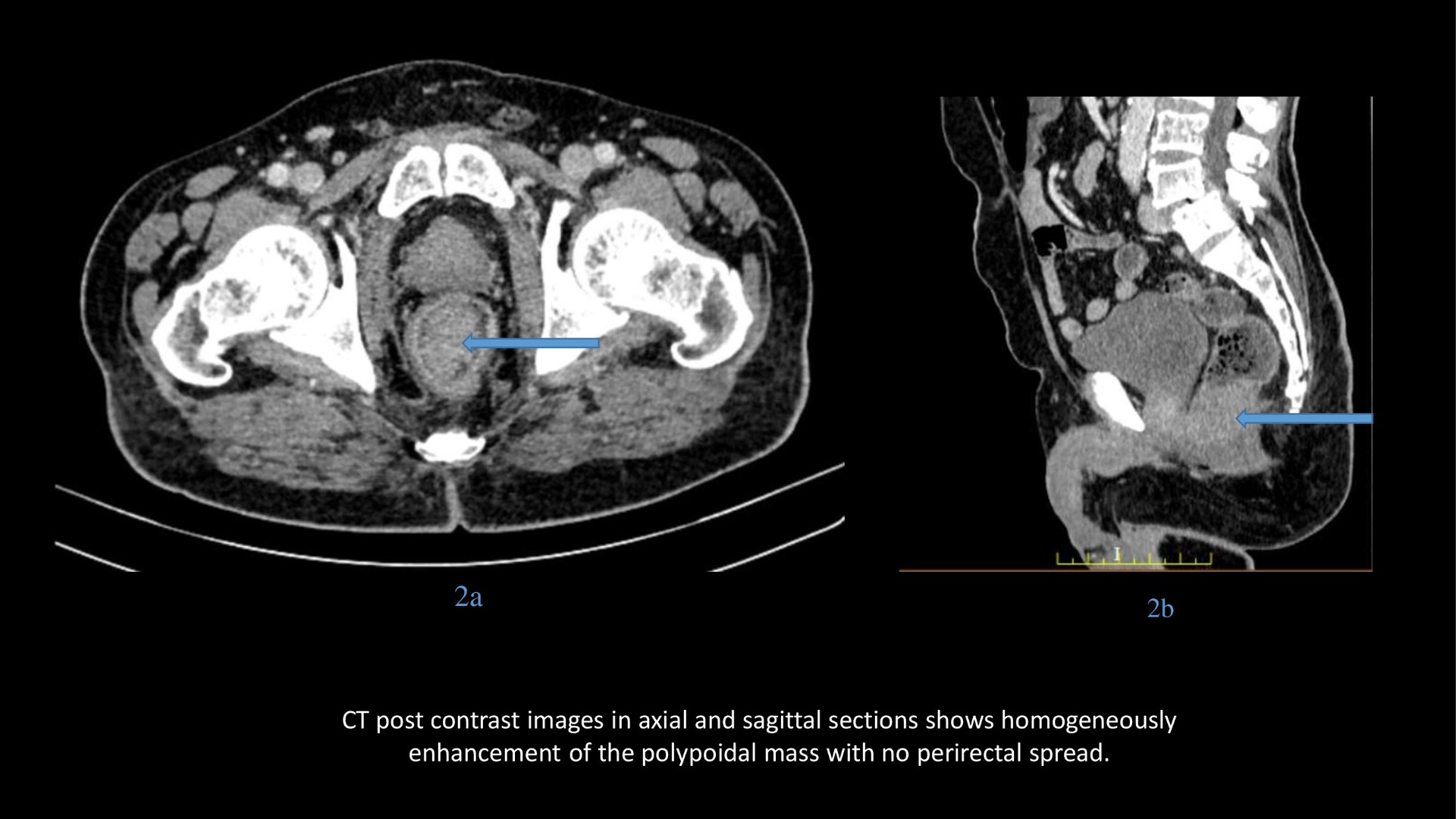
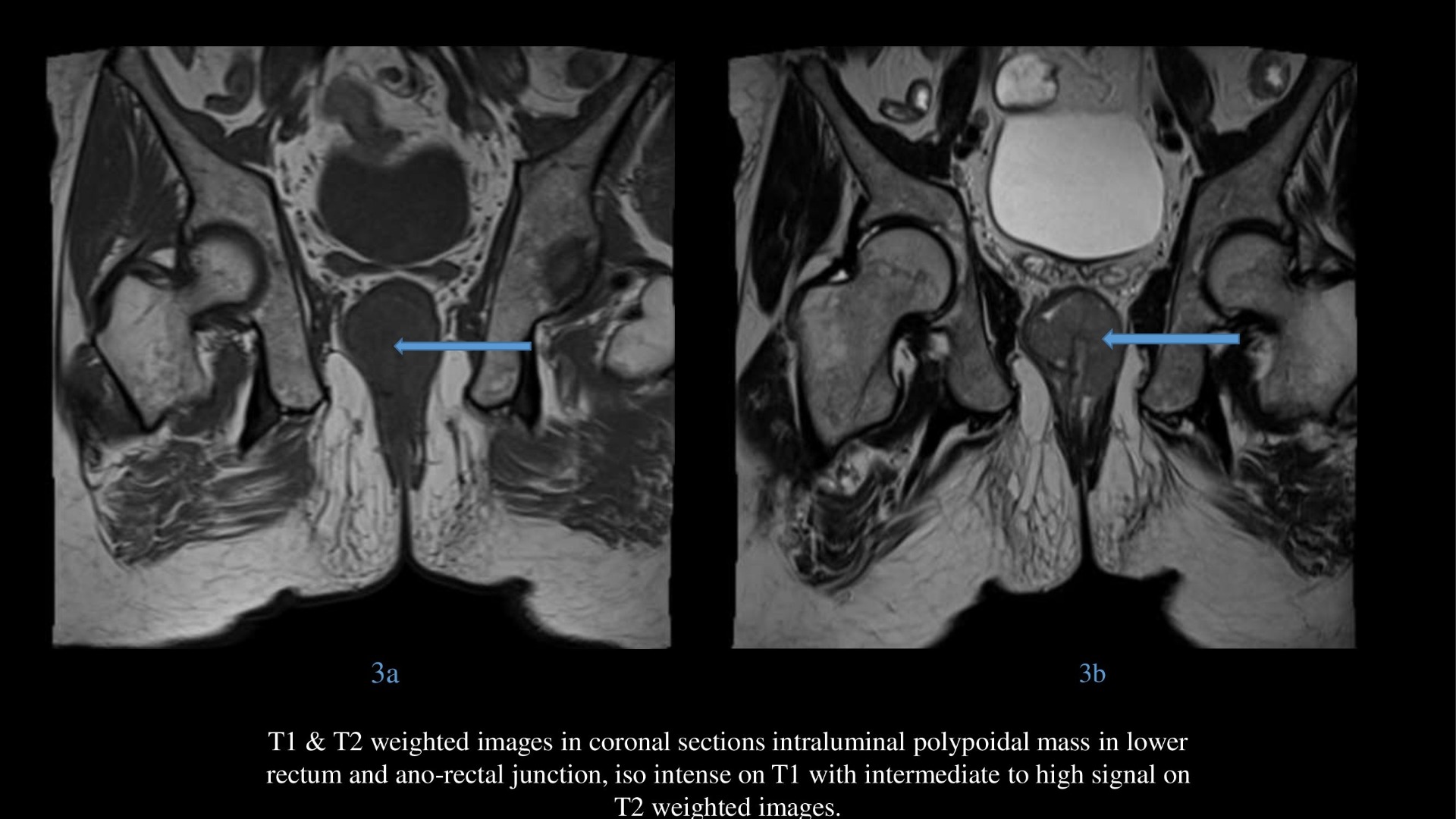
