54 years old gentleman, known diabetic and hypertensive with history of left nephrectomy (post traumatic) and chronic kidney disease on ESRD.
- 54 years old gentleman, known diabetic and hypertensive with history of left nephrectomy (post traumatic) and chronic kidney disease on ESRD.Presented with AKI and urosepsis. CECT was performed.
- Patient again presented 4 months later with anuria and severe abdominal pain, underwent CECT again.
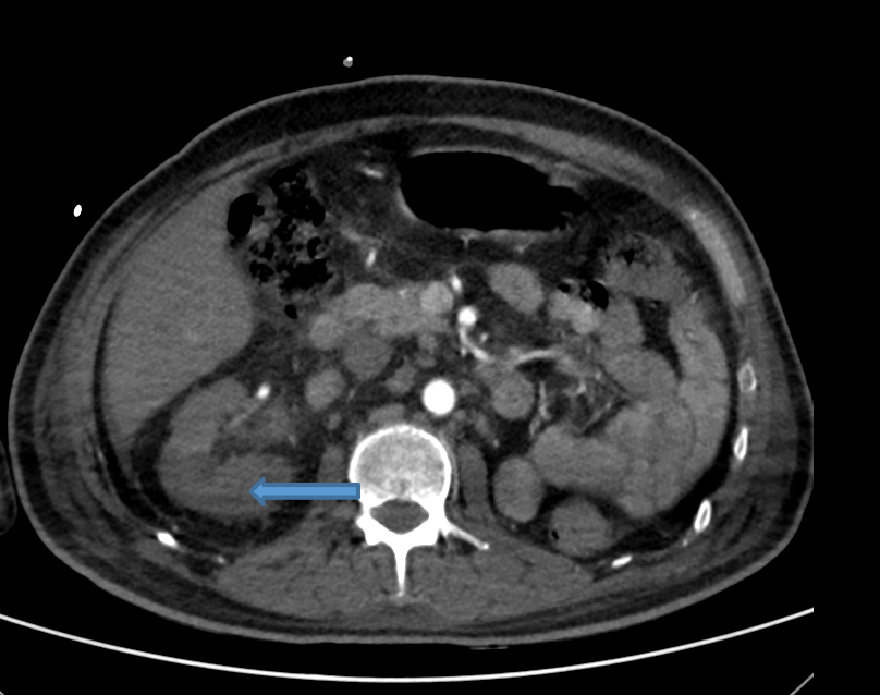
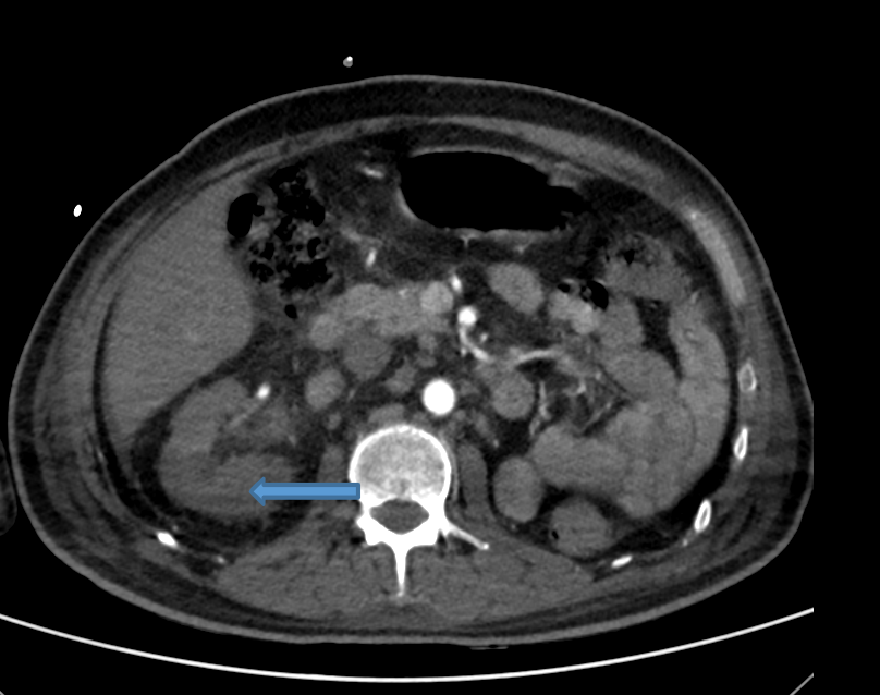
- Axial arterial phase image depicting global hypo enhancement of right kidney (arrow) with surrounding fat stranding – right renal infarct. Non visualization of left kidney –post nephrectomy status.
