6 year old female presented with post RTA
FINDINGS
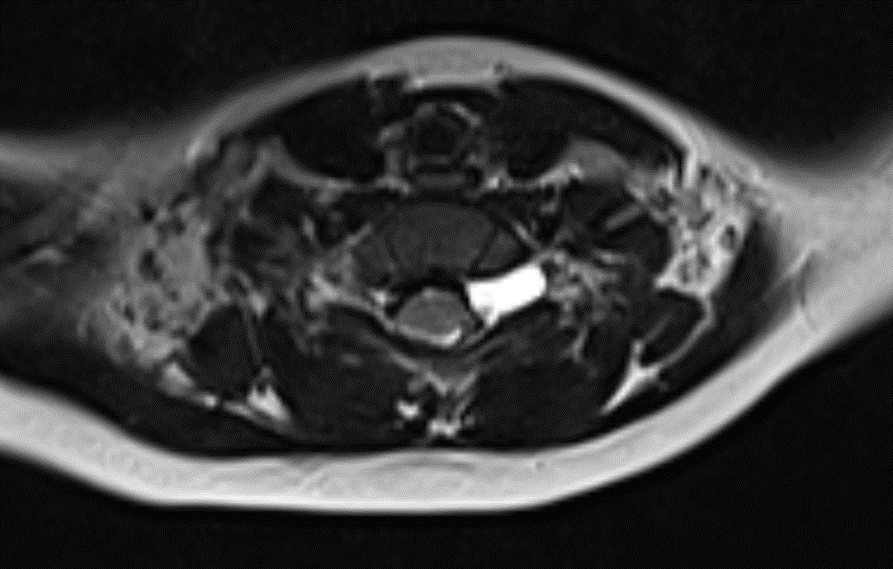
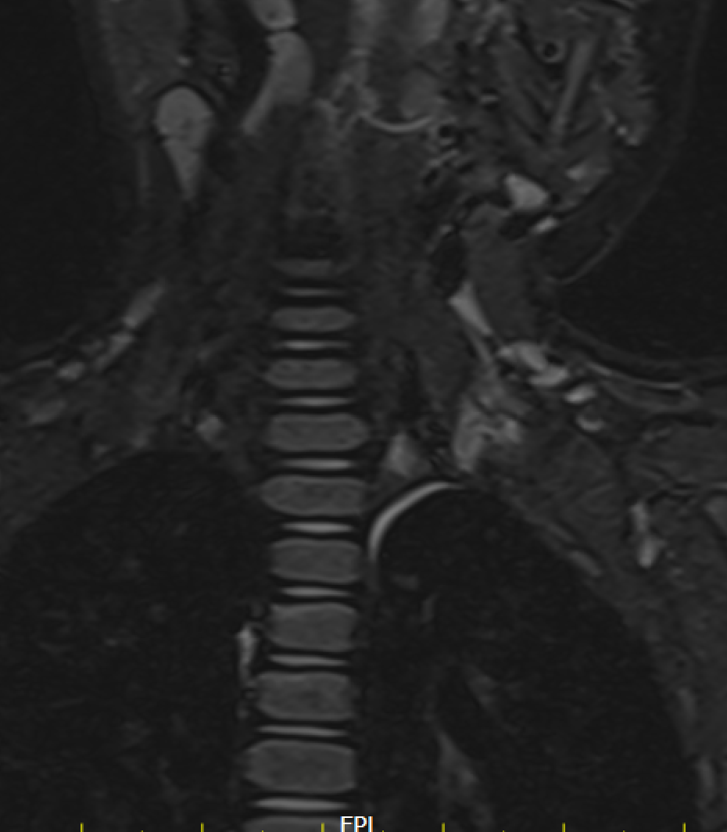
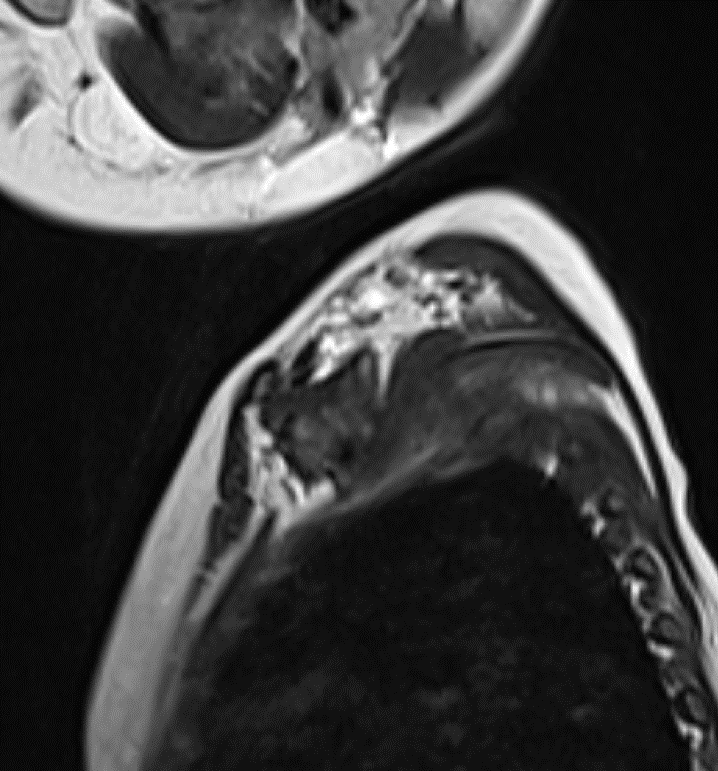
- Shows preganglionic avulsion of C6 ,C7 , C8 ,T1 and T2 ( not completely covered in the images shown) dorsal and ventral