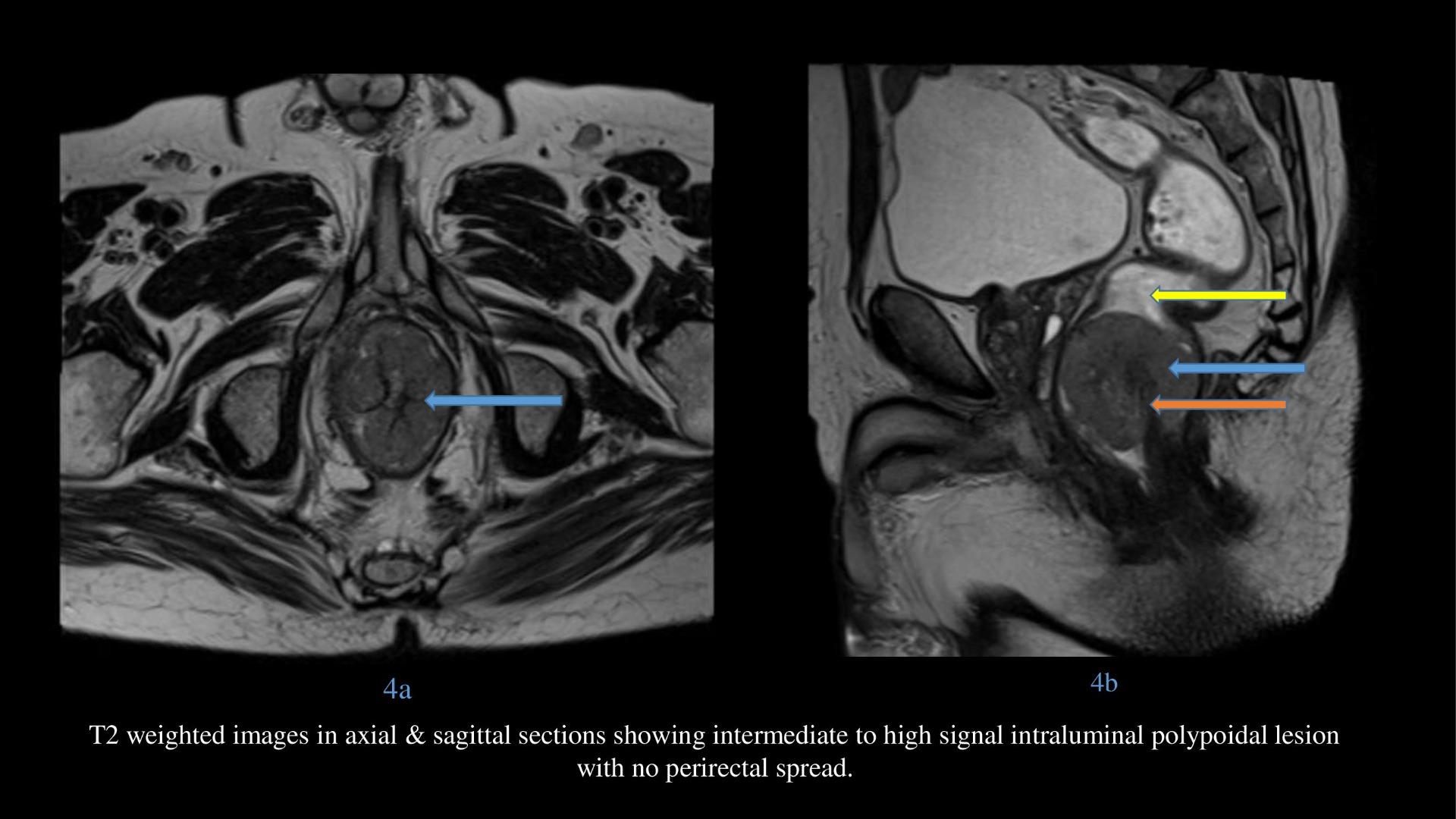
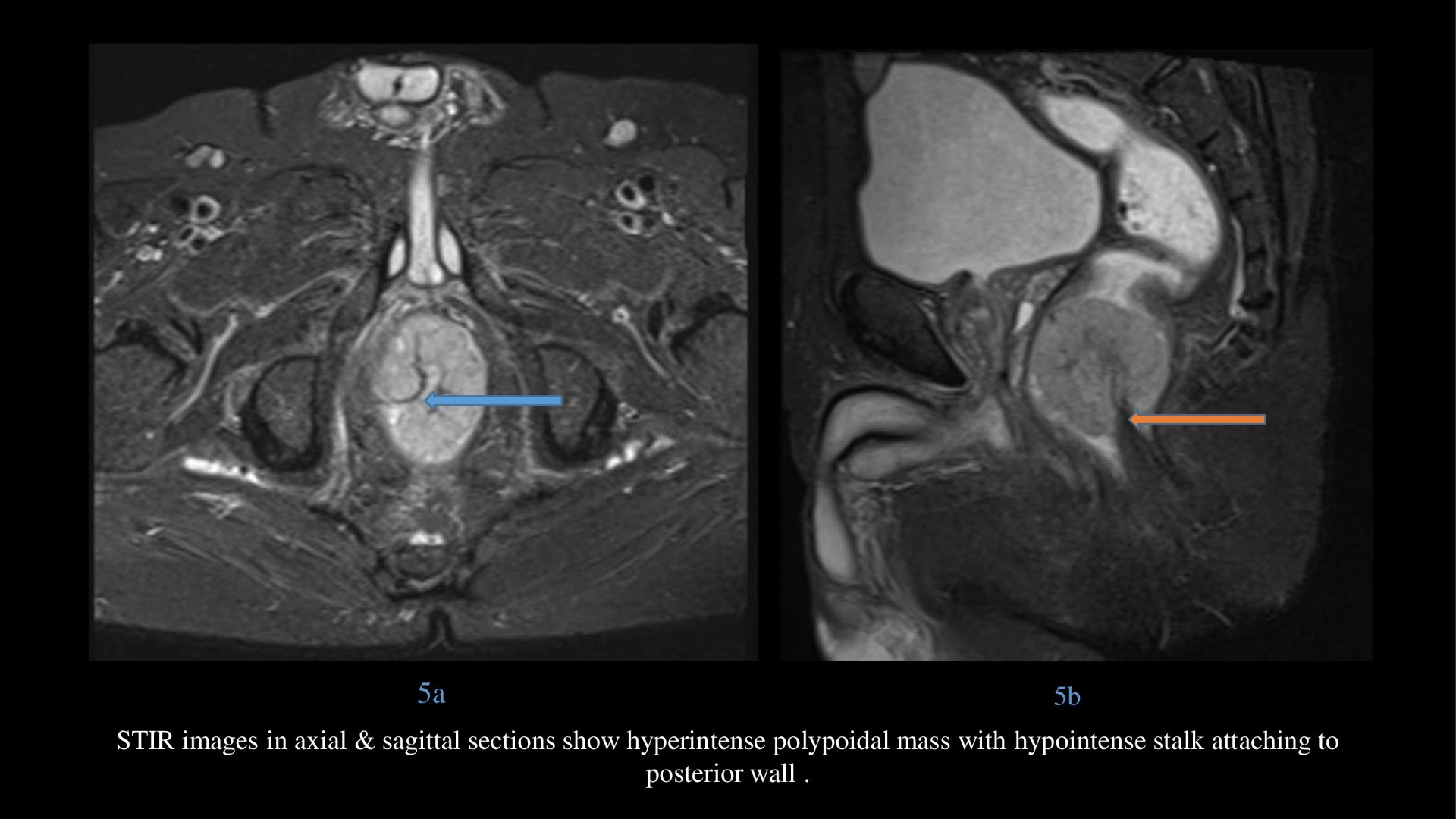