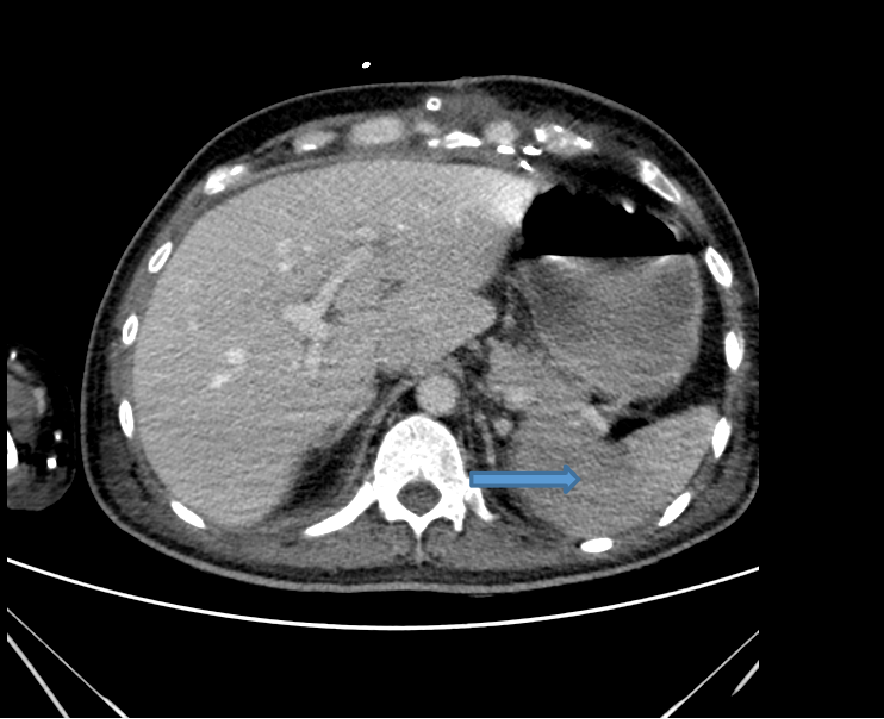
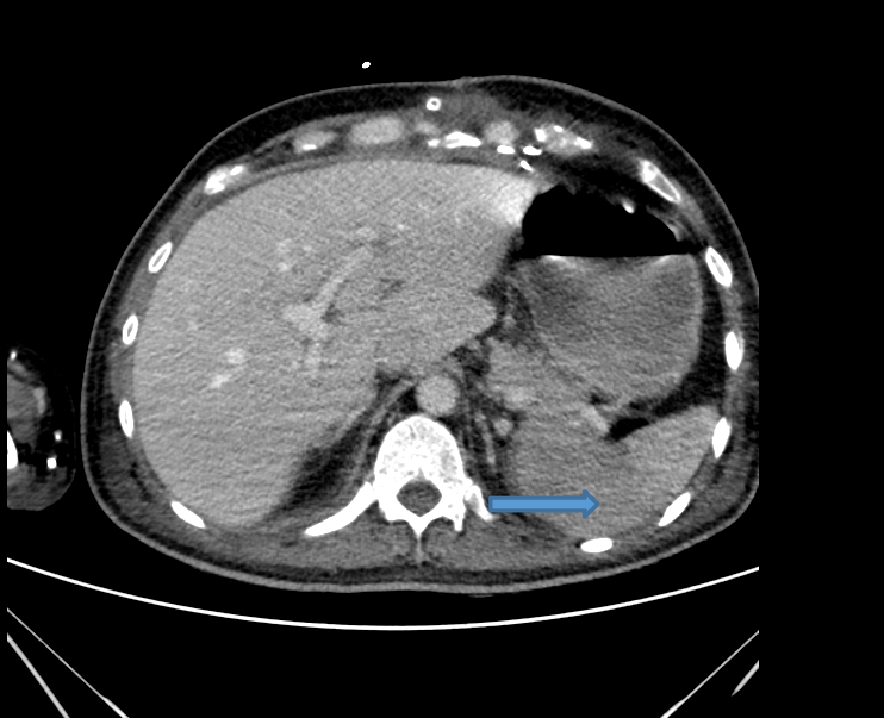
- Axial venous phase image showing wedge shaped area of hypo enhancement of splenic parenchyma (arrow)suggestive of infarction.
