58-year-old female presented to emergency department with complaints of 3 episodes of black coloured stools and tiredness
- 58 year old female presented to emergency department with complaints of 3 episodes of black coloured stools and tiredness.
- On examination, patient was hypotensive. Resuscitation was done and vitals were stabilized.
- Upper and lower GI scopy was done and were normal.
- Contrast CT of abdomen and pelvis with angiography was done.
FINDINGS
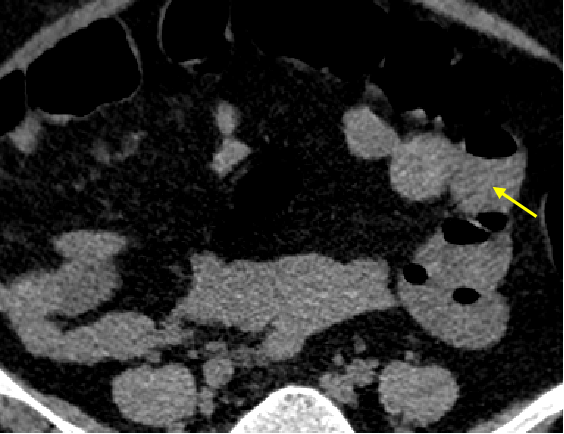
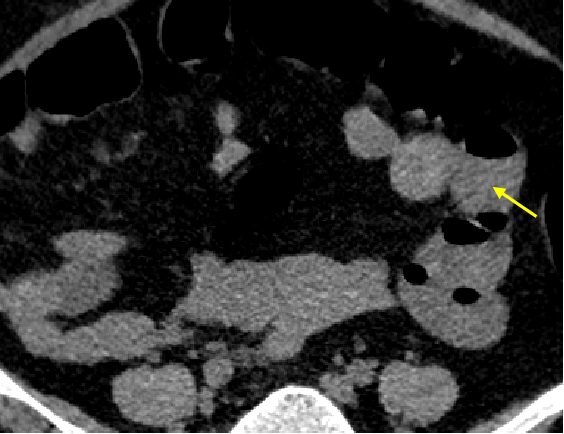
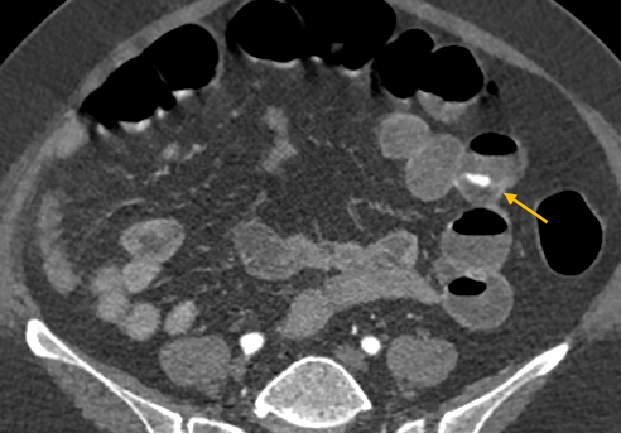
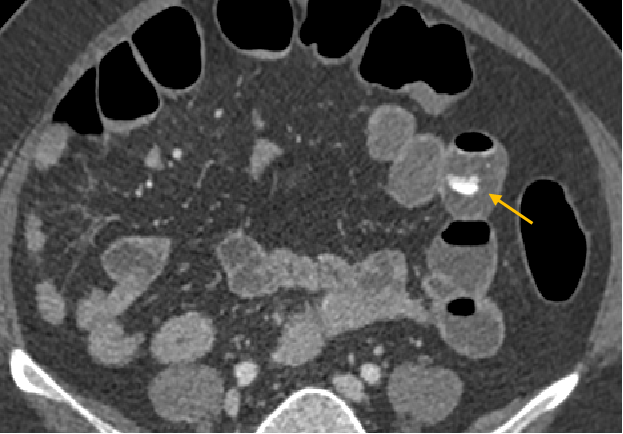
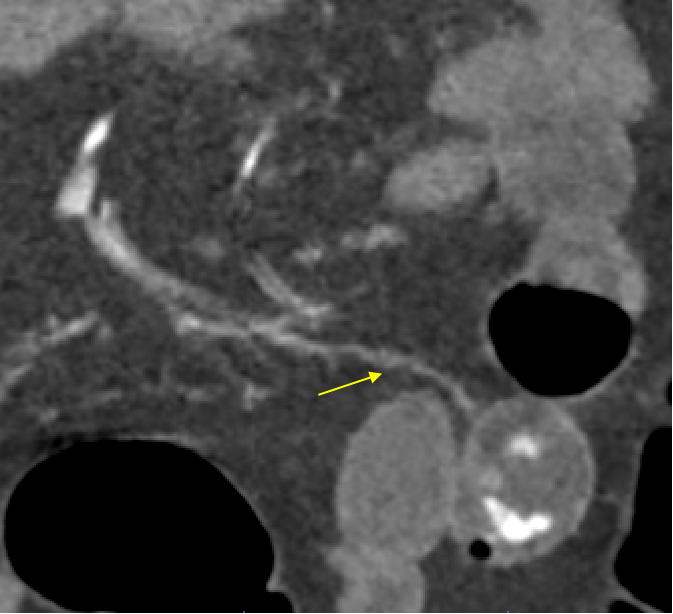
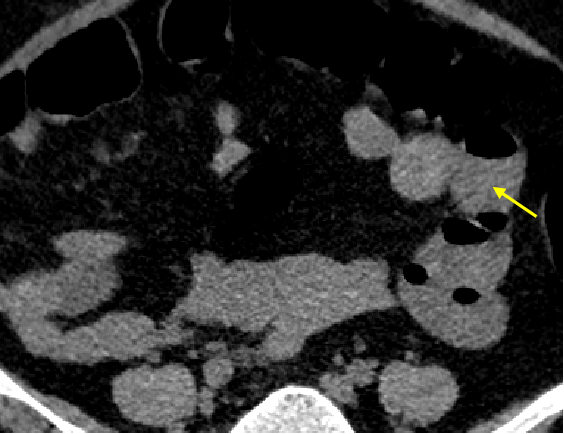
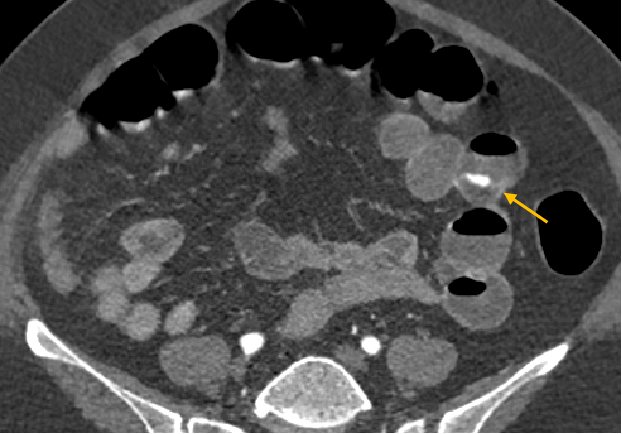
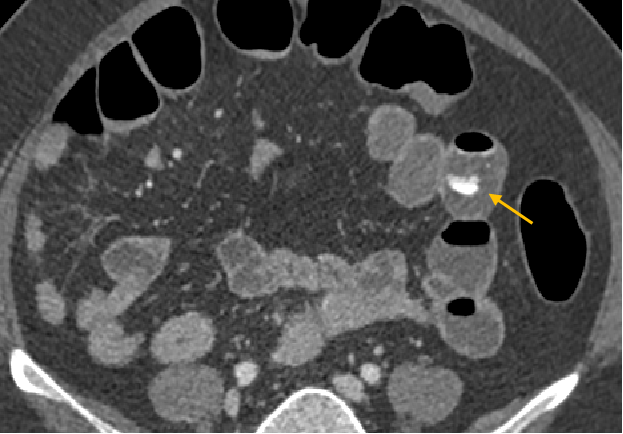
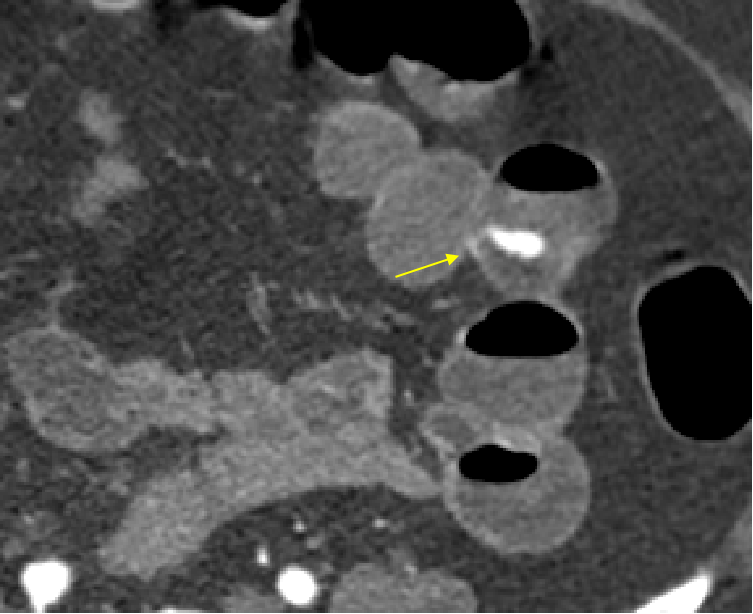