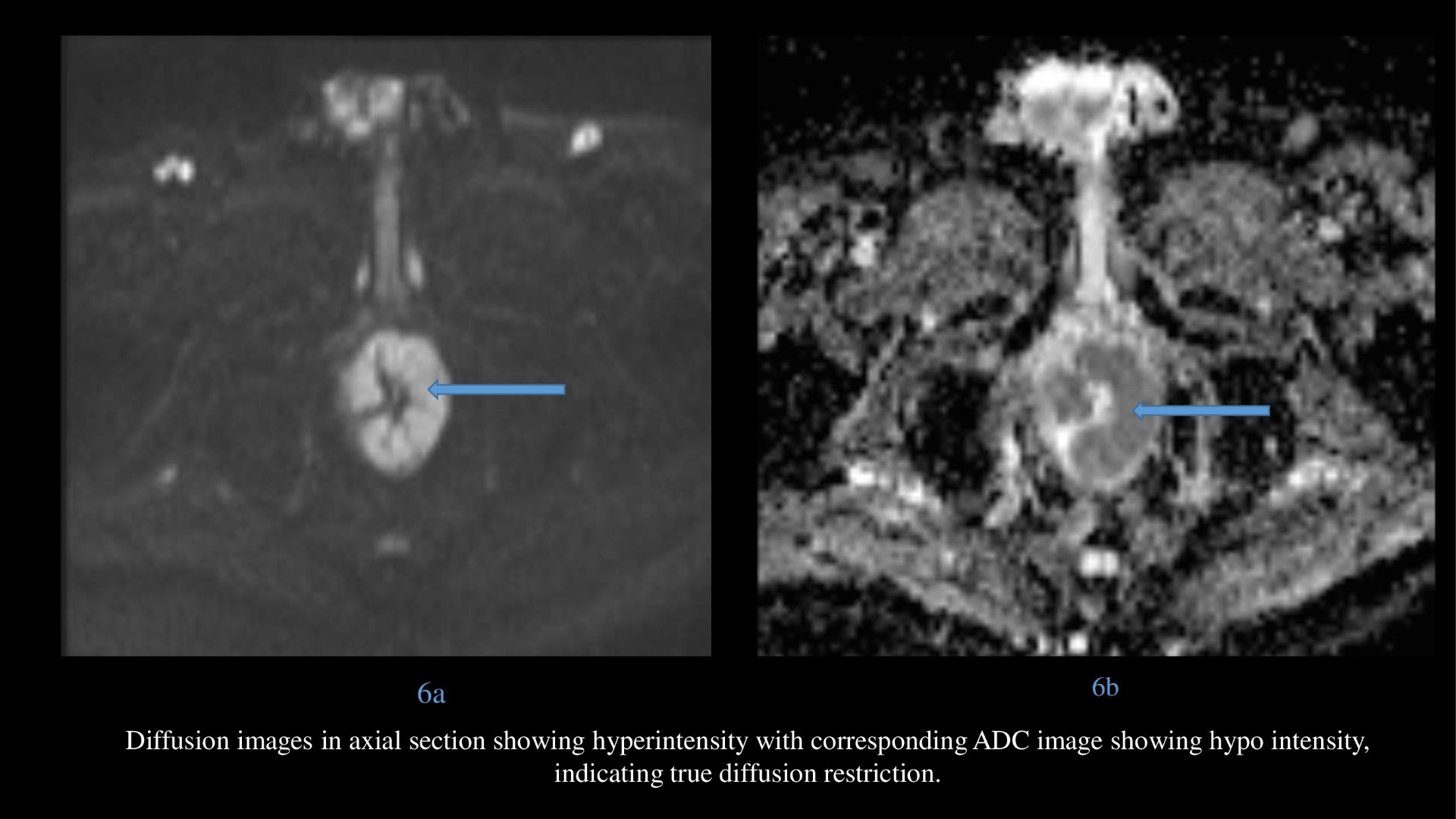
Blue arrow and Yellow arrows:
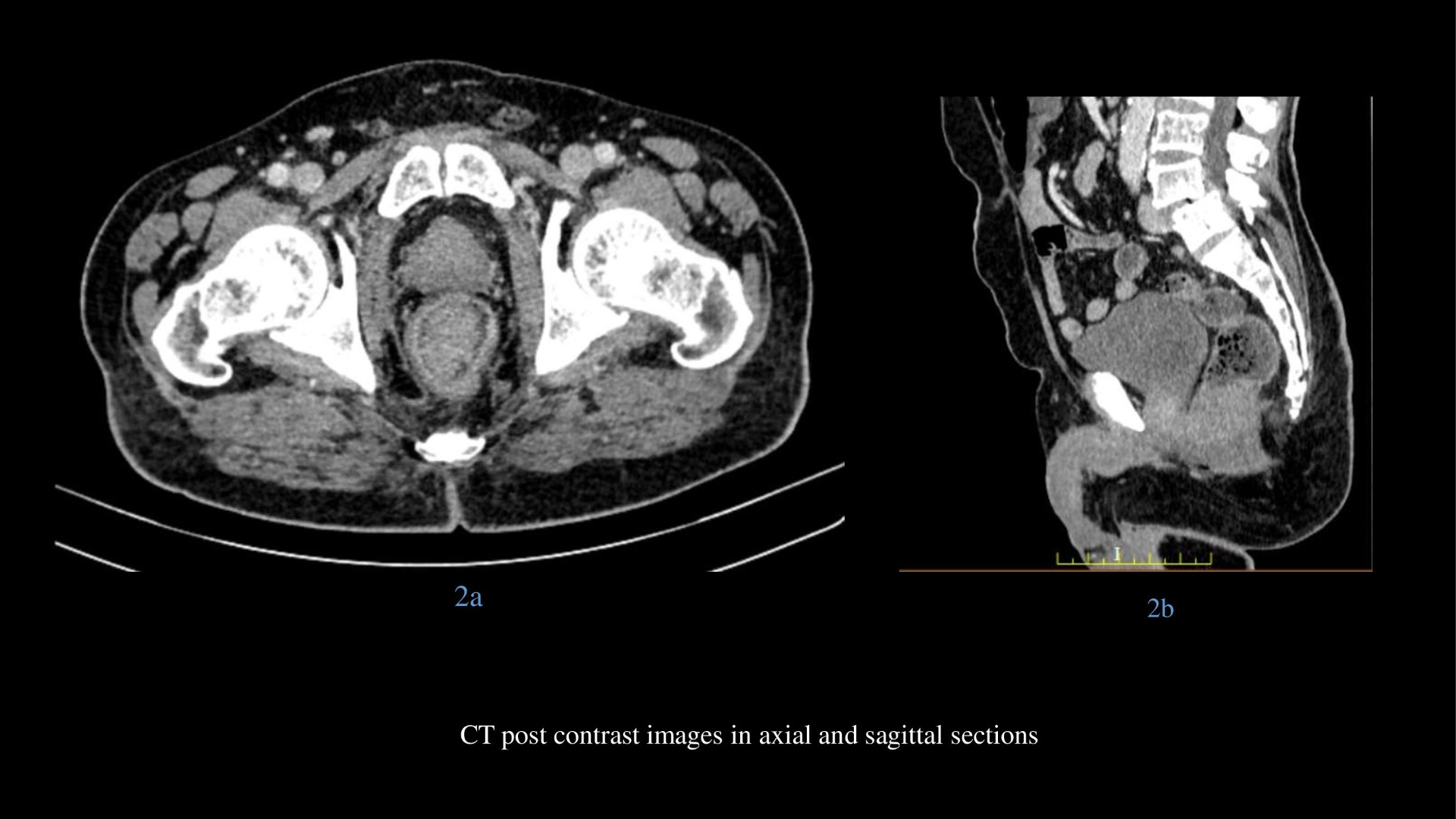
- CT plain and post contrast images in axial and sagittal sections shows polypoidal mass which is homogeneously enhancing without proximal obstruction.
