67 year old female patient complains of dry cough for 2 months
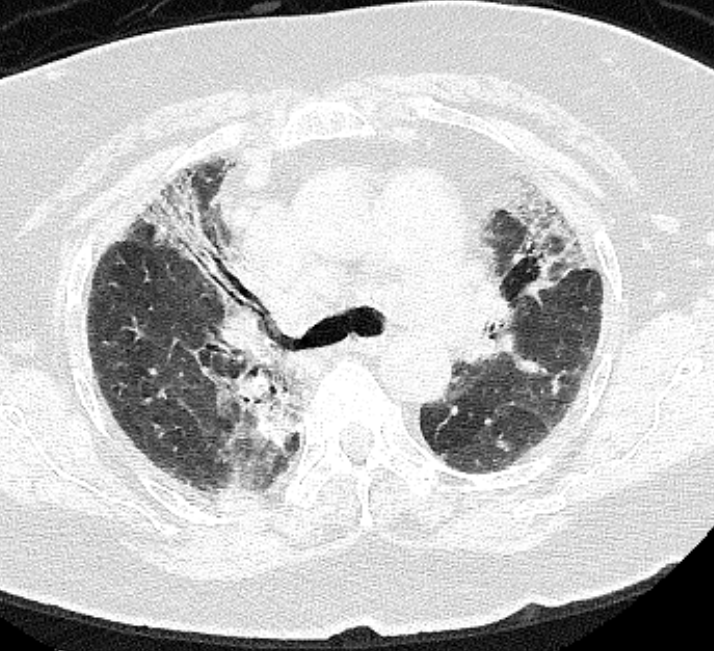
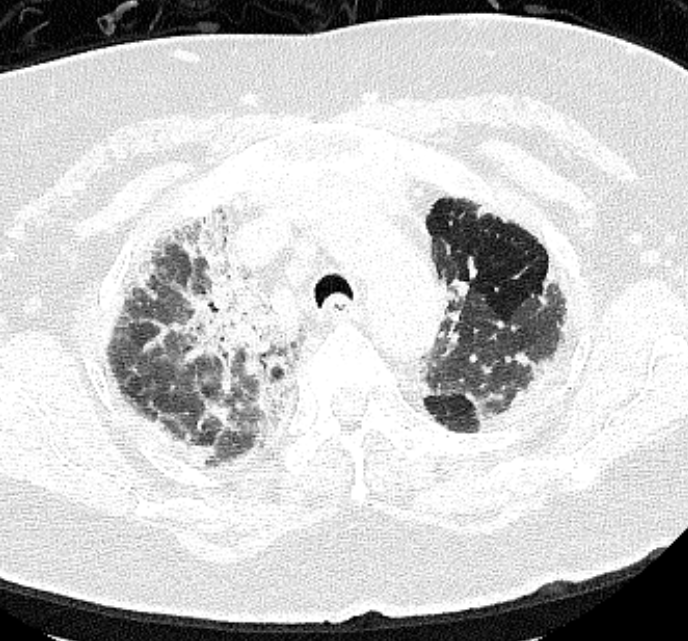
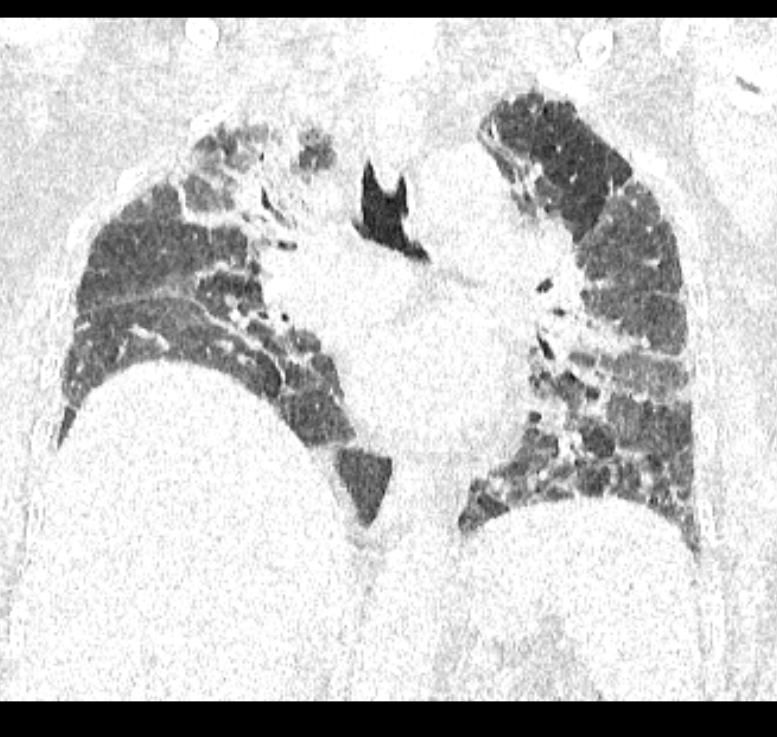
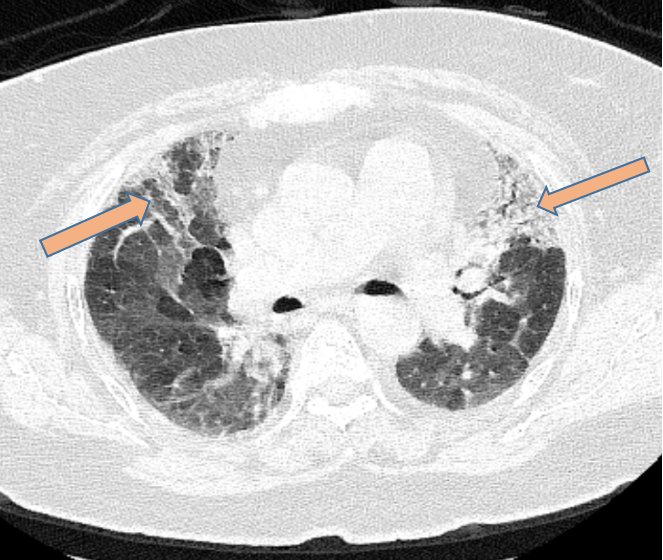
