58 year old male presented with complaints of coughing and right sided chest pain for 1 month
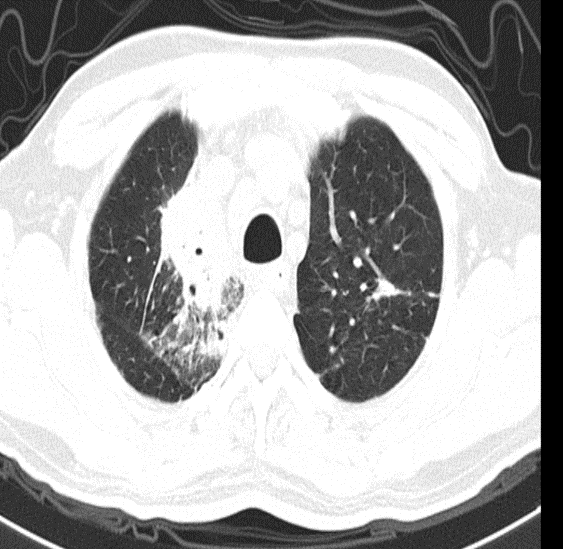
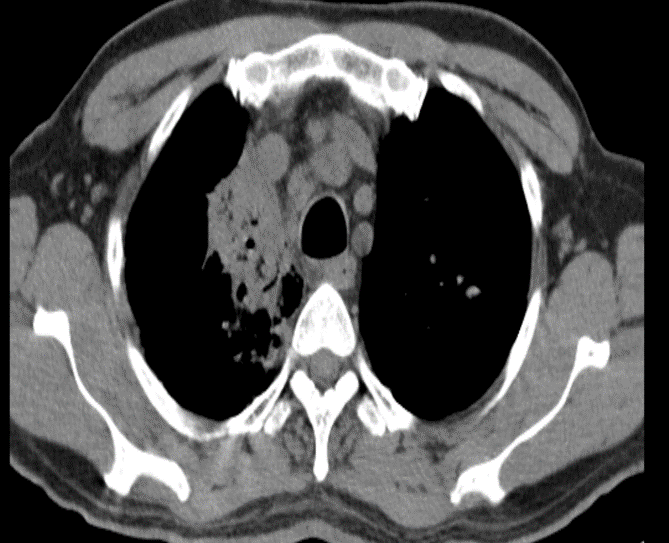
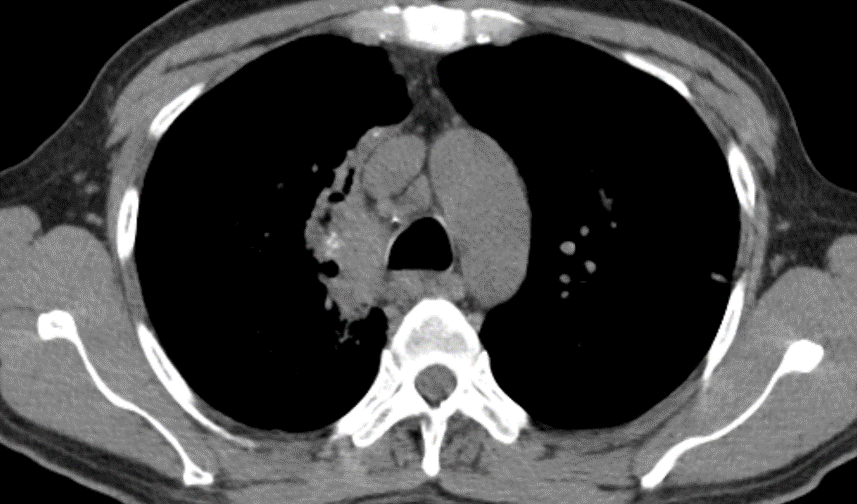
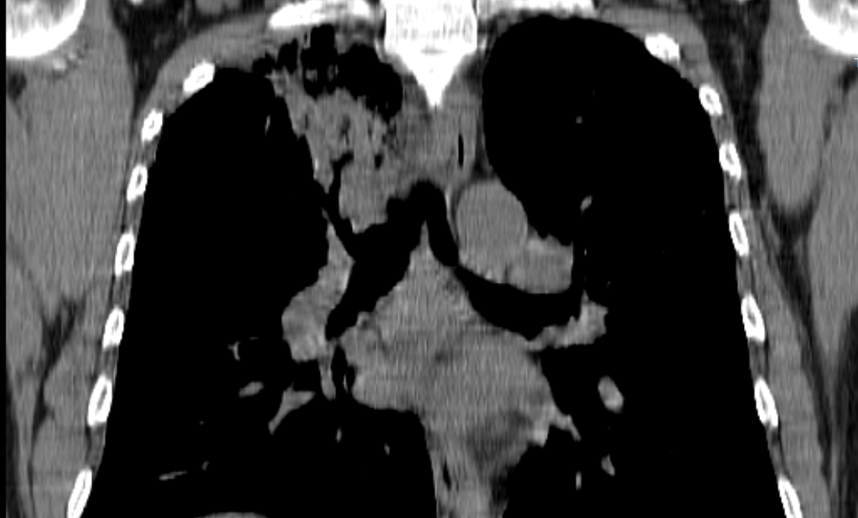
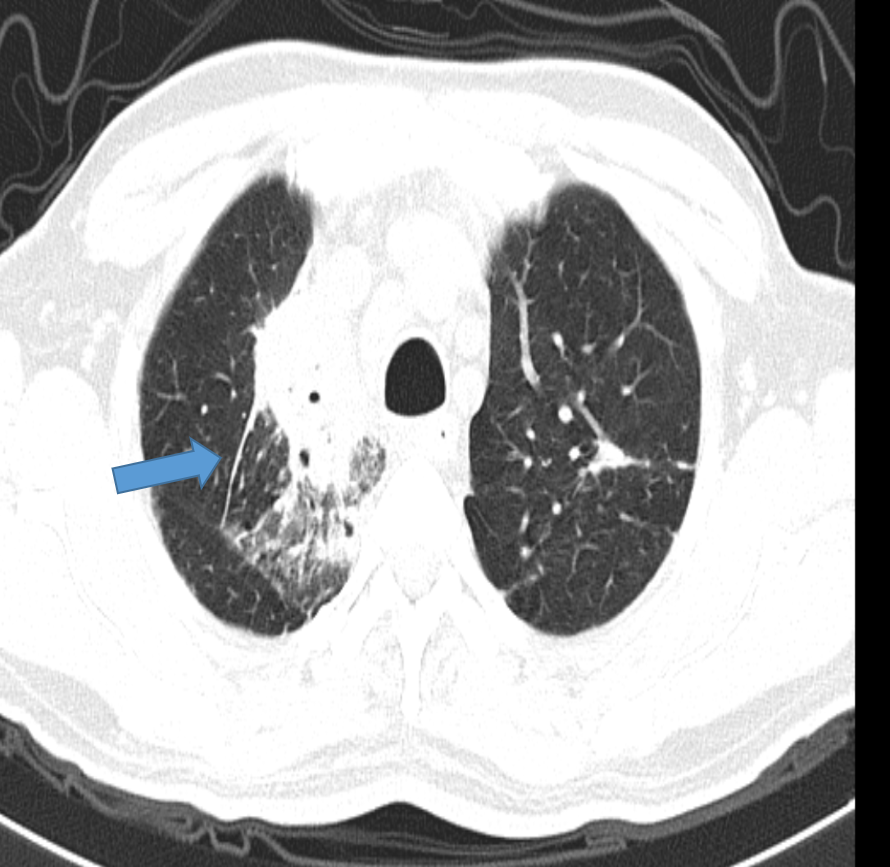
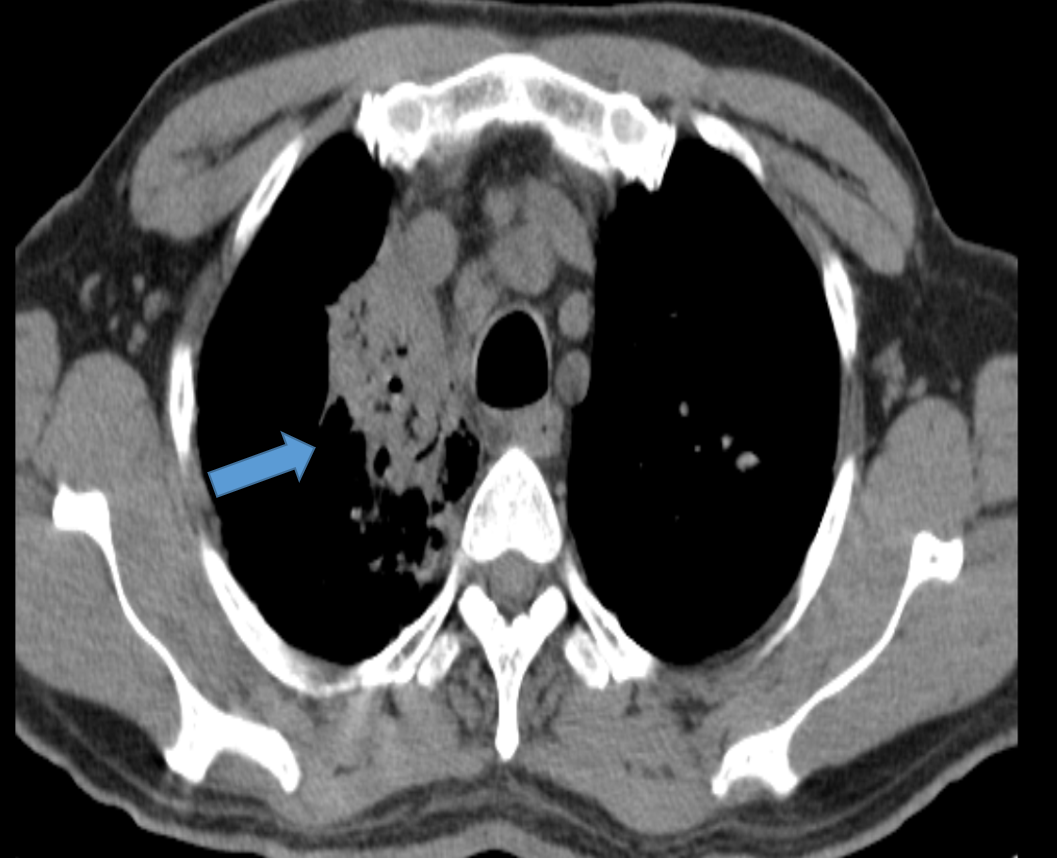
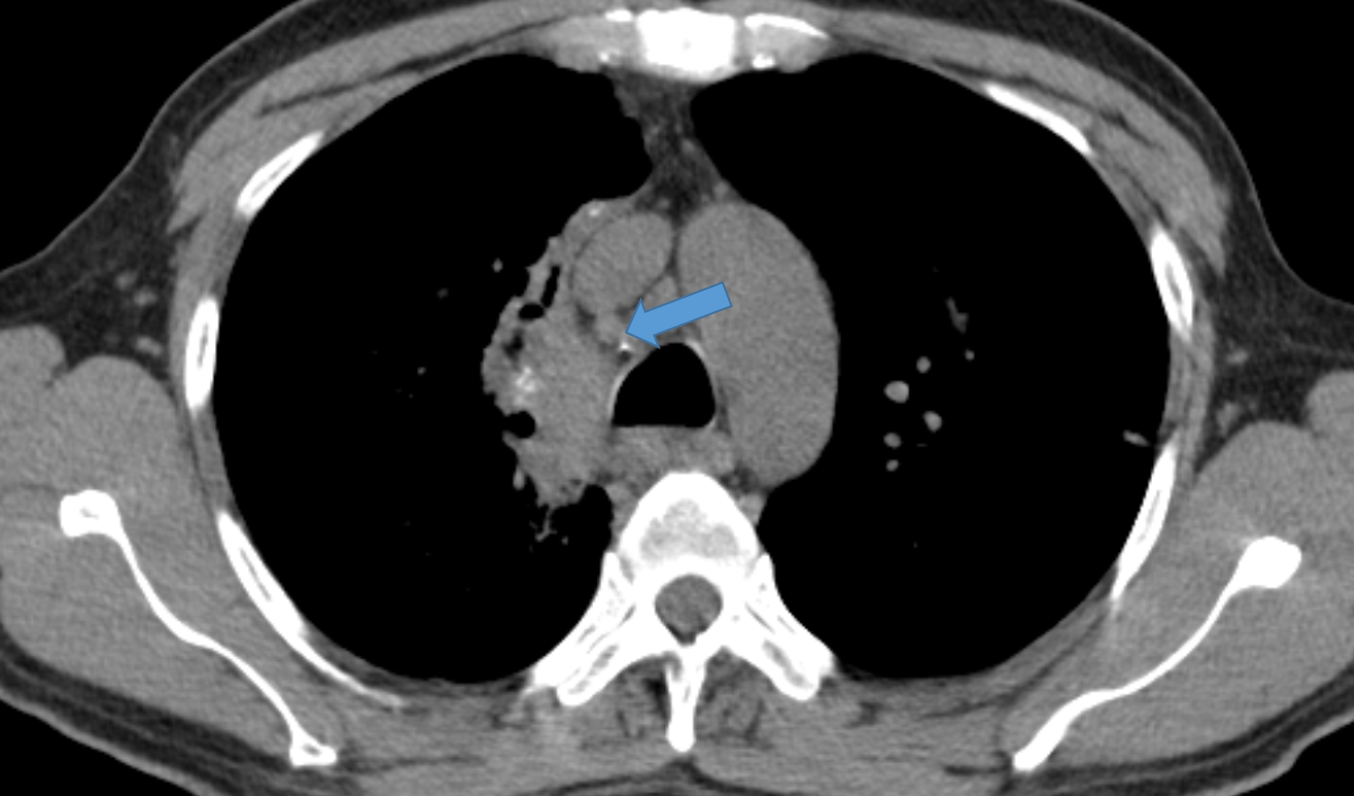
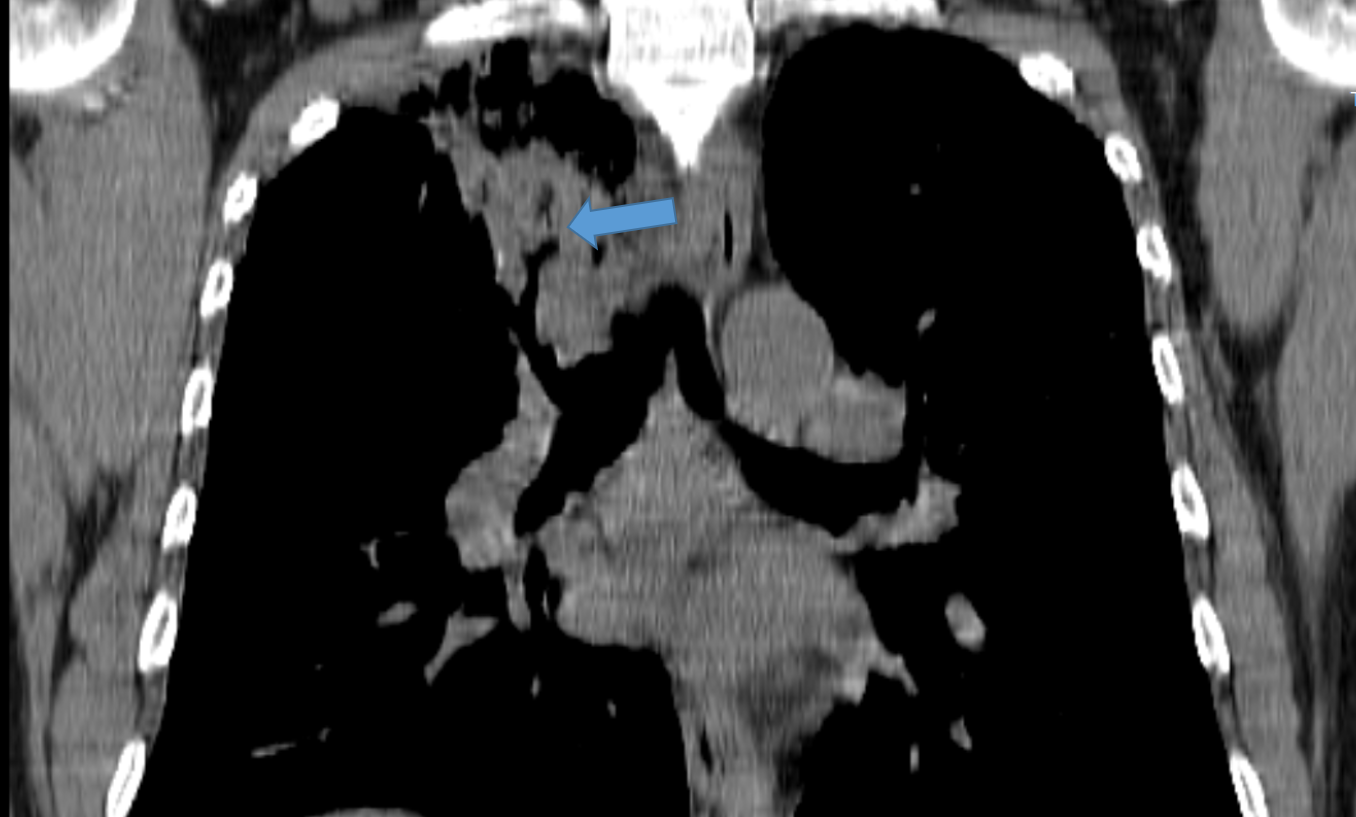
1. Axial CT images
Heterogeneous segmental consolidation is seen in the apical segment of the right upper lobe. Areas of breakdown cavitations are seen within the consolidation. Adjacent to the consolidation there is some amount of ground glassing with interlobular septal thickening.
