65 yr old known case of renal failure with altered sensorium ,coma and seizures
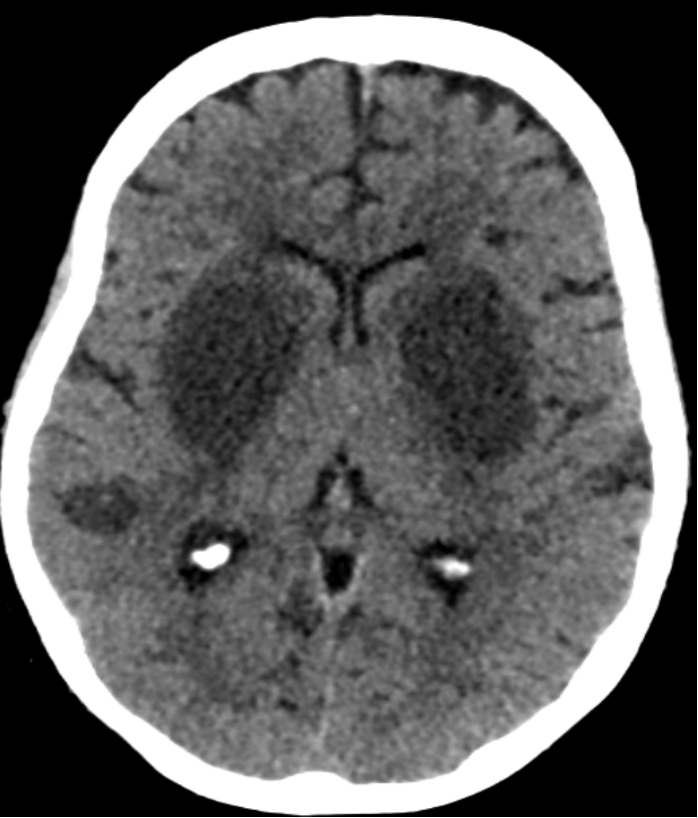
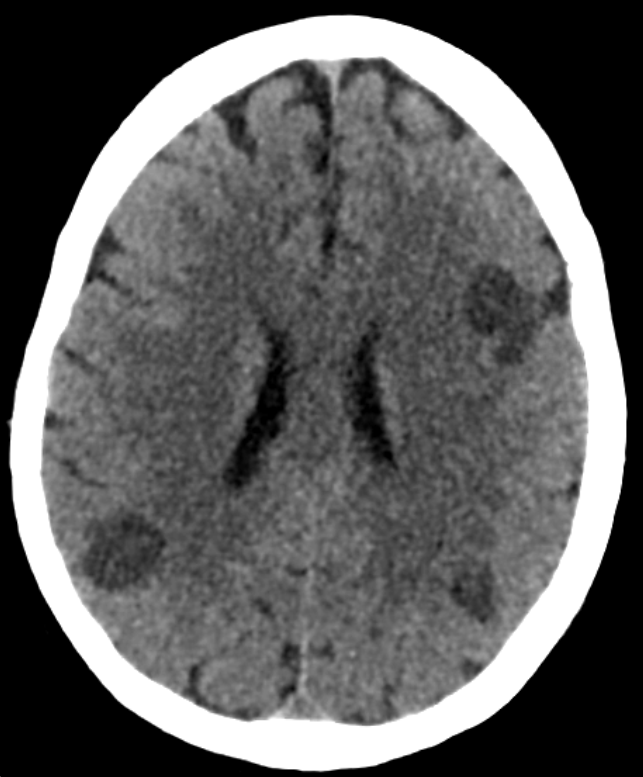
- CT shows symmetrical hypodensities seen in bilateral lentiform nuclei(blue arrows) with few other patchy hypodensities in cortical, subcortical regions of right temporal and bilateral frontoparietal lobes(orange arrows)