- Plain scans demonstrating blood in jejunal loops (FIG 1A). Post contrast angiography showing active contrast extravasation in arterial phase in distal jejunal bowel loop (FIG 1B) with increase in bleed on venous phase of study (FIG 1C) consistent with active bleeding.
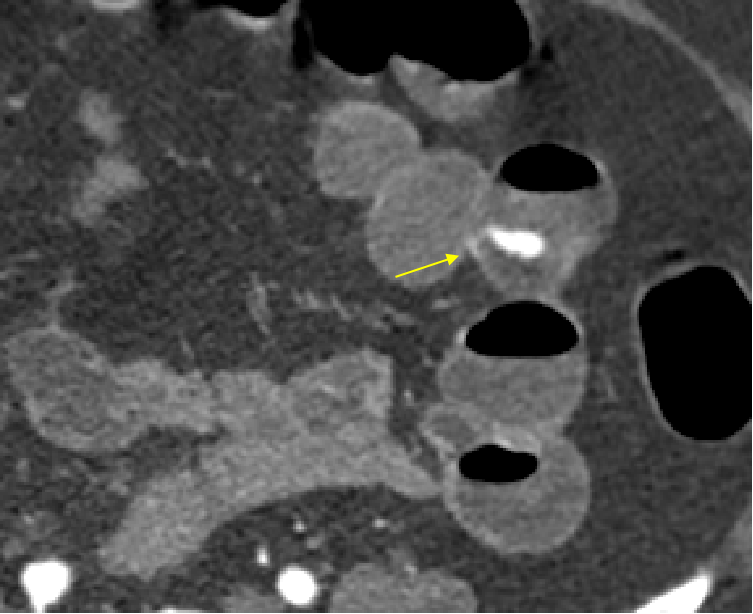
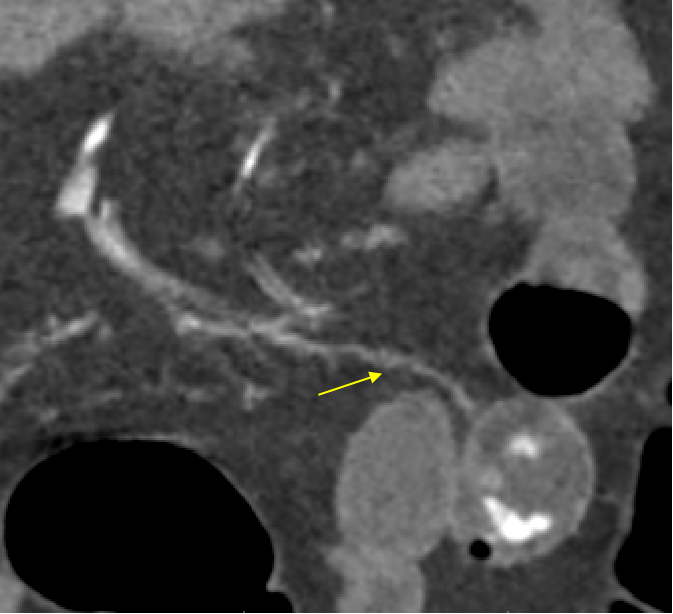
- Coronal reformatted image showing active contrast blush being supplied by distal jejunal branch of superior mesenteric artery (FIG 2A and 2B).
