7 year old, female child presented with intermittent abdominal pain (lasting for 15-20 min), vomiting (4-5 episodes non bilious) and fever for 2 days. Not passed stools since 2 days.
- 7 year old, female child presented with intermittent abdominal pain (lasting for 15-20 min), vomiting (4-5 episodes non bilious) and fever for 2 days. Not passed stools since 2 days.
- Past history - Pain abdomen in March, 2024 - USG abdomen features s/o transient ileo-ileal intussusception, mesenteric lymphadenitis
- PA - Mild distension+, guarding+, tenderness in right lumbar and right iliac region. Pallor+ Temp 101F, HR 180bpm, SpO2 97% RA
- USG- Ascites, inflamed mesenteric fat and probe tenderness in RIF. Suspicion of acute appendicitis.
- CT Abdomen and Pelvis was advised.
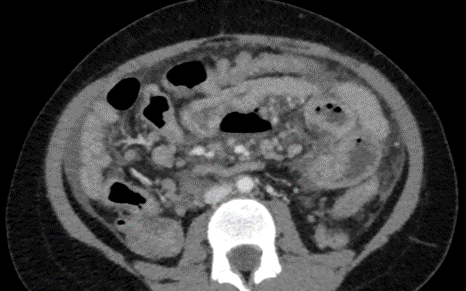
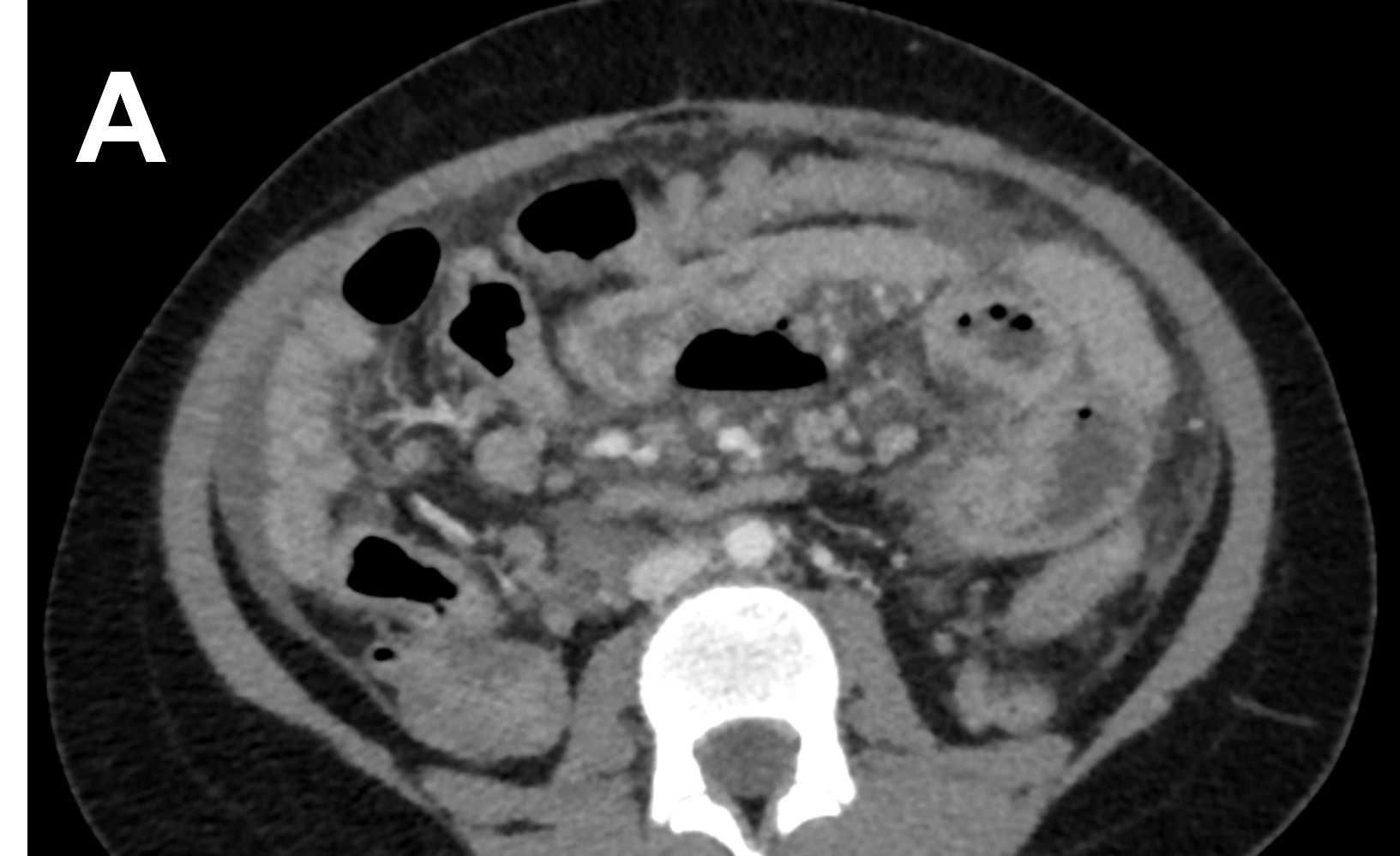
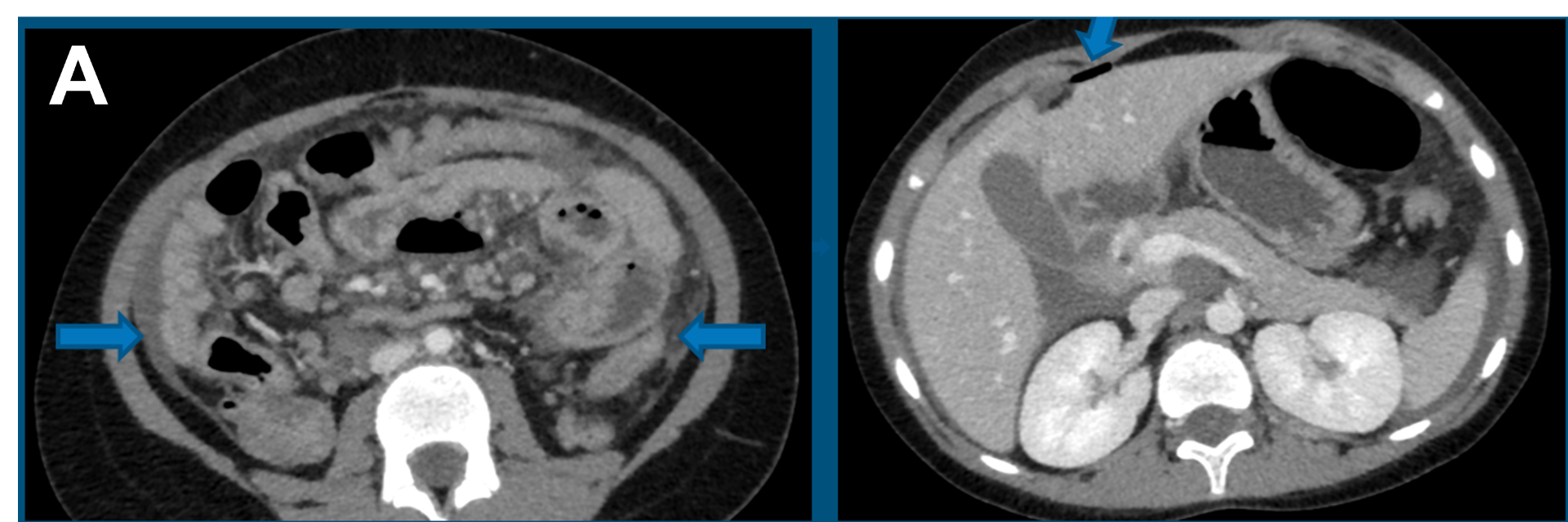
- A. Axial venous phase images
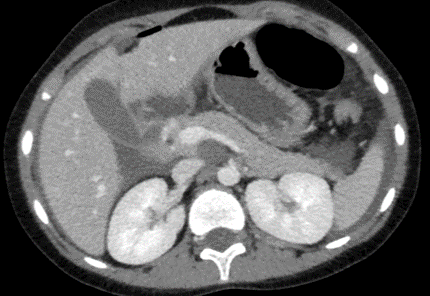
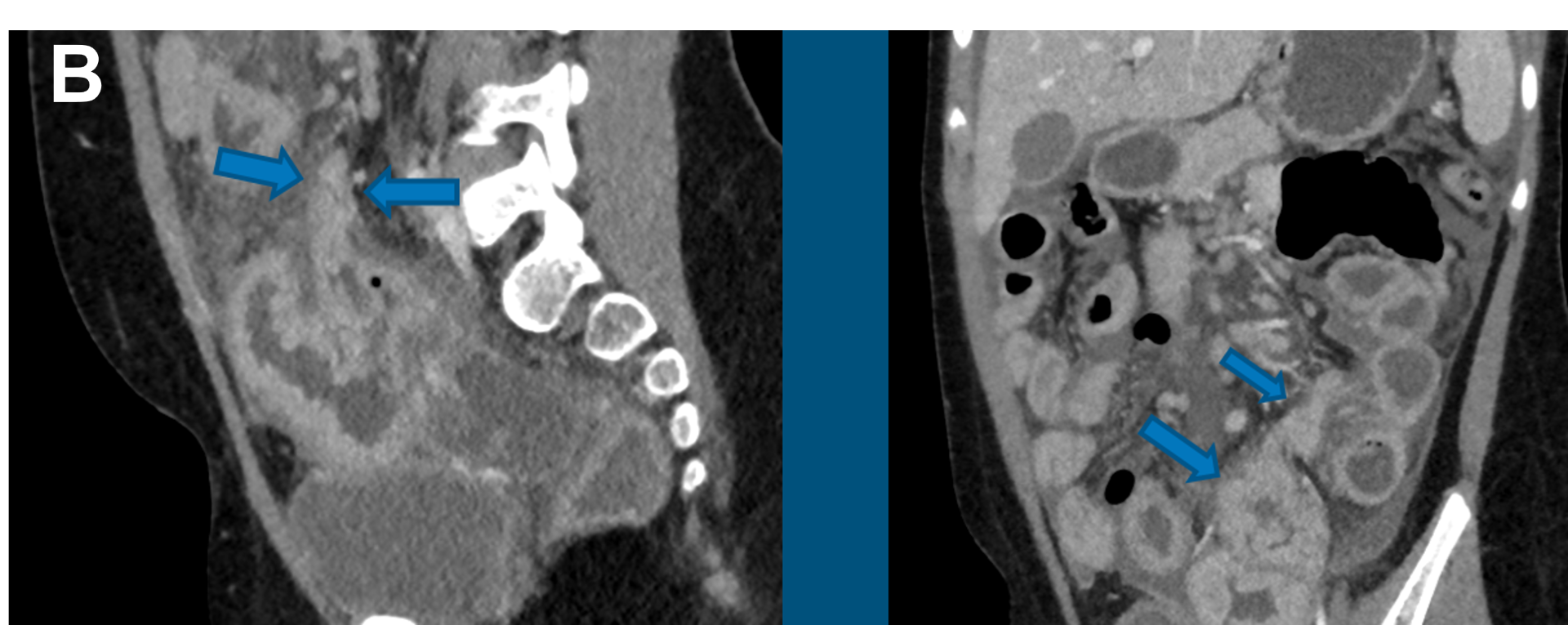
- B. Sagittal and Coronal venous phase images
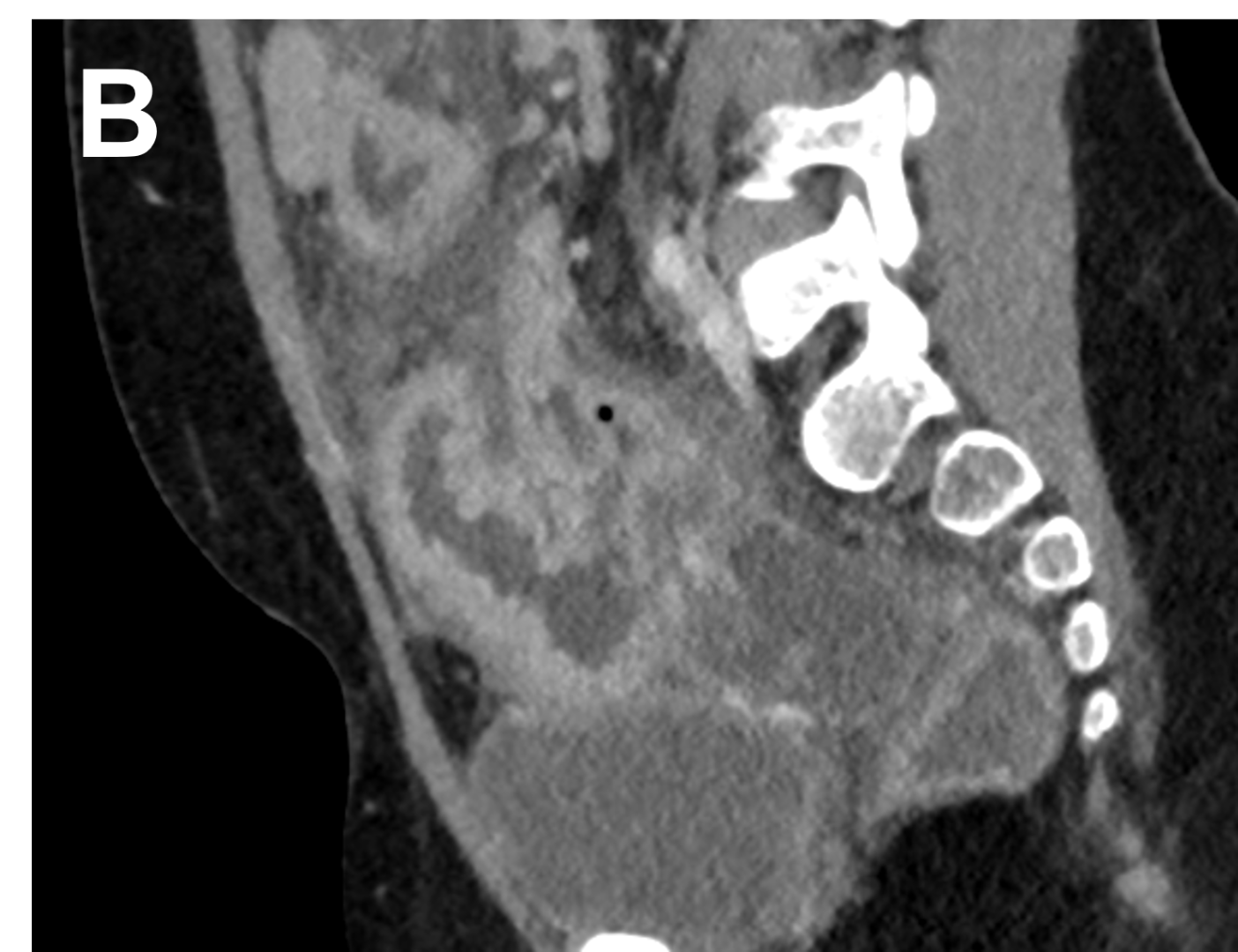
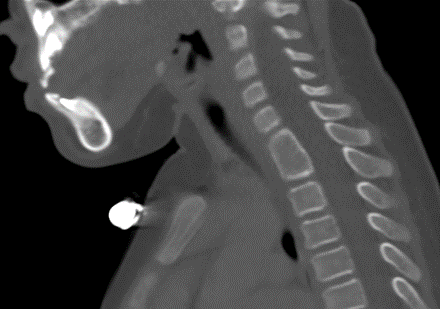
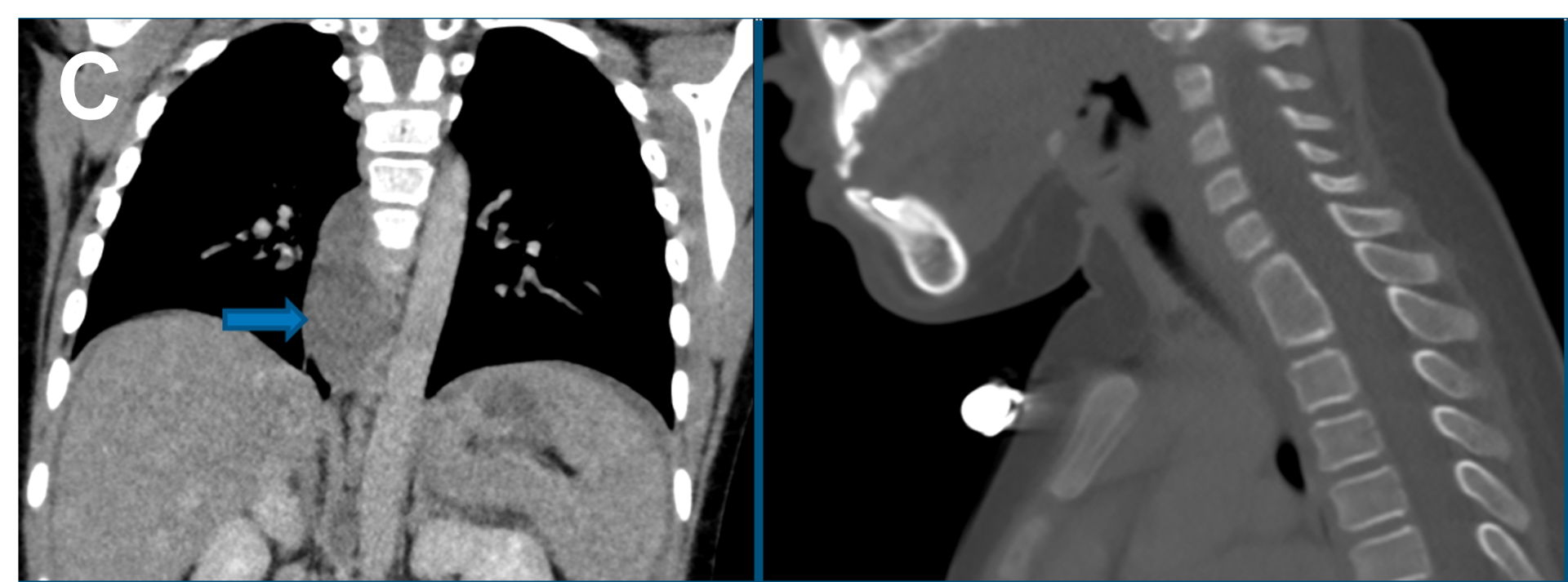
- C. Coronal venous phase chest and sagittal bone window images
- A. Axial venous phase images
- Moderate ascites, diffuse omento-mesenteric fat stranding, enhancing thickening of peritoneal layers – peritonitis.
- Free air - pneumoperitoneum