nerve roots on left side with pseudomeningocele.
- shows the avulsed nerve roots are clumped up at interscalene triangle.
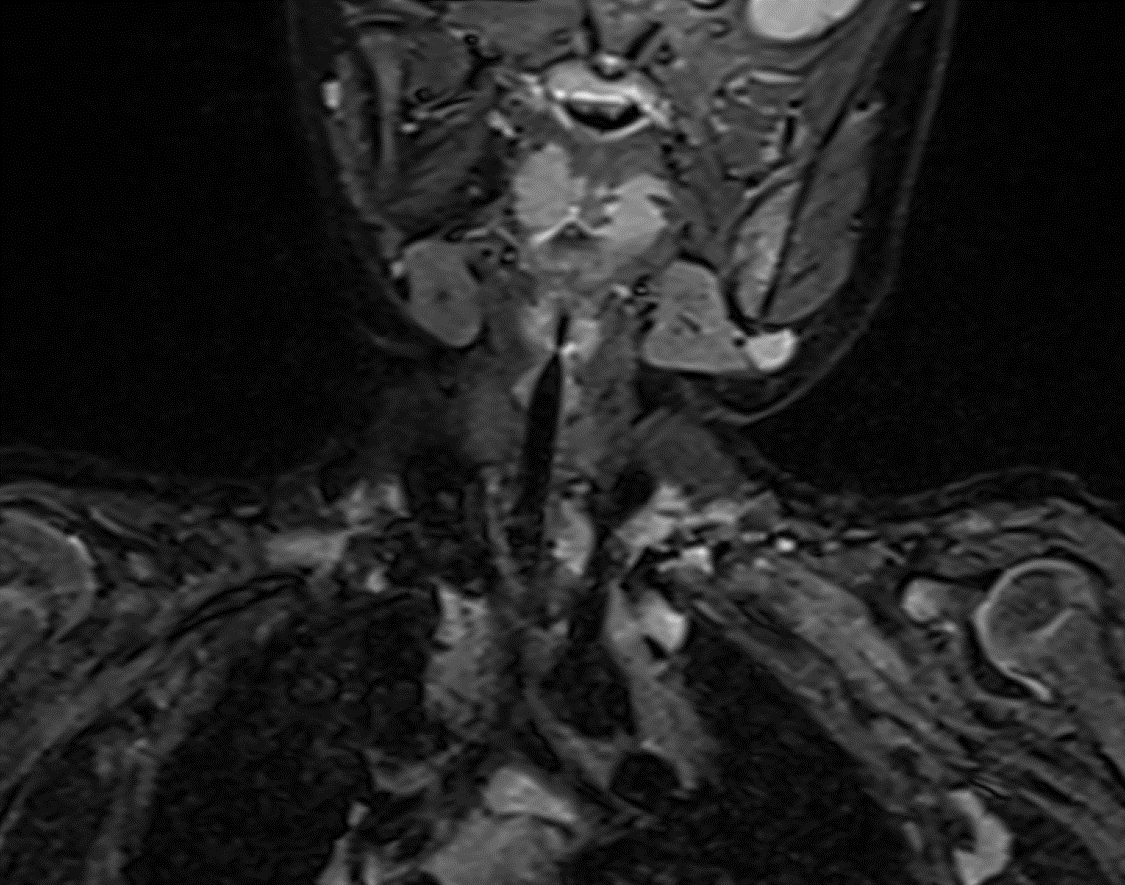
Diffuse swelling and hyperintensity seen involving the roots, trunks and divisions of left brachial plexus with clumping of nerve roots.