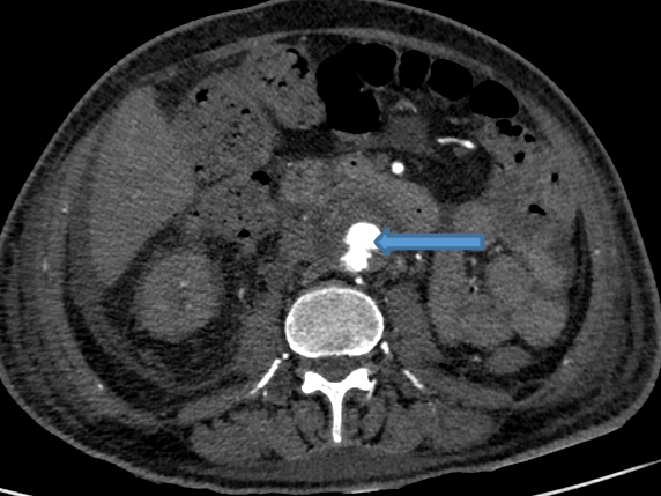
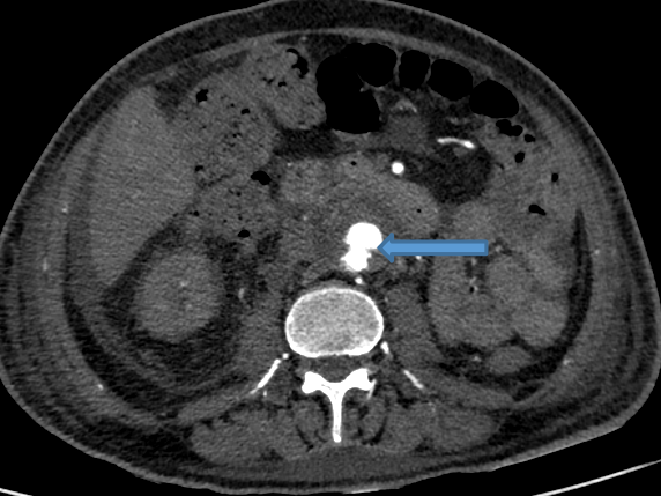
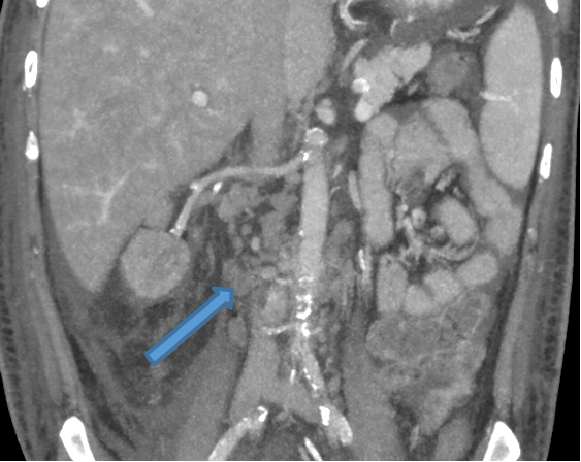
- Saccular aneurysm with irregular lobulated outline arising from infra-renal abdominal aorta, surrounded by thick rim of hypodensity.