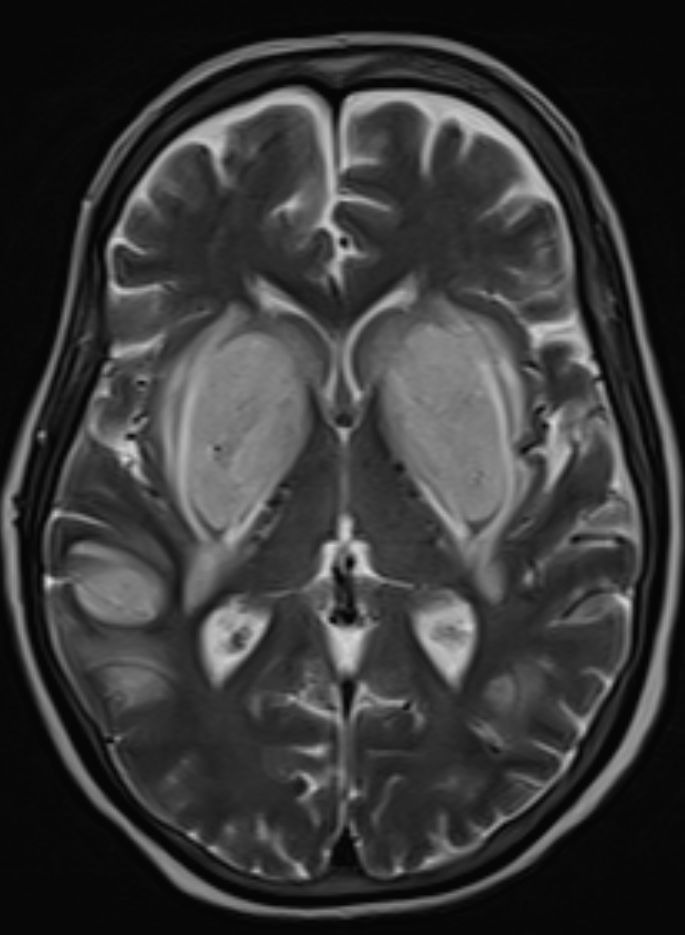
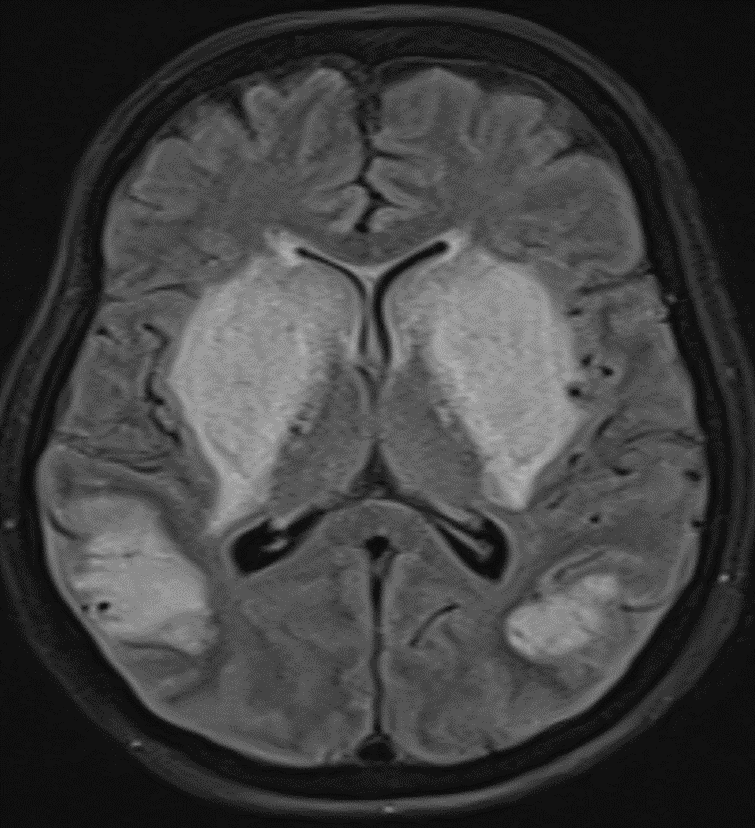
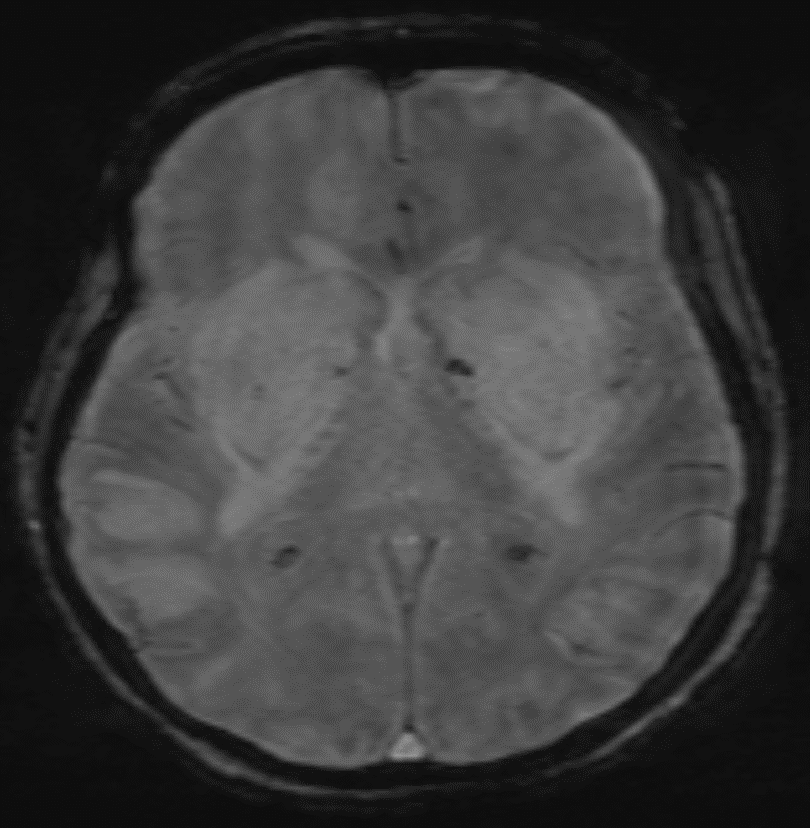
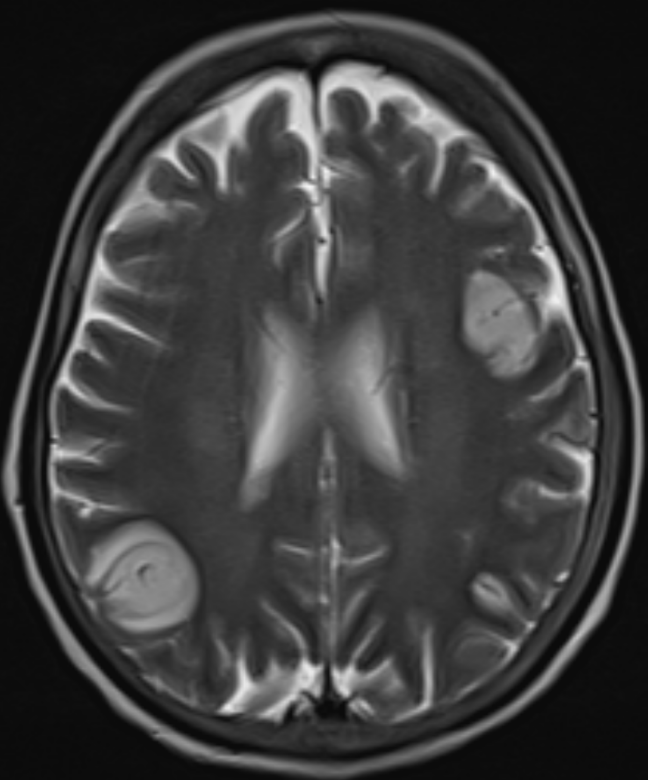
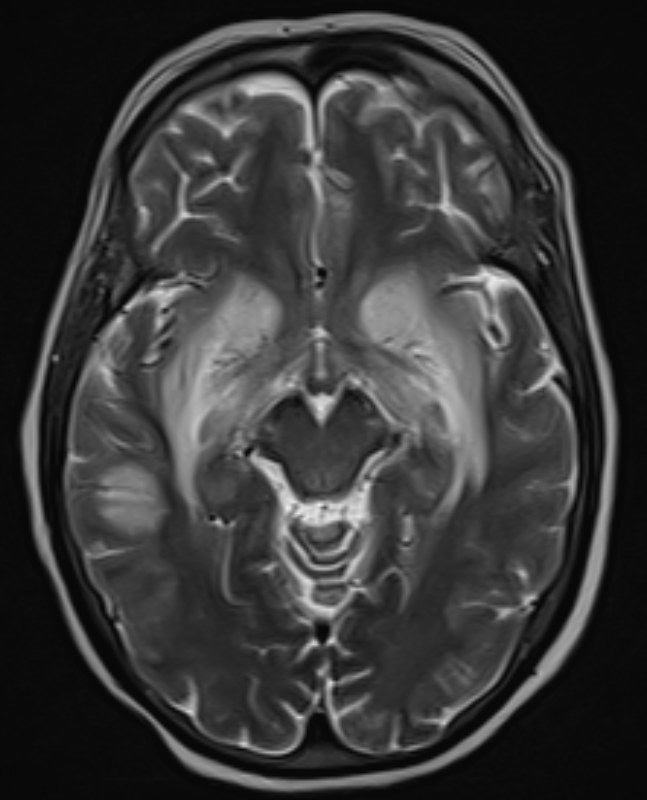
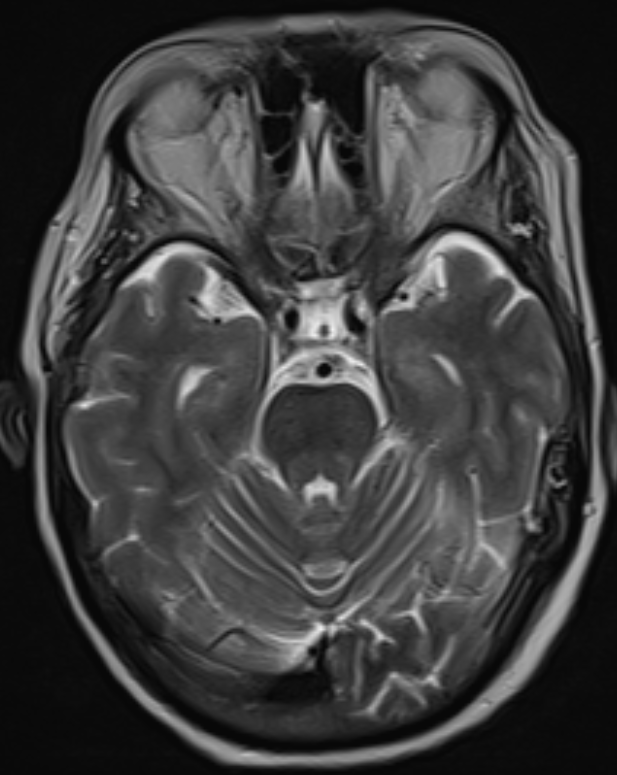
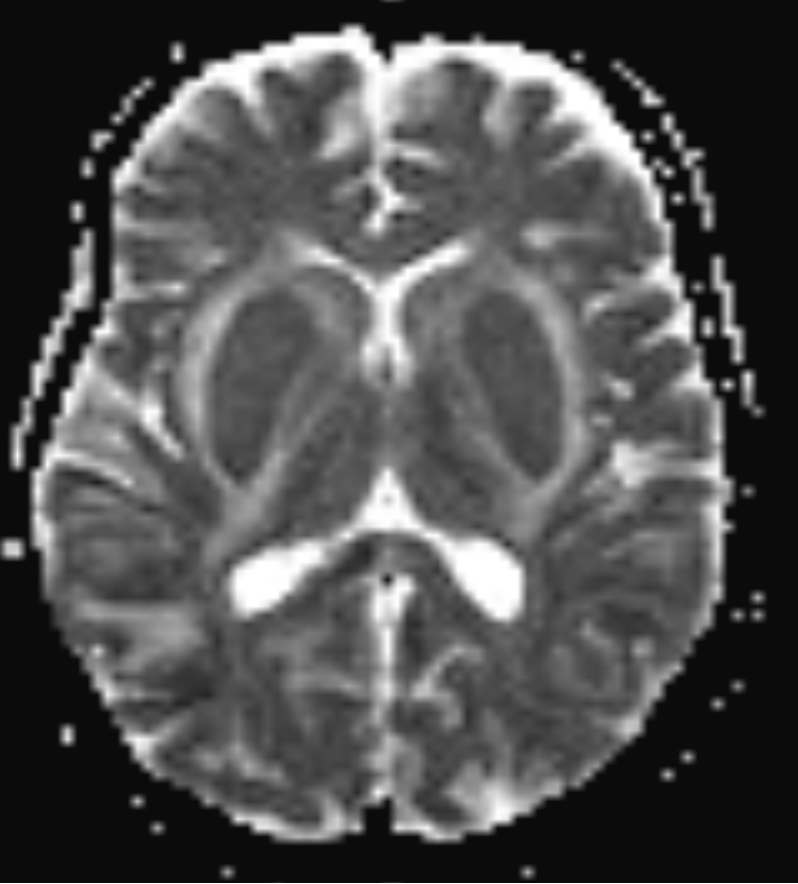
