52 year old male presented with long standing intermittent and recurrent GI issues
52 year old male presented with long standing intermittent and recurrent GI issues
- Post prandial distress ,bloating , followed by abdominal pain and vomiting.
- Altered bowels with loose stools.
- No Weight loss /No dysphagia.
FINDINGS:
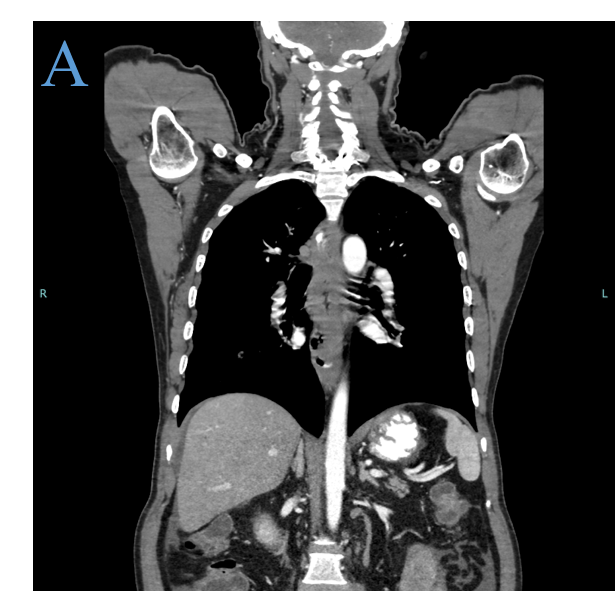
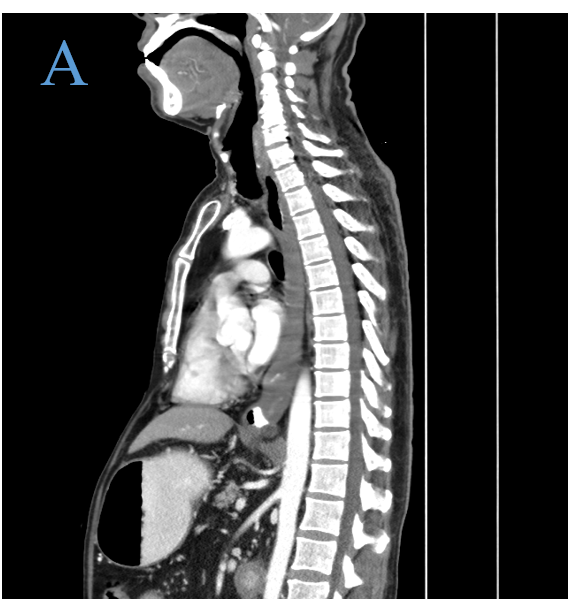
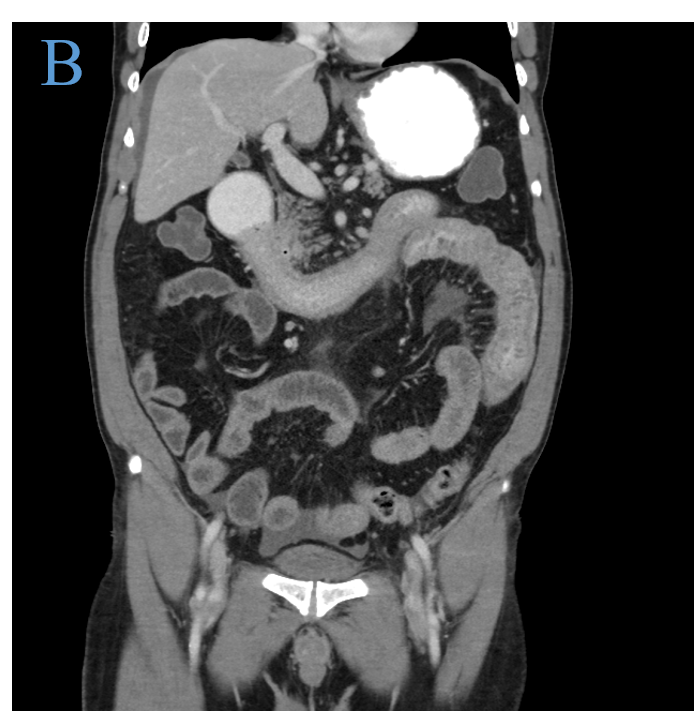
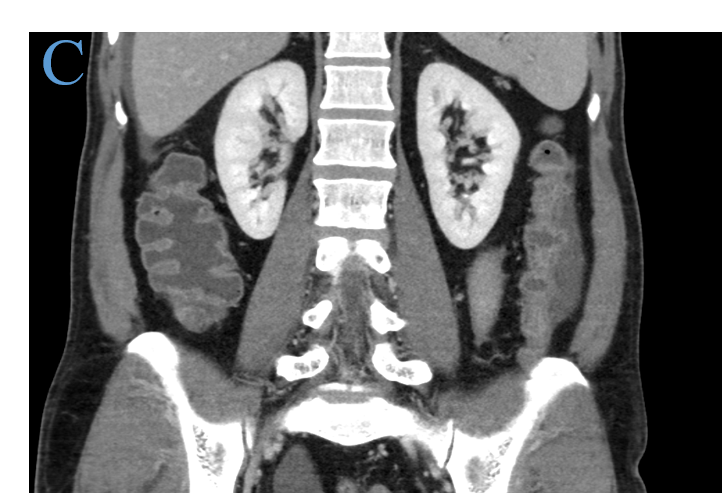
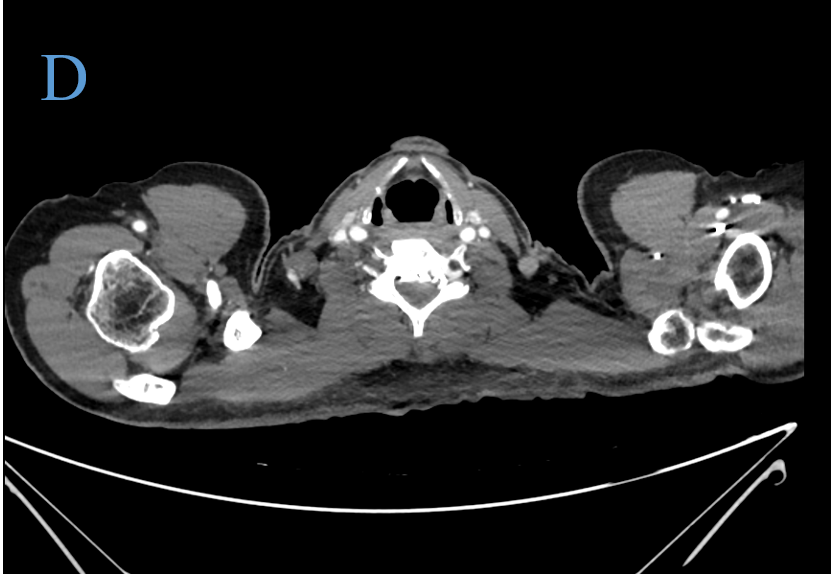
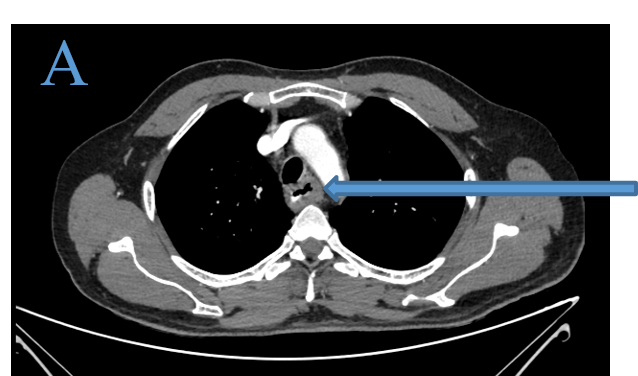
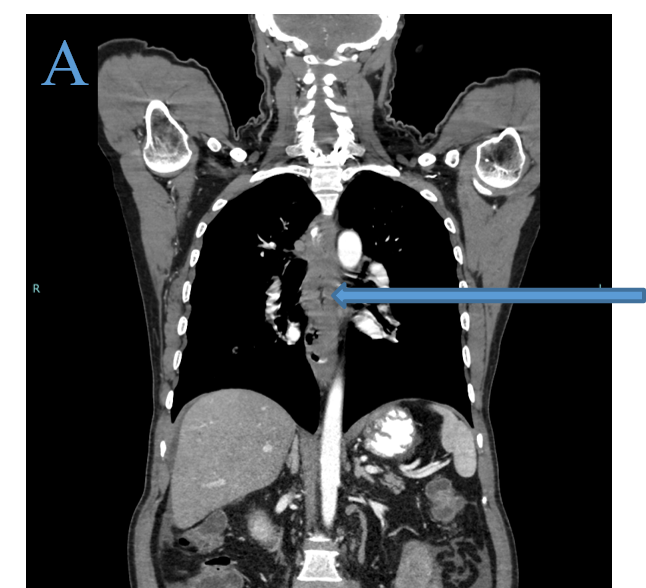