- Multiple enlarged retroperitoneal nodes.
- Multiple enlarged retroperitoneal nodes.
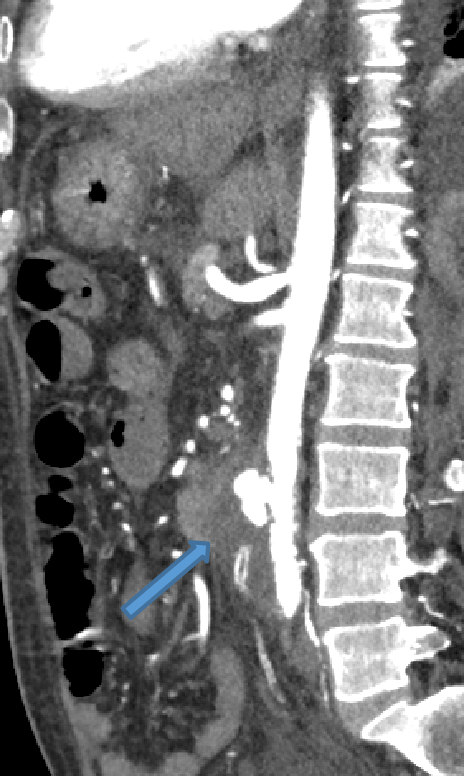
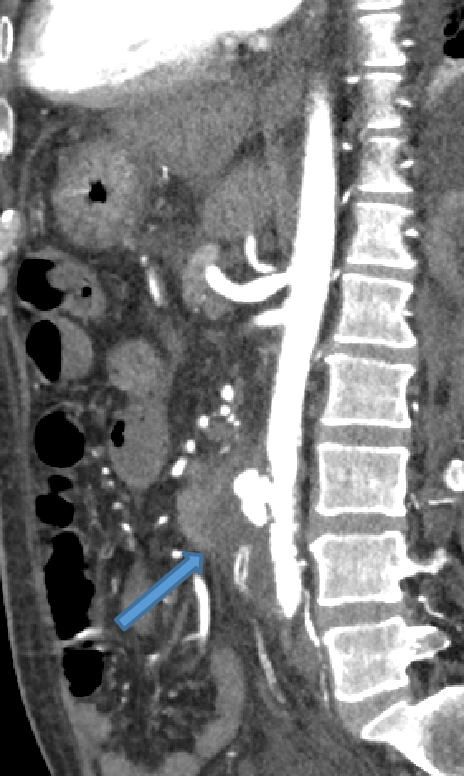
- Coronal NCCT image depicting EVAR graft within the infrarenal abdominal aorta.
DIAGNOSIS
- MYCOTIC ANEURYSM OF INFRARENAL ABDOMINAL AORTA
DISCUSSION
- Infected aneurysm (or mycotic aneurysm) is defined as an infectious break in the wall of an artery with formation of a blind, saccular outpouching that is contiguous with the arterial lumen.
- It consists of compressed perivascular tissue, hematoma, and fibroinflammatory tissue. The infected aneurysm can subsequently undergo free rupture due to sustained systemic arterial pressure.
- Aorta, peripheral arteries, cerebral arteries, and visceral arteries are involved in descending order of frequency.
- Causes: (a) hematogenous spread of infectious micro emboli into the vasa vasorum, (b) infection of a preexisting intimal defect by circulating infectious agent, (c) contiguous involvement of the vessel from an adjacent source of sepsis, (d) direct infectious inoculation of the vessel wall at the time of vascular trauma.
- Thoracic aortic aneurysms usually manifest as chest and interscapular pain, whereas infected abdominal aortic aneurysms usually manifest as abdominal pain with or without a pulsatile mass.