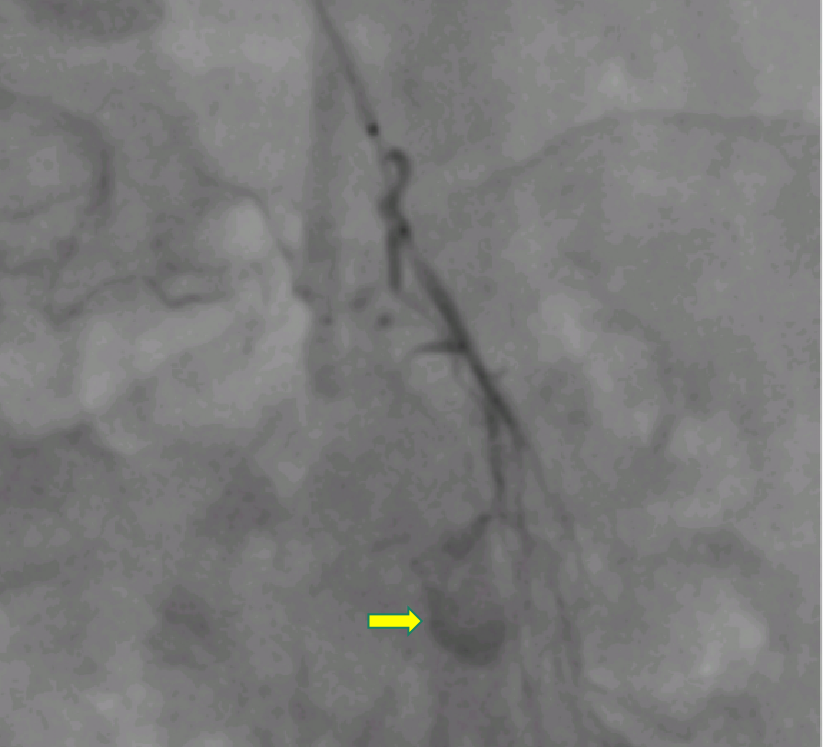
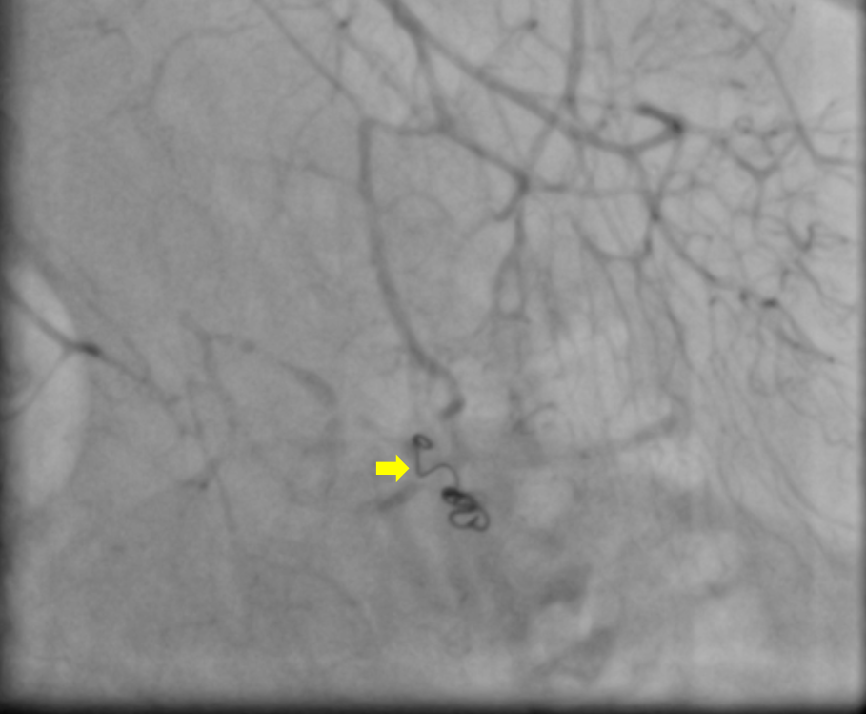
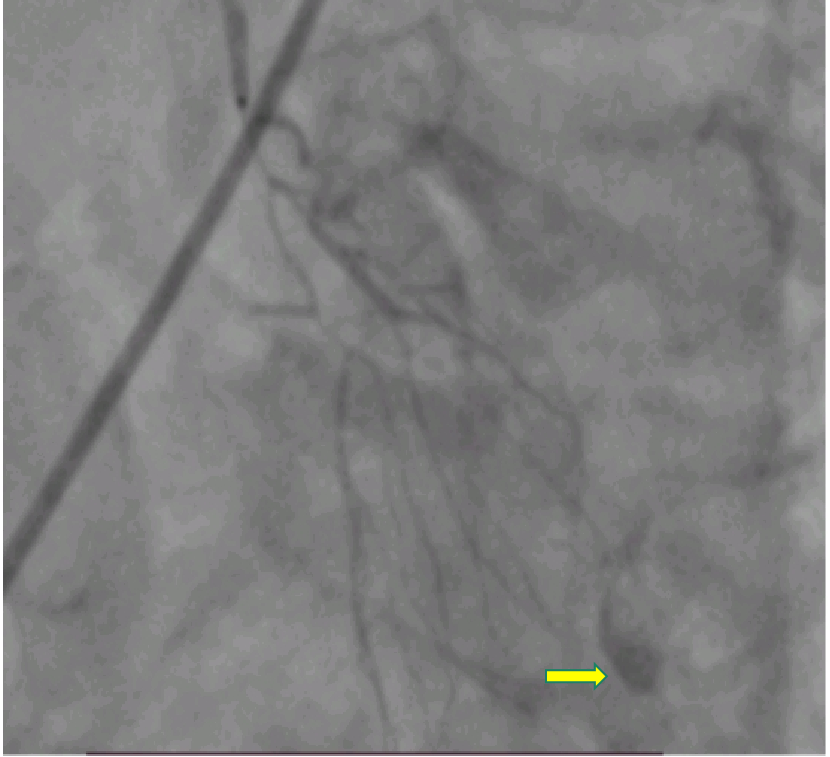
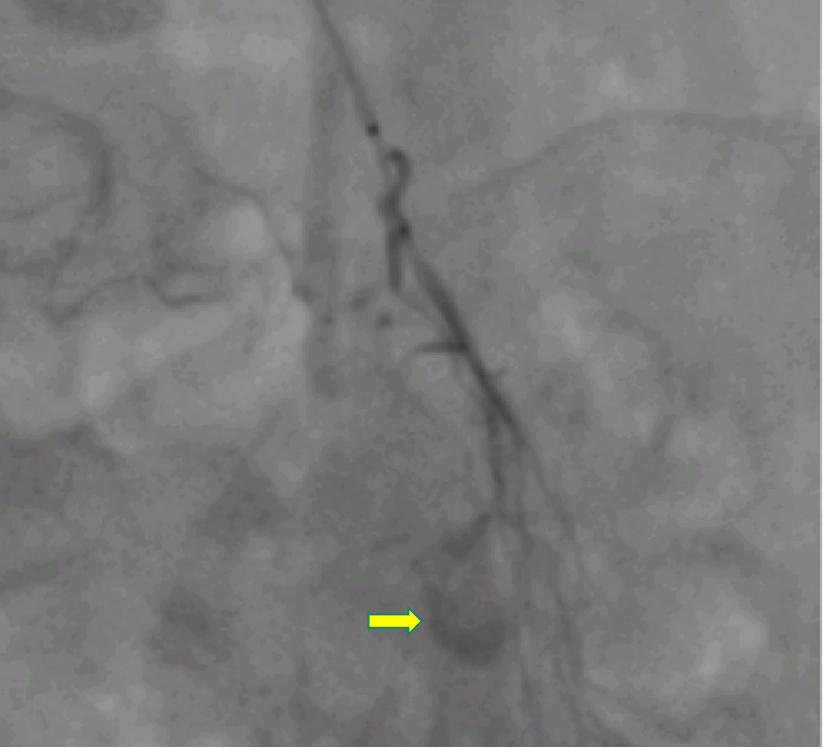
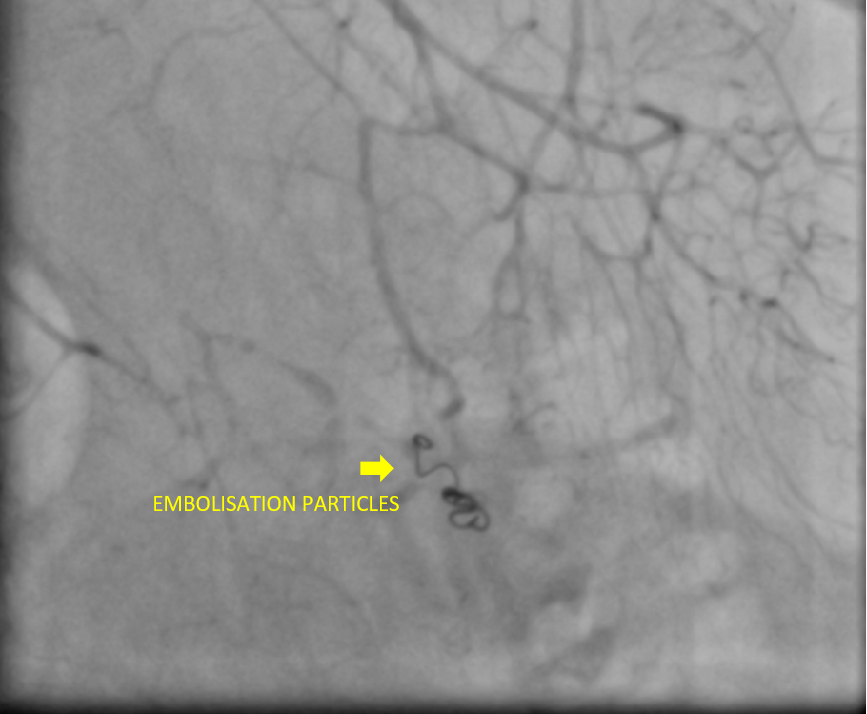
- Based on CT angiography findings; patient was taken up for DSA and embolization of distal jejunal branch. Digital substraction angiography demonstrates active contrast blush in one of the distal jejunal branch (FIG 3A and 3B).
- Post embolization images showing no active blush.
Diagnosis:
Active small bowel bleeding
Lower gastrointestinal bleeding (LGIB) is defined as that occurring distal to the ligament of Treitz (i.e. from the jejunum, ileum, colon, rectum or anus) and presenting as either haematochezia (bright red blood/clots or burgundy stools) or melaena.
Small bowel causes of GI bleeding:
- Most common cause of obscure gastrointestinal bleeding.