- MRI images show confluent symmetrical T2 and FLAIR hyperintense areas seen in bilateral basal ganglia, lentiform more than caudate(blue arrows) with few other patchy T2, FLAIR hyperintensities seen in cortical, subcortical regions of right temporal and bilateral frontoparietal lobes(orange arrows)
- Hyperintensities involving internal and external capsules bilaterally(green arrows) –indicate lentiform fork sign
- Note made of few tiny SWI blooming areas in left basal ganglia hyperintensity-indicative of microhemorrhage (green arrow)
- No abnormal hyperintensities in the midbrain(blue arrow in C) and pons(green arrow in C)
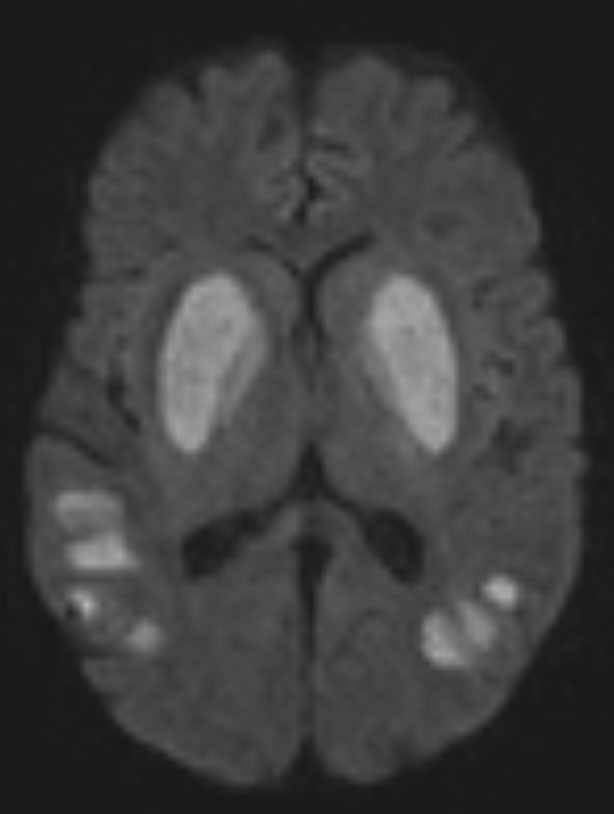
- Evidence of Diffusion restriction within these symmetrical basal ganglia hyperintensities(blue arrows) and in other cortical and subcortical hyperintensities(orange arrows)
Diagnosis: UREMIC ENCEPEHALOPATHY WITH LENTIFORM FORK SIGN
DISCUSSION:
- Uremic encephalopathy(UE) is a neurologic complication resulting from endogenous uremic toxins in patients with severe renal failure.