2. There is likely invasion of the mediastinal pleura with bulging of the pleura towards the mediastinum
3. The consolidation shows subsegmental bronchiolar cut-off.
Bronchogenic carcinoma presenting as persistent long standing consolidation
DISCUSSION:
- Lung cancer is a leading type of cancer, equal in prevalence to breast cancer . It is the leading cause of cancer mortality worldwide; accounting for ~20% of all cancer deaths
- The major risk factor is cigarette smoking which is implicated in 90% of cases and increase the risk of lung cancer, which can be divided by histological subtype :squamous cell lung cancer: 11x (men), 15x (women)small cell lung cancer: 10x (men), 25x (women)large cell lung cancer: 7x (men), 8x (women)
lung adenocarcinoma: 4x (men and women)
L-PLADC (localized pneumonic-type lung adenocarcinoma ) is described as a special type of lung adenocarcinoma that presents as a focal consolidation involving < 50% of the area of a lobe . It is essential to differentiate clinical and imaging features between L-PLADC and localized pulmonary inflammatory lesion (L-PIL).
RADIOGRAPHIC FEATURES DIFFERNTIATING L-PLADC AND L-PIL
L-PLADC
Air bronchogram, irregular air bronchogram
Ground-glass opacity (GGO) component
and pleural retraction
L-PIL
Necrosis
Satellite lesions
Halo sign