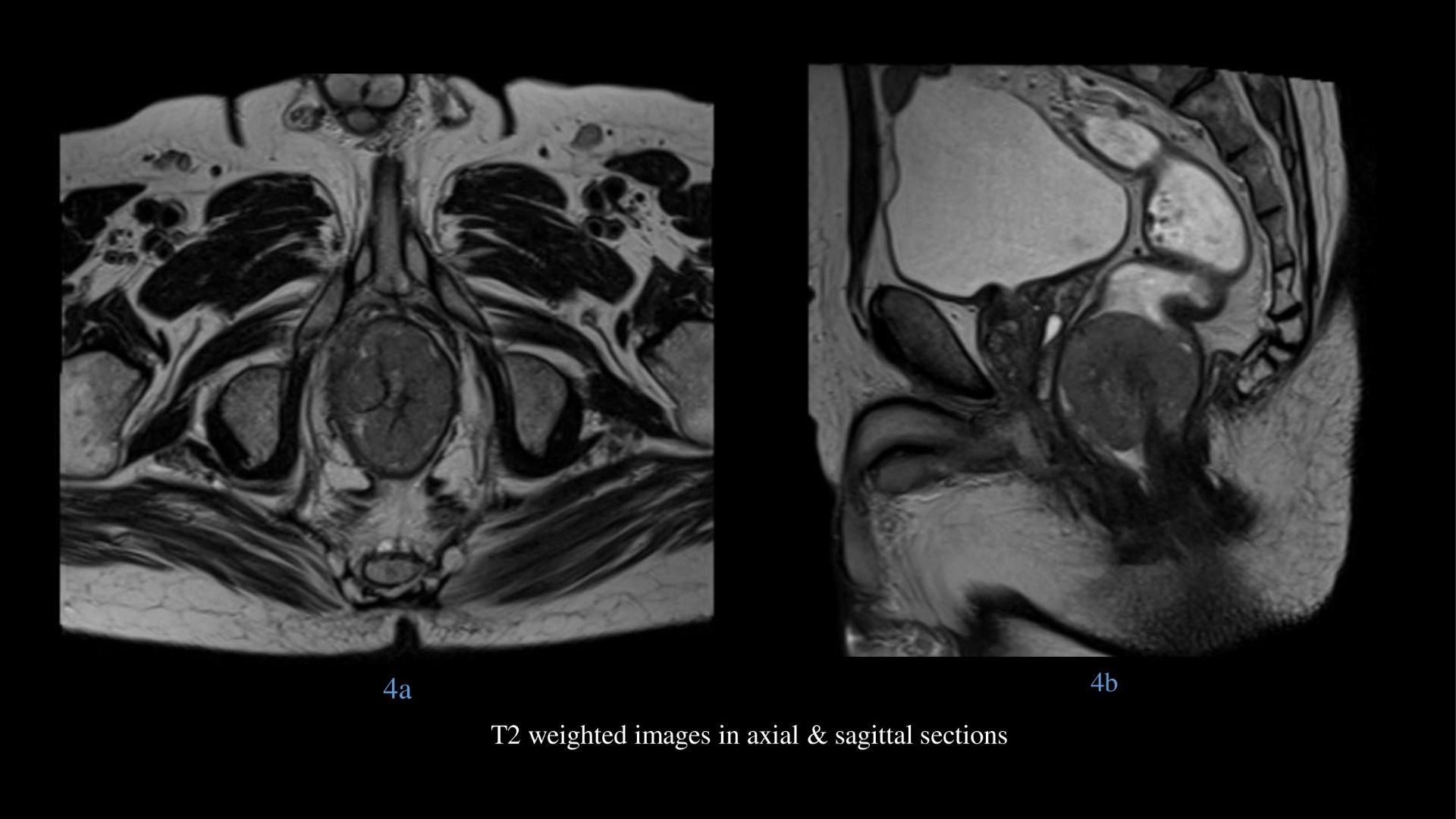
- T2 weighted images in axial & sagittal sections showing intermediate to high signal intraluminal polypoidal lesion at anorectal junction without perirectal spread.
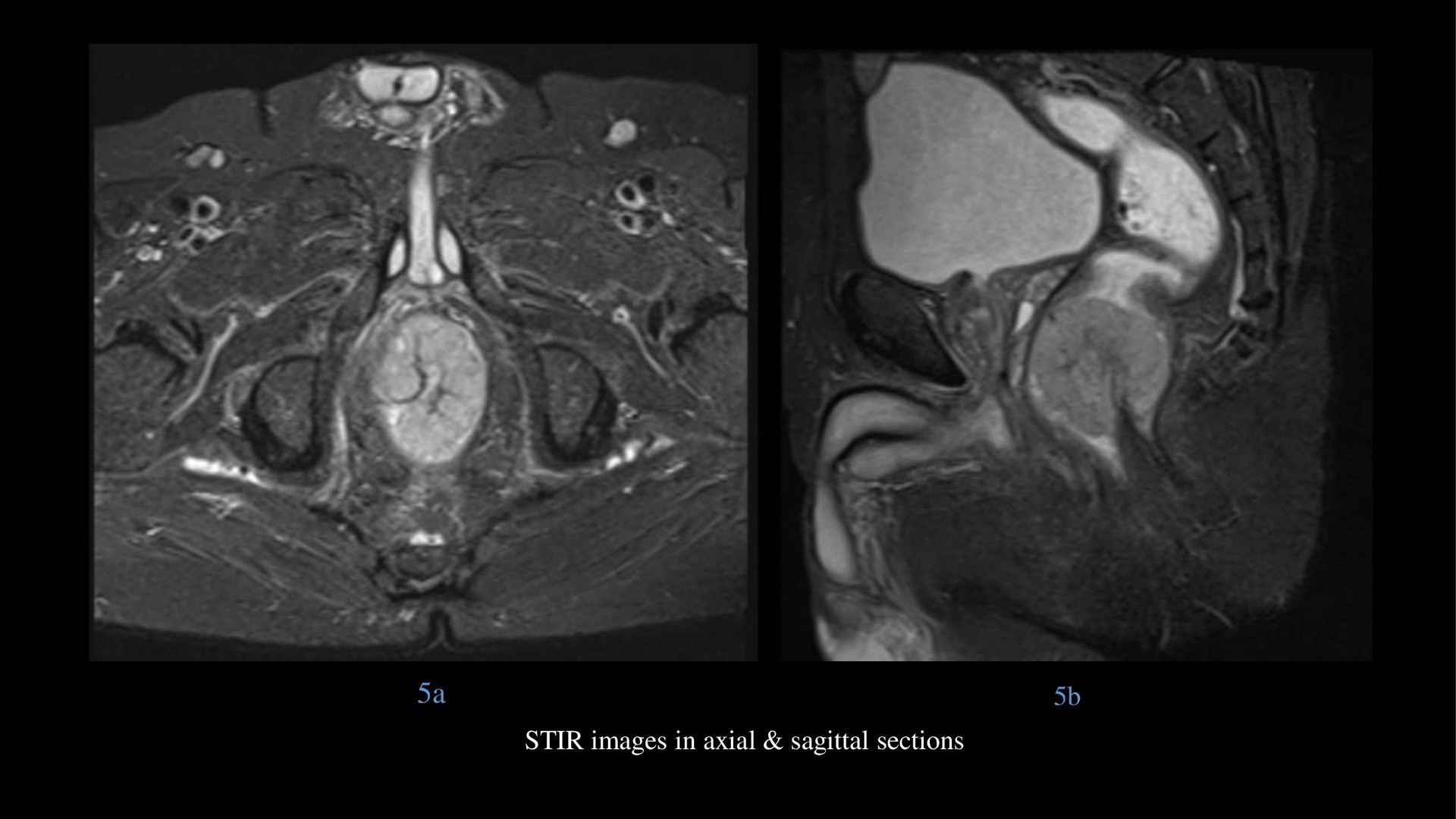
- STIR images in axial & sagittal sections show hyperintense polypoidal mass with hypointense stalk at anorectal junction.
- Diffusion images in axial section showing hyperintense intraluminal lesion with corresponding ADC image showing hypo intensity, indicating diffusion restriction.
Orange arrow – hypointense vascular stalk on T2 weighted and STIR images in sagittal section supplying the lesion centrally.
Diagnosis: Amelanotic Melanoma
DISCUSSION:
Primary anorectal melanoma is rare, comprising only 0.5–5% of all anorectal malignancies, but it is the most common site of primary non cutaneous melanoma in the alimentary tract.
Mean age at presentation: 60–70 years.
Female predominance (female-to-male ratio, 4:1) .
Presentation:
Patients most commonly present with rectal bleeding (in 55% of cases),
Perianal or rectal mass (34%),
Pain (13%).
Anorectal melanoma drains into inguinal and inferior mesenteric lymph nodes, and up to 20% of patients may have gross inguinal lymphadenopathy at presentation.
Approximately one-third of patients have distant metastases at the time of diagnosis, most commonly metastases to the liver, followed by the lungs and then bone.
Pathology:
- Anorectal melanoma arises from melanocytes at the anal transition zone between the columnar epithelium lining the digestive tract and the squamous epithelium.
- Accordingly, most arise either at or slightly above the dentate line and they are rarely rectal in location.
- The tumor is often polypoid and ulcerated.
- Prognosis is poor, with a median life expectancy of 8–19 months and a 5-year survival rate of 6%.
- Surgical management involves either sphincter-sparing wide local excision or abdominoperineal resection requiring a permanent colostomy.
CT findings:
On CT, the tumor usually appears as a fungating or polypoid enhancing intraluminal mass that may focally expand the lumen without causing obstruction.