- The pathogenesis is complex and unclear
- Accumulation of uremic toxins such as guanidine compounds (eg, creatinine and guanidine) might stimulate the neurotoxic effect of excitatory N-methyl-D-aspartate receptors, and concomitant inhibition of inhibitory γ-aminobutyric acid receptors may play an important role in the etiology of UE.
- UE presents 3 patterns of imaging findings:1. basal ganglia involvement 2.cortical or subcortical involvement and 3.white matter involvement.
CT AND MRI DEMONSTRATE:
- On CT typically presents as confluent bilateral hypodensity involving the basal ganglia, thalamus and midbrain. The anatomical boundaries between the deep subcortical grey matter typically appear obliterate.
- On MRI, bilateral T2/FLAIR hyperintensities involving the basal ganglia, thalamus, midbrain and mesial temporal lobes.
- Restricted diffusion may or may not be present to a varying degree, but is not characteristic of uremic encephalopathy.
- Enhancement is not a typical feature.
- Lentiform fork sign(LFS) :The lentiform fork sign is attributed to metabolic acidosis in patients with diabetes and renal failure with a history of incomplete dialysis leading to reversible basal ganglia and adjacent white matter injury . The edematous external capsule represents the lateral arm of the fork, with both the external and internal capsule joining to build the stem of the fork. Edema of the medial lentiform margin forms the medial arm, which splits into two along the medullary laminae to envelop the globus pallidus .
- The lentiform fork sign is reliable in the early diagnosis of uremic encephalopathy, regardless of the presence of metabolic acidosis.
- Cytotoxic edema and/or vasogenic edema on DWI/ADC maps may be associated with uremic encephalopathy.
- Cortical or subcortical lesions of UE are predominantly found in the parieto-occipital lobes
Differential Diagnoses:
- Severe metabolic acidosis
- Ketoacidosis
- Dialysis disequilibrium syndrome
- Intoxication (ie, methanol, ethylene glycol)
- Drug induced (ie, metformin)
REFERENCE:
- Kim DM, Lee IH, Song CJ. Uremic encephalopathy: MR imaging findings and clinical correlation. AJNR Am J Neuroradiol 2016;37(9):1604–1609.
- Narra RK. Lentiform fork sign in uraemic encephalopathy. BMJ Case Rep 2021;14(9):e245623.
- Ishizaki Y, Nishizono R, Kikuchi M, Inagaki H, Sato Y, Fujimoto S. Case Report: A Case of Encephalopathy Presenting the Lentiform Fork Sign on MRI in a Diabetic Dialysis Patient. F1000 Res 2020;9:969
- Kumar G, Goyal MK. Lentiform fork sign: a unique MRI picture— is metabolic acidosis responsible? Clin Neurol Neurosurg 2010;112:805–12 doi:10.1016/j.clineuro.2010.06.006 pmid:20615611
- Grasso D, Borreggine C, Perfetto F, et al. Lentiform fork sign: a magnetic resonance finding in a case of acute metabolic acidosis. Neuroradiol J 2014;27:288–92 doi:10.15274/NRJ-2014-10041 pmid:24976195
Case Contributors:
Dr. SRIRAM PATWARI
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru
Dr. MAYANK M RANGARI
Cross-sectional fellow
Manipal Hospital, Yeshwanthpur, Bengaluru