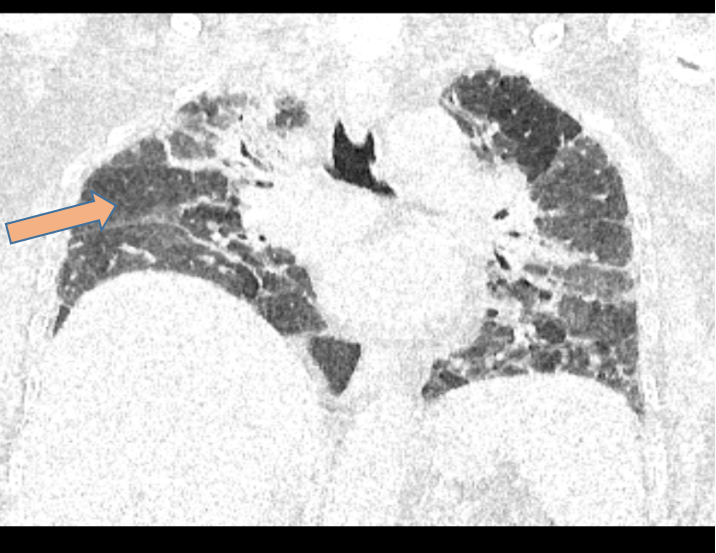
- A and B. Bilateral extensive predominantly peribronchovascular interstitial thickening, fibrosis, architectural distortion and traction bronchiectasis seen, most marked in bilateral upper and right middle lobe.