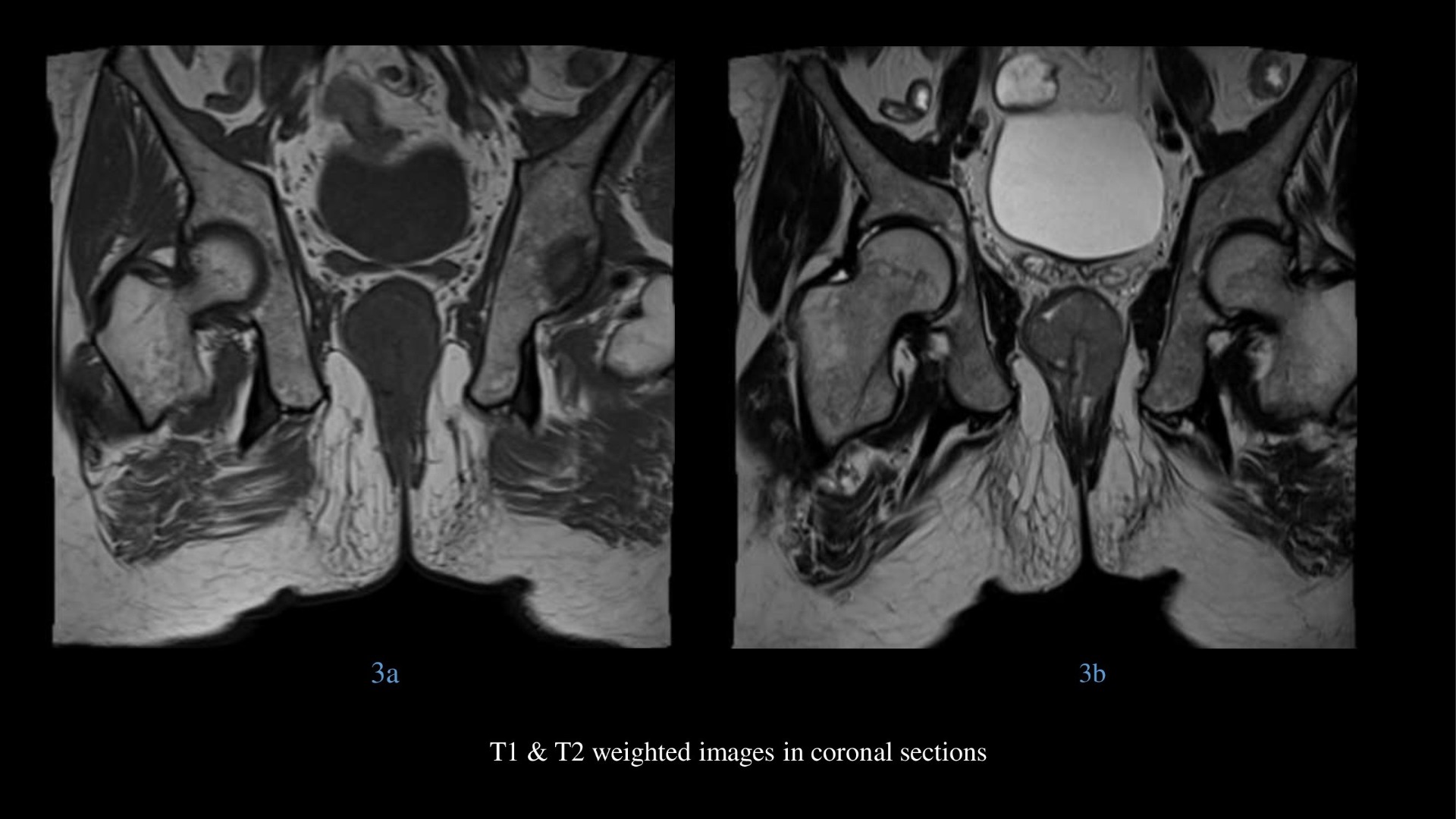
MR Findings:
Melanoma has been reported to show hyperintensity on T1-weighted images and hypo intensity on T2-weighted images. Such findings were noted in most previously reported cases of anorectal melanoma.
However, in amelanotic melanoma, which comprises approximately 20% of all melanomas, these features may be absent.
Lesions may show iso intensity on T1 when compared with pelvic muscles.
Although a considerable number of lesions may show mixed signal intensity on T2-weighted images, some lesions may show high signal intensity.
Lesions may show enhancement and diffusion restriction like other melanomas.
Summary:
- The possibility of the presence of anorectal melanoma should be considered in patients with a bulky intraluminal polypoid mass without colonic obstruction, showing T1 hyperintensity, high or mixed signal T2 intensity, hyper enhancement, minimal perirectal or anal infiltration, and lymphadenopathy.
- Differential diagnosis of Amelanotic melanoma includes Lymphoma, Gastroinstestinal stromal tumor and undifferentiated carcinoma.
- Thus histopathology with immunohistochemistry are essential for correct diagnosis.
References:
- Blecker D, Abraham S, Furth EE, Kochman ML. Melanoma in the gastrointestinal tract. Am J Gastroenterol 1999; 94:3427–3433
- McDermott VG, Low VH, Keogan MT, Lawrence JA, Paulson EK. Malignant melanoma metastatic to the gastrointestinal tract. AJR 1996; 166:809–813
- Meguerditchian AN, Meterissian SH, Dunn KB. Anorectal melanoma: diagnosis and treatment. Dis Colon Rectum 2011; 54:638–644
- Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 1998; 83:1664–1678
- Klas JV, Rothenberger DA, Wong WD, Madoff RD. Malignant tumors of the anal canal: the spectrum of disease, treatment, and outcomes. Cancer 1999; 85:1686–1693
Dr. Srinivas P
Cross-sectional Fellow
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.
Dr. Vishwanath Joshi
Consultant Radiologist.
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.