How does radiology help ?
- Clinical differentiation of GI bleed as UGI versus LGI is the first step in diagnostic workup.
- Imaging plays a key role with both overt and occult GI bleeding that are hemodynamically stable.
CT ANGIOGRAPHY
- CTA can detect flow rates as low as 0.3 mL/min and has a sensitivity of 50%-86% and specificity of 92%-95% for identifying lesions responsible for GI bleed.
- In addition to identifying the site of bleeding; CTA can often identify the etiology of GI bleed which may be useful for further management.
- Typical protocol for CTA consists of noncontrast (unenhanced), arterial phase, and portal venous phase with intravenous contrast at 4-5 mL/s.
TRANS CATHETER ARTERIAL EMBOLIZATION
- Transcatheter arterial embolization (TAE) is effective for controlling acute GI bleed.
- The goal of TAE is super-selective embolization of bleeding vessels to reduce arterial perfusion pressure while maintaining adequate collateral blood flow to minimize the risk of bowel infarction.
- The type of embolic agent used is conventionally dependent on the interventional radiologist’s experience and preference, etiology of bleeding, and availability of the agent.
REFERENCE:
- Carney BW, Khatri G, Shenoy-Bhangle AS. The role of imaging in gastrointestinal bleed. Cardiovasc Diagn Ther. 2019 Aug;9(Suppl 1):S88-S96. doi: 10.21037/cdt.2018.12.07. PMID: 31559156; PMCID: PMC6732104.
- Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015 Sep;110(9):1265-87; quiz 1288. doi: 10.1038/ajg.2015.246. Epub 2015 Aug 25. PMID: 26303132.
Dr. Vishwanath Joshi
Consultant Radiologist
Manipal hospital -Varthur, Bengaluru.
Dr. Ronisha
Radiology resident.
Manipal hospital -Varthur, Bengaluru.