- B. Sagittal and Coronal venous phase images
- Short segment heterogeneously enhancing thickening with aneurysmal dilation of a proximal ileal loop in left lower abdomen. A blind ending bowel loop like structure arising from the thickened segment of bowel loop - suspicious of a Meckel’s perticulum.
- Pneumoperitoneum, with focal mural discontinuity at the base of this bling ending loop like structure.
- C. Coronal venous phase chest and sagittal bone window.
- Tubular hypodense structure in the paraesophageal location extending from D6 to D10 vertebrae and cervical block vertebrae- paraesophageal cyst/neuroenteric cyst.
Meckel’s diverticulum with perforation peritonitis.
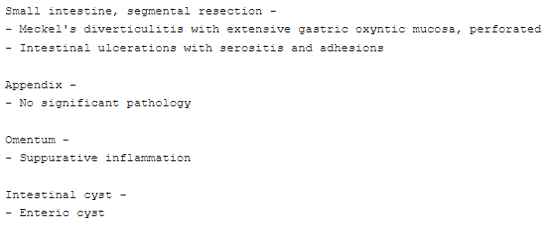
INTRAOPERATIVE
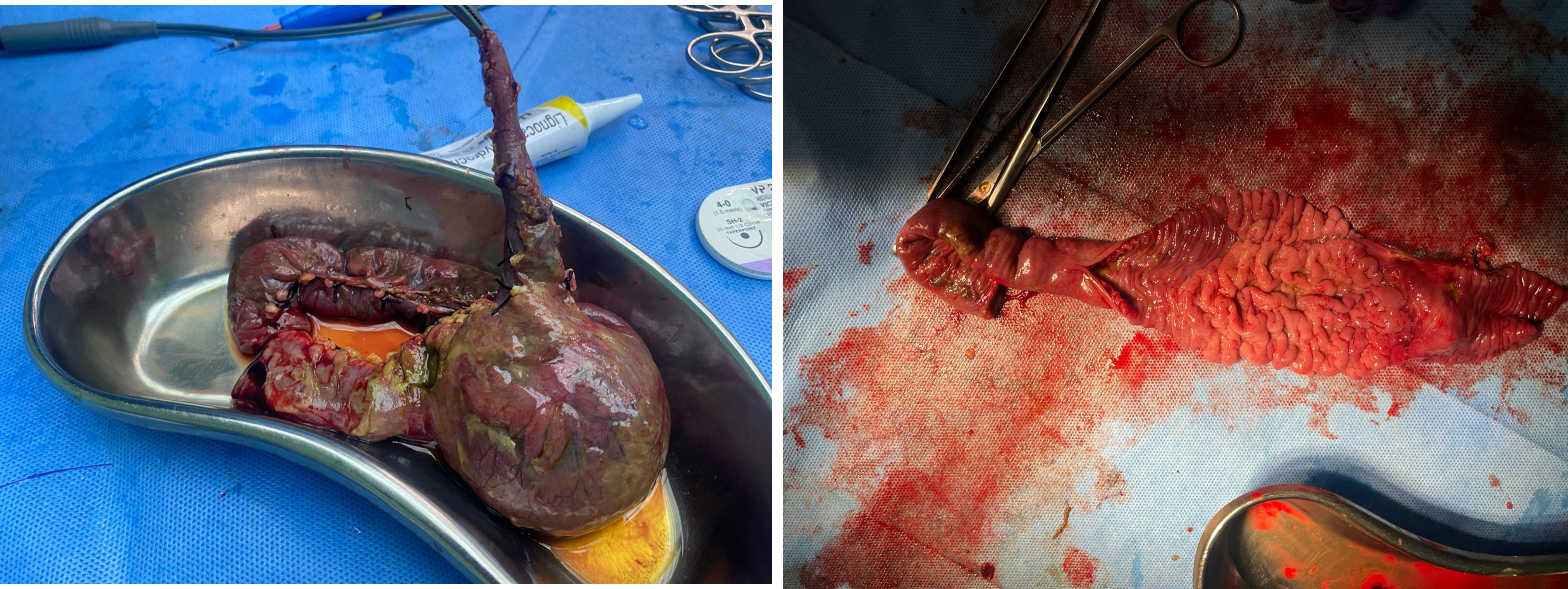
- Patient underwent laprotomy and excision of meckels diverticulum.
HPE
DISCUSSION
- Commonest congenital anomaly of the gastrointestinal tract.
- True diverticulum having all the layers of the intestinal wall.
- Remnant of the omphalomesenteric (vitellointestinal) duct, which in fetal life connects the yolk sac with developing midgut.
- Meckel's diverticulum accounts for nearly 98% of the cases of omphalomesenteric duct anomalies.
- Diverticulum arises from the antimesenteric border of the terminal ileum and is usually supplied by the vitellointestinal artery originating from the ileal branches of the superior mesenteric artery. The diverticulum has a separate fold of mesentery, which carries the supplying vessels.