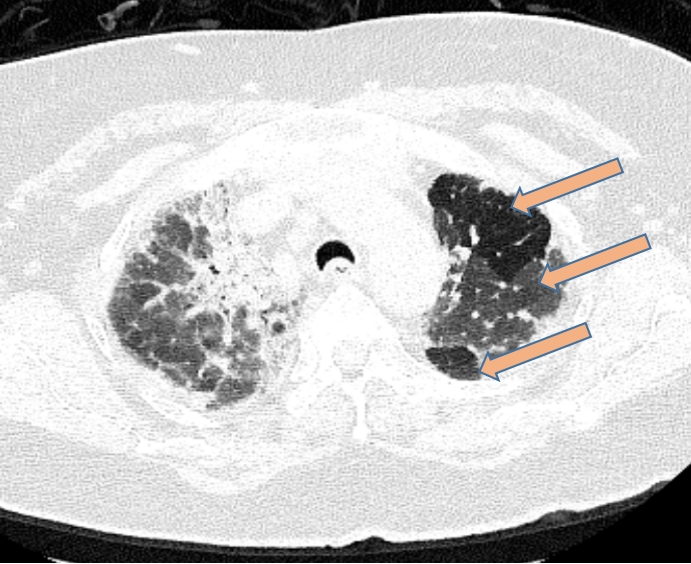
- C and D. Three-density pattern seen with areas of mosaic attenuation, ground glass opacities and normal lung attenuation. There is volume loss in bilateral lungs (Right > Left)
DIAGNOSIS
- FIBROTIC HYPERSENSITIVITY PNEUMONITIS
DISCUSSION
HYPERSENSITIVITY PNEUMONITIS
- HP is typically an immune-mediated disease that manifests as an interstitial lung disease in susceptible individuals after exposure to an identified or unidentified factor characterized by an inflammatory granuloma and/or fibrotic reaction affecting the lung parenchyma and small airways.
- Various specific antigens are responsible for the development of HP including bacterial, fungal, protozoal and animal (usually bird) proteins and low-molecular weight chemicals , drugs, occupational agents (eg, isocyanates, formaldehyde, western red cedar) that can cause hypersensitivity pneumonitis.
- Different HP syndromes are named after the specific environment in which exposure occurs, such as farmer’s lung which is caused by inhalation of specific bacteria or fungi that grow in moist hay or bird fancier’s lung which results from inhalation of avian proteins.
CLINICAL FEATURES
- Acute HP presents with symptoms of cough, dyspnea, wheezing, chest tightness and fever, four to six hours after the exposure to a specific antigen. These symptoms most commonly resolve within hours or days but may return on reexposure.
- Subacute HP is caused by intermittent or continuous exposure to low dose of antigen and is presented with symptoms similar to those in acute phase, but less severe.
- Chronic HP is result of very low level continuous or repeated exposure to antigen with characteristic finding of fibrosis. Affected patients with chronic stage HP present with symptoms of dyspnea, weight loss and general malaise.
DIAGNOSIS
- Evidence of exposure to appropriate antigen by clinical history and clinical improvement following removal of that antigen.
- Bronchoalveolar lavage fluid shows a lymphocytes content of more than 30 % often with increased CD4 - to - CD8 ratio of T cells.
- Characteristic HRCT imaging findings.
- Histopathologic features of HP include cellular bronchiolitis, diffuse lymphocytic interstitial infiltration and noncaseating granulomas.
TREATMENT
- Avoidance of the antigen.
- Systemic corticosteroid therapy.
HIGH-RESOLUTION CT FINDINGS
- Older terms like Acute, Subacute and Chronic hypersensitivity pneumonitis are not now recommended in imaging.
- Radiologically Hypersensitivity Pneumonitis is categorized into two subtypes:
- Non-Fibrotic Hypersensitivity pneumonitis.
- Fibrotic Hypersensitivity Pneumonitis.
Non- Fibrotic Hypersensitivity Pneumonitis
- Patchy or diffuse ground-glass opacities.
- Mosaic attenuation.
- Centrilobular ground-glass nodules.
- Headcheese sign- Combination of patchy ground-glass opacities, normal regions, and air trapping.
- Atypical findings like consolidation and cysts may be seen.