No discontinuity of fibres. - T2WI shows clumped divisions of left brachial plexus in costoclavicular triangle.
Diagnosis: Preganglionic nerve root avulsion at C6 to T2 level with Grade III injury of roots, trunks and divisions of left brachial plexus


Companion Case:
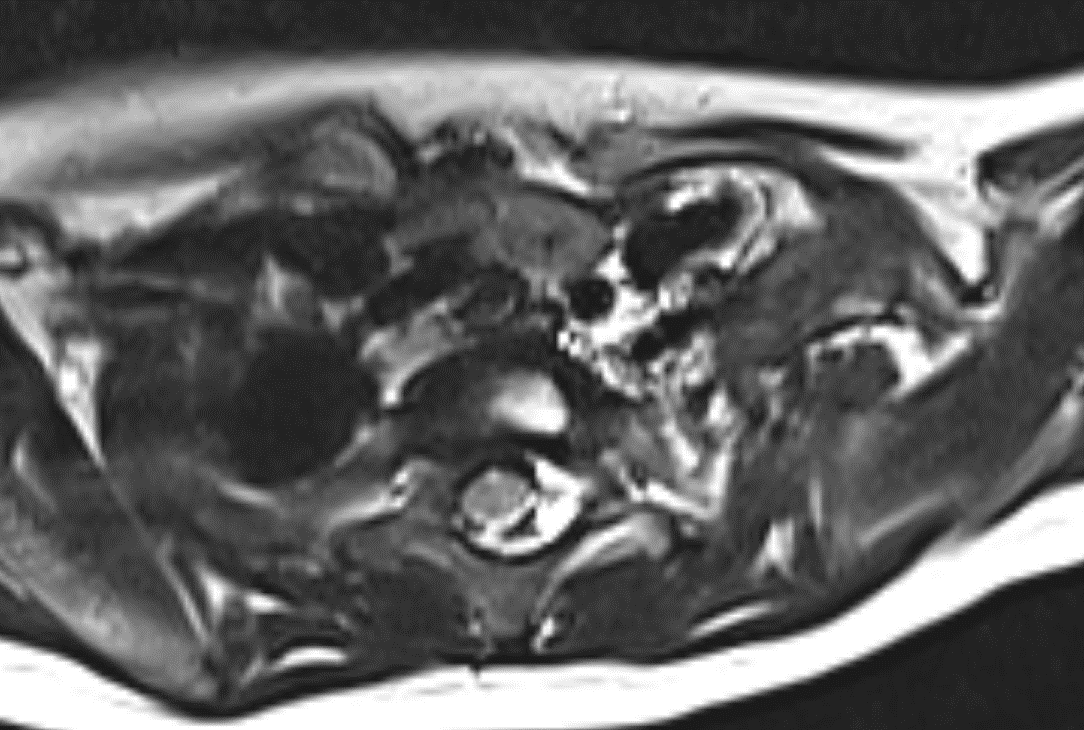
Case of old right brachial plexus injury
Preganglionic avulsion of nerve roots with clumping of nerve roots at interscalene triangle .
No pseudomeningocele
Atrophy of right shoulder girdle muscles.
DISCUSSION:
- Brachial plexus injuriesare a spectrum of upper limb neurological deficits secondary to partial or complete injury to the brachial plexus, which provides the nerve supply of upper limb muscles.