Bronchial wall thickening, interlobular septa thickening, pleural attachment, and pleural thickening were more commonly seen in L-PIL
Differential diagnosis for chronic air space opacities
Cryptogenic organizing pneumonia
Granulomatosis with polyangiitis
Churg strauss pneumonia
Alveolar sarcoidosis
Post transplant lymphoproliferative disease
Lipoid pneumonia
Adenocarcinoma
Conclusion
In patients with chronic air space opacity , rule out underlying adenocarcinoma
Associated findings can help to narrow down the differentials
Biopsy to be considered in such cases
Reference :
- Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
- Pascoe HM, Knipe HC, Pascoe D, Heinze SB (2018) The many faces of lung adenocarcinoma: a pictorial essay. J Med Imaging Radiat Oncol 62:654–661
- Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL (1997) Bronchioloalveolar carcinoma: clinical, histopathologic, and radiologic findings. Radiographics 17:1345–1357
- Jung JI, Kim H, Park SH et al (2001) CT differentiation of pneumonic-type bronchioloalveolar cell carcinoma and infectious pneumonia. Br J Radiol 74:490–494
- Satoru N (2014) CT findings of pneumonic adenocarcinoma: comparison between invasive mucinous adenocarcinoma and nonmucinous adenocarcinoma. Global J 14:1–4
Dr. SHARNITHA JOHNSON
Fellow in Radiology
Manipal Hospital, Yeshwanthpur, Bengaluru.