Fibrotic Hypersensitivity Pneumonitis
Confidence in CT models is essential: "typical", "compatible with" and "indeterminate" in fibrotic disease.
- Typical
- Coarse reticulations with lung distortion +/- non-predominate traction bronchiectasis and honeycombing.
- Distribution may be random, midzone predominant or with relative lower zone sparing
- Small airways disease - ill-defined centrilobular nodules and/or GGOs,mosaic attenuation, three density pattern and/or air trapping
- Compatible
- Usual interstitial pneumonia (UIP) pattern
- Extensive GGOs with subtle lung fibrotic changes
- Variant distribution of lung fibrosis in peribronchovascular or subpleural or upper zones
- Small airways disease
- Indeterminate
- UIP pattern alone (i.e. no variant distribution or small airways disease)
- Indeterminate or probable UIP pattern
- Fibrotic non specific interstitial pneumonia (NSIP) pattern
- Organizing pneumonia
DIFFERENTIAL DIAGNOSIS
UIP (Usual Interstitial Pneumonia)
- Subpleural and basal-predominant reticular abnormality (frequently spatially heterogeneous) with traction bronchiectasis.
- Honeycomb cyst formation.
- Absence of features to suggest an alternative diagnosis.
NSIP (Nonspecific Interstitial Pneumonia)
- More ground-glass opacities with frequent underlying reticular abnormality and traction bronchiectasis.
- Honeycombing can be seen but should be mild.
- Lower lung predominance
- Subpleural sparing of the ground-glass opacities.
- Sometimes on followup, fibrosis may assume more of a UIP pattern.
SARCOIDOSIS
- Upper lung predominance
- Fibrosis occurs more central or peribronchovascular distribution and radiate outward from the superiorly retracted hila with substantial upper lung volume loss.
- Air trapping can be seen.
IDIOPATHIC PLEUROPARENCHYMAL FIBROELASTOSIS
- Upper lung predominant fibrosis
- Substantial associated apical pleural thickening.
- Dense subpleural consolidation with associated traction bronchiectasis and upper lobe volume loss.
- May be seen in conjunction with a concomitant UIP pattern.
REFERENCES
- Hirschmann JV, Pipavath SN, Godwin JD. Hypersensitivity pneumonitis: a historical, clinical, and radiologic review. Radiographics. 2009 Nov;29(7):1921-38.Valentino M, Quiligotti C, Carone L. Branchial cleft cyst. Journal of Ultrasound. 2013 Mar;16:17-20.
- Franks TJ, Galvin JR. Hypersensitivity pneumonitis: essential radiologic and pathologic findings. Surgical pathology clinics. 2010 Mar 1;3(1):187-98.
- Glazer CS, Rose CS, Lynch DA. Clinical and radiologic manifestations of hypersensitivity pneumonitis. Journal of thoracic imaging. 2002 Oct 1;17(4):261-72.
- Sahin H, Kaproth-Joslin K, Hobbs SK. Hypersensitivity pneumonitis. InSeminars in Roentgenology 2019 Jan 1 (Vol. 54, No. 1, pp. 37-43). WB Saunders.
- Johannson KA, Elicker BM, Vittinghoff E, Assayag D, de Boer K, Golden JA, Jones KD, King TE, Koth LL, Lee JS, Ley B. A diagnostic model for chronic hypersensitivity pneumonitis. Thorax. 2016 Oct 1;71(10):951-4.
- Vasakova M, Morell F, Walsh S, Leslie K, Raghu G. Hypersensitivity pneumonitis: perspectives in diagnosis and management. American journal of respiratory and critical care medicine. 2017 Sep 15;196(6):680-9.
Dr. DEEPTI H V
CONSULTANT RADIOLOGIST
MANIPAL HOSPITAL , YESHWANTHPUR, BENGALURU
Dr. JOMON SUNNY
FELLOW IN CROSS SECTIONAL IMAGING
MANIPAL HOSPITAL , YESHWANTHPUR, BENGALURU