- Rules of 2” - Meckel's diverticulum occurs in about 2% of the population, it is about 2 inches in length, is usually located within 2 feet of the ileocaecal valve and usually presents before 2 years of age.
- Location of Meckel diverticulum in the ileum varies from patient to patient - closer to the ileocecal valve in infants (30–90 cm) compared with adults (60–100 cm)
- The length of a Meckel diverticulum may measure up to 15 cm. Giant Meckel diverticula are considered to be those more than 5–6 cm in diameter
- Gastric heterotopia is most common, reported in 23%–50% of cases, pancreatic tissue is found in 5%– 16% of cases
- Complications include intestinal hemorrhage, obstruction, intussusception, volvulus, hernia and strangulation.
US
- Ultrasound may show a blind-ending peristaltic loop connected to the small bowel.
CT
- CT may show a fluid- or air-filled blind-ending pouch that arises from the antimesenteric side of the distal ileum.
- It is possible for the diverticulum to invert and appear as an intraluminal polypoid lesion
Treatment
- Surgical removal of a Meckel's diverticulum is the current management of choice in a patient symptomatic for a Meckel's diverticulum or for any of its complications
Dr VIKHYATH SHETTY
Consultant radiologist
Manipal hospital, Yeshwanthpur, Bengaluru.
Dr. NEHA SATHYANARAYANA
Radiology resident
Manipal hospital, Yeshwanthpur, Bengaluru.