CLINICAL PRESENTATION:
- C5/C6 involvement leads to paralysis of shoulder and biceps muscles
- C7 is involved, paralysis extends to wrist and hand muscles
- C8/T1 involvement leads to paralysis of the forearm flexors and hand intrinsic muscles
CLASSIFICATION:
In the simplest form, brachial plexus injuries can be classified as preganglionic or postganglionic. Each injury has very different management and prognosis.
Preganglionic
- Injury proximalto the dorsal root ganglion, therefore, affecting the CNS which does not have the capacity to regenerate
e.g. nerve root avulsion
Postganglionic
- distalto the dorsal root ganglion affecting the PNS which does have some capacity to regenerate
e.g. nerve ruptures with discontinuity or continuous nerve fibres with mild injury
RADIOGRAPHIC FEATURES
CT myelography
Indications
- gold standard for defining level of nerve root injury
- avulsion of cervical root causes dural sheath to heal with meningocele
- scan should be done 3-4 weeks after injury
MRI
Indications
- suspect injury is distal to nerve roots
- can visualize much of the brachial plexus
Findings
- Traumatic neuromas and edema consistent with injury
- Pseudomeningocele (T2 highlights water content present in a pseudomeningocele)
- Empty nerve root sleeves (T1 images highlight fat content nerve roots and empty sleeves)
- Cord shift away from midline (T1 highlights fat of cord)
Localisation of brachial plexus:
- Roots seen in medial aspect of interscalene triangle
- Trunks seen in lateral aspect of interscalene triangle
- Divisions seen in Costoclavicular triangle
- Cords seen in infraclavicular region

TREATMENT OPTIONS:
- Till grade III injury , mostly conservative management is tried.
- For Grade IV injury with neuroma in continuity neurolysis and anterior epineurectomy is performed, excising the fibrous tissue.
- For grade V injury treatment options includes nerve grafts. The sural nerve, the sensory branch of ulnar nerve, and the medial cutaneous nerve of the forearm are the usual donor nerves. The outcome is influenced by the length of the nerve graft, the presence of scar tissue at the wound site, the number of grafts used, the presence of a healthy proximal stump available for grafting and the nerve gap to be covered.
- In preganglionic injury usually intercostal nerves are used as nerve grafts.
Conclusion
Brachial plexus injuries (BPIs) can involve any degree of injury at any level of the plexus and range from obstetric injuries to traumatic avulsions.
Diagnosis requires focused physical examination with EMG/NCS and MRI studies used for confirmation .
Treatment can be conservative versus operative depending on the chronicity of injury, degree of injury and nerve root involvement. For deciding the treatment options , the report should state whether there is pre or post ganglionic injury and in post ganglionic injury whether the nerve fibres are continuous or discontinuous.
REFERENCE:
- Yoshikawa T, Hayashi N, Yamamoto S et-al. Brachial Plexus Injury: Clinical Manifestations, Conventional Imaging Findings, and the Latest Imaging Techniques1. Radiographics. 2006;26 (suppl 1): S133-S143. Radiographics (full text)– doi:10.1148/rg.26si065511
- Castillo M. Imaging the anatomy of the brachial plexus: review and self-assessment module. AJR Am J Roentgenol. 2005;185 (6 Supplement): S196-204. AJR Am J Roentgenol (full text)– doi:10.2214/AJR.05.1014– Pubmed citation
- Nagano A, Ochiai N, Sugioka H et-al. Usefulness of myelography in brachial plexus injuries. J Hand Surg Br. 1989;14 (1): 59-64. Pubmed citation
- Baxter D. Tharin, Jonathan A. Kini, Gerald E. York, John L. Ritter. Brachial Plexopathy: A Review of Traumatic and Nontraumatic Causes. (2013) American Journal of Roentgenology. 202 (1): W67-75. doi:10.2214/AJR.12.9554– Pubmed
- Singer AD, Meals C, Kesner V, Boulis N, M Gonzalez F, Umpierrez M, Chhabra A. The Multidisciplinary Approach to the Diagnosis and Management of Nonobstetric Traumatic Brachial Plexus Injuries. (2018) AJR. American journal of roentgenology. doi:10.2214/AJR.18.19887– Pubmed
Dr. DEEPTI H.V
Consultant Radiologist
Manipal Hospitals Radiology Group
Dr. SHARNITHA JOHNSON
Fellow in Radiology
Manipal Hospitals Radiology Group