- Non treatment or delayed treatment of infected aneurysms often leads to fulminant sepsis, spontaneous arterial rupture, and death.
- Imaging allow detection of infected aneurysms in clinically suspicious cases and characterization of infected aneurysms, as well as vascular mapping to facilitate treatment planning in confirmed cases.
- Multidetector CT angiography is the current imaging modality of choice for the evaluation of suspected infected aneurysms. Cardiac gating can be used to evaluate thoracic aortic aneurysms.
- MRI – 3Dcontrast-enhanced MR angiography, faster gradient technology, use of advanced techniques (such as steady-state free precession, optimized k-space filling strategies, parallel imaging techniques, and time-resolved imaging have increased the utility.
- Sonography in diagnosis of infected aneurysms is limited to the peripheral arteries.
- Nuclear scintigraphy, such as gallium scanning and indium-labeled leukocyte scanning, for routine evaluation of infected aneurysms is limited.
AORTA
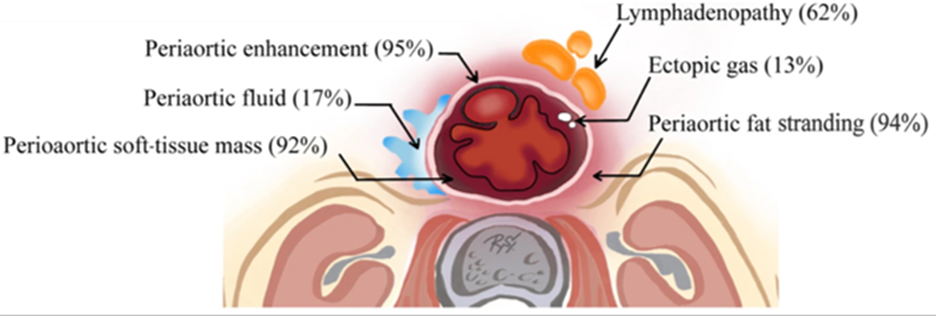
- Early changes of aortitis - irregular arterial wall, periaortic fat stranding, periaortic soft-tissue mass, and periaortic gas.
- Aneurysm - focal, contrast-enhancing dilatation that is usually saccular. The lumen can be central or eccentric and can be a single or multiloculated. Disrupted arterial wall calcification can occur adjacent to the infected aneurysm. Calcification and thrombus within an infected aneurysm are uncommon.
- Ruptured aneurysms show active contrast extravasation and adjacent hematoma.
TREATMENT
- The specific management of an infected aneurysm must be individualized and is dependent on the characteristics of the aneurysm, patient characteristics.
- In general, small, asymptomatic, and unruptured infected aneurysms can be managed with a trial of intravenous antibiotics for 4–6 weeks along with surveillance imaging.
- Enlarging or residual aneurysms at surveillance imaging are triaged to surgical management.
- Surgical techniques include endovascular aneurysm repair, endovascular embolotherapy.
REFERENCES
- Lee WK, Mossop PJ, Little AF, Fitt GJ, Vrazas JI, Hoang JK, Hennessy OF. Infected (mycotic) aneurysms: spectrum of imaging appearances and management. Radiographics. 2008 Nov;28(7):1853-68.
- Dean RH, Waterhouse GE, Meacham PW, Weaver FA, O'Neil Jr JA. Mycotic embolism and embolomycotic aneurysms. Neglected lessons of the past. Annals of surgery. 1986 Sep;204(3):300.
- Aoki C, Fukuda W, Kondo N, Minakawa M, Taniguchi S, Daitoku K, Fukuda I. Surgical management of mycotic aortic aneurysms. Annals of vascular diseases. 2017 Mar 24;10(1):29-35.
Dr RAJESH HELAVAR
Senior Consultant Interventional Radiologist MHRG
Dr VIKHYATH SHETTY
Consultant Radiologist MHRG
Dr ANAGH VISHNU NARAYANAN
Radiology resident Manipal Hospital, Yeshwanthpur, Bengaluru.