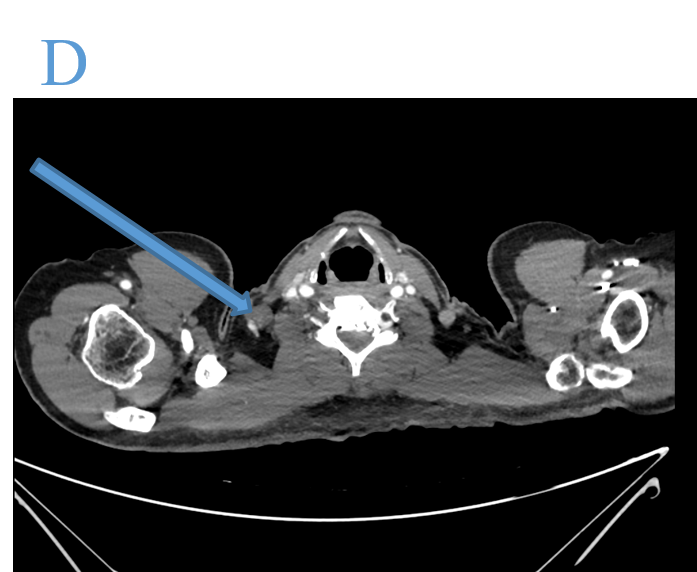
- CECT CHEST, ABDOMEN AND PELVIS
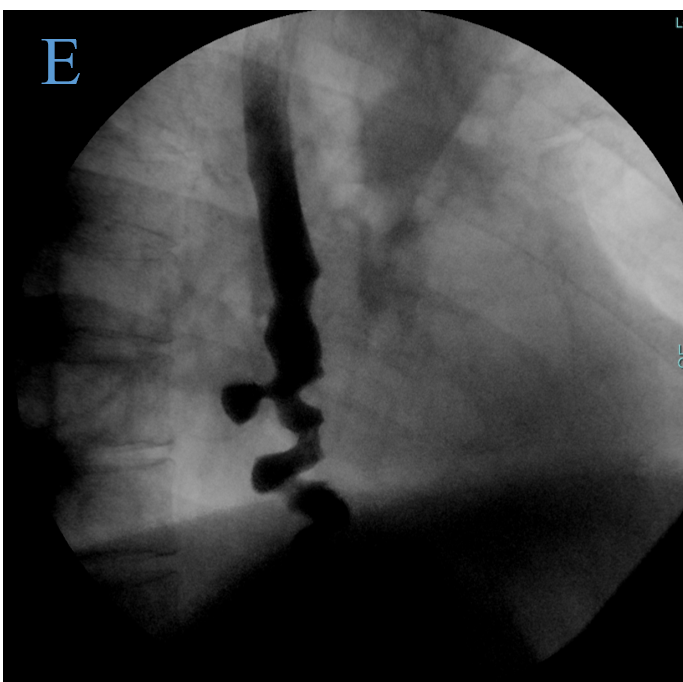
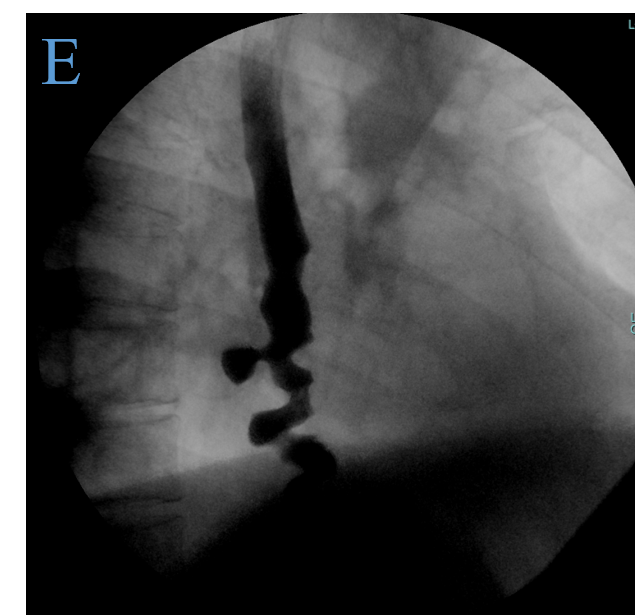
- BARIUM SWALLOW
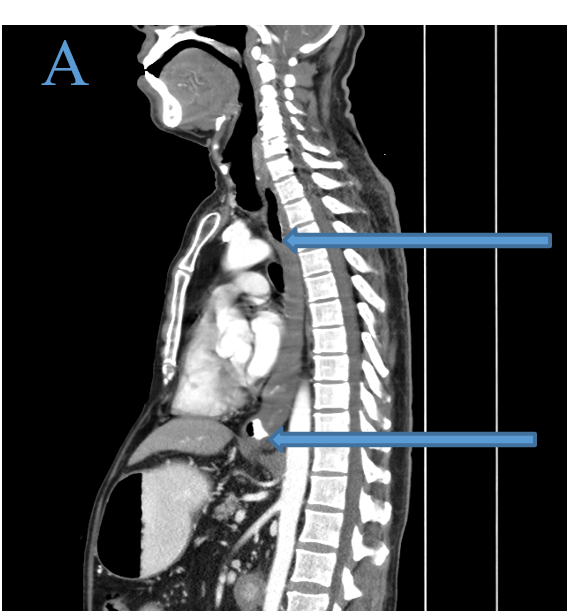
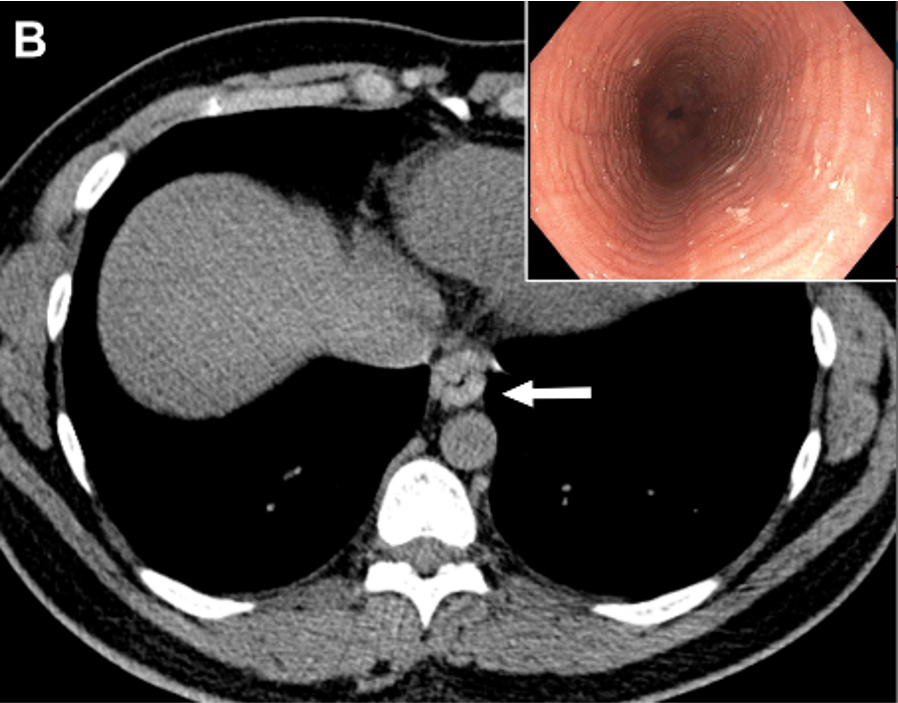
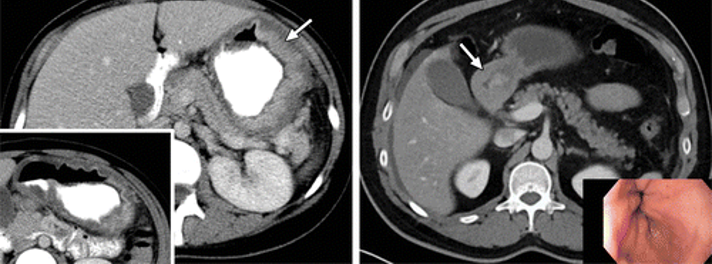
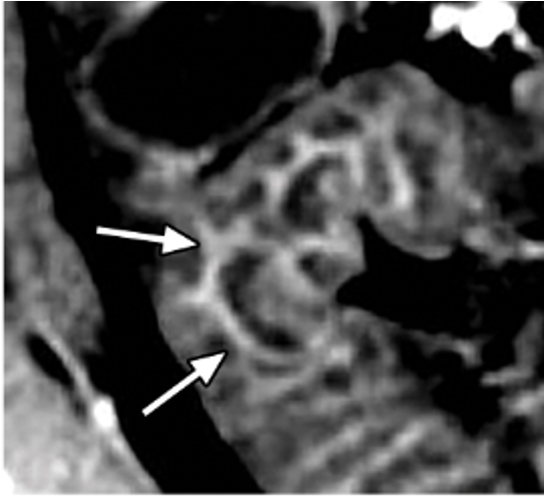
- Asymmetric, homogenously enhancing, circumferential long segment wall thickening of the
upper, middle and lower esophagus resulting in significant luminal narrowing. - It begins at T3 ( just distal to sternal notch level) and extends to GE junction.
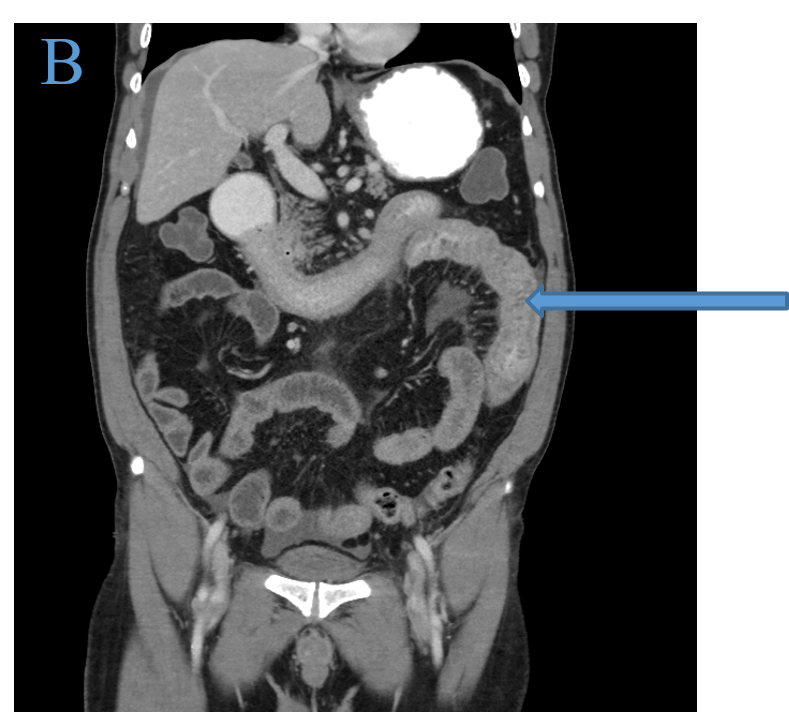
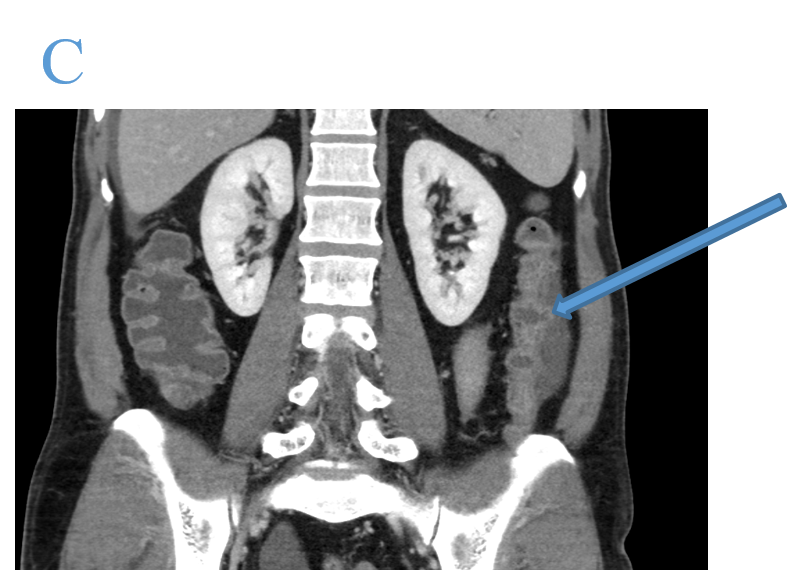
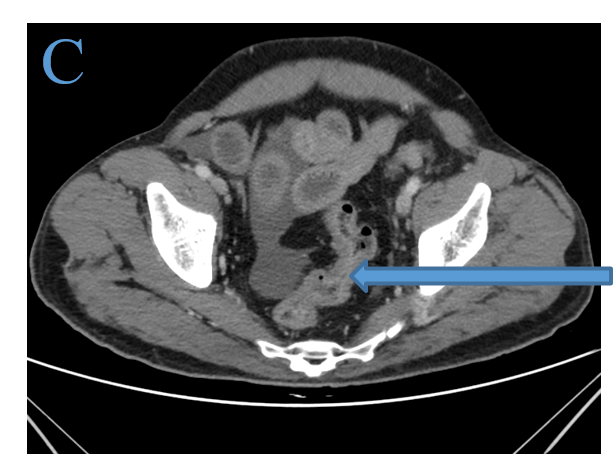
- Diffuse, edematous and smooth mucosal thickening of all the proximal small bowel loops with moderate surrounding peri-enteric fat stranding and non-marginated fluid.
- Diffuse, edematous and smooth mucosal thickening of the descending and sigmoid colon.
- An enlarged and non-necrotic right posterior triangle (level V).
- Corkscrew esophagus seen in distal esophagus with 1 cm sized diverticulum- diffuse esophageal spasm.
- The upstream esophagus is mildly dilated.
DIAGNOSIS:
- Eosinophilic esophagitis and gastroenteritis.
DISCUSSION:
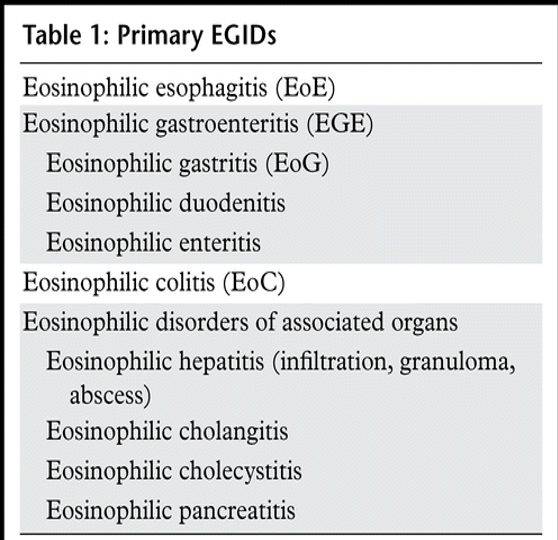
- Eosinophilic GI Disorders
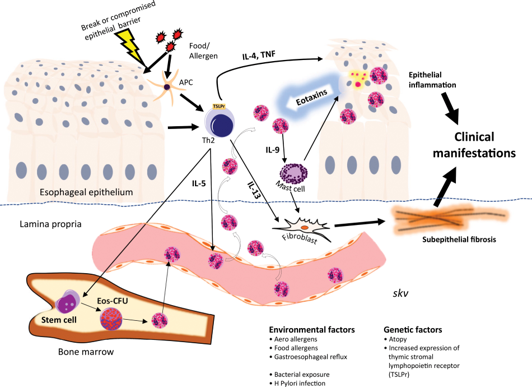
EGIDs can be primary or secondary EGIDs
Primary EGIDs-
- Primarily affect the GI tract, with eosinophil-rich inflammation in absence of known causes of eosinophilia such
as parasitic infections, malignancy, and drug reactions. - These EGIDs are associated with atopy and allergies and can be localized to one or more organs in the GI tract.
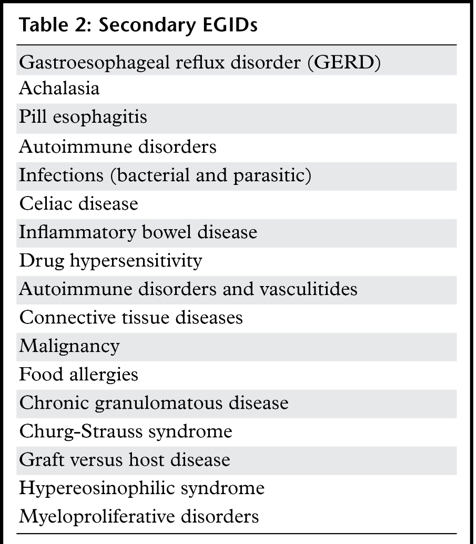
Secondary EGIDs-
- Eosinophilic infiltration of the GI tract occurs in association with a separate known cause or identifiable
systemic disease. - The clinical symptoms of EGIDs are variable - a diagnostic evaluation is recommended for patients with refractory
GI symptoms, especially those with a history of allergy-related diseases or a family history of EGIDs.
Eosinophilic esophagitis
- Most common EGID.
- Result of a complex interaction between immunogenic factors and environmental exposure in predisposed
individuals with atopy.
- Imaging modality of choice for EoE diagnosis and follow-up is Esophagography.
- It allows real-time measurement of the esophageal diameter for stricture assessment and interventional planning.
- The predominant pattern of EoE seen at esophagography is that of fixed luminal narrowing, which may be
smooth and tapered or associated with characteristic ring like indentations.
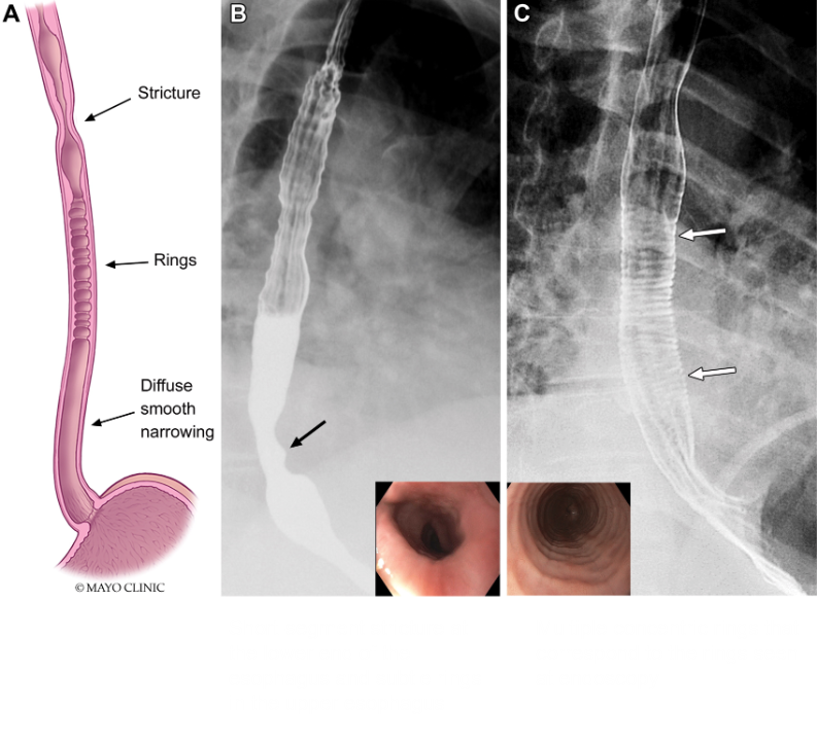
- Esophageal wall thickening secondary to EoE can be visualized with CT and MRI.
- Rarely performed for the evaluation of EOE.
Eosinophilic Gastroenteritis
- Eosinophilic infiltration of the stomach and small intestine.
- A single bowel segment or multiple organs in various combinations also may be involved concurrently.
- Three subtypes of EGE have been defined on the basis of the predominant gut layer involved by eosinophilic
infiltration: mucosal, muscular, and serosal.
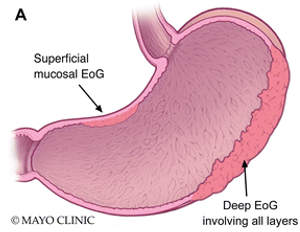
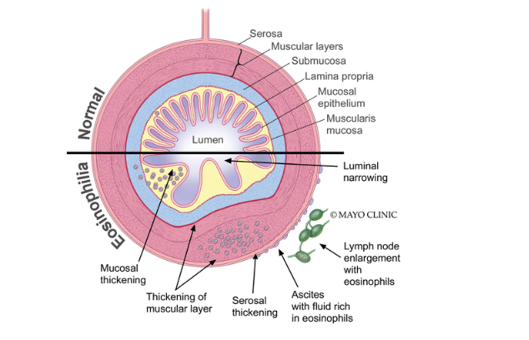
- The radiologic findings of EGE depend on the predominant gut layer involved.
- Mucosal EGE - Mucosal thickening is the most prominent finding.
- Muscular EGE- Bowel wall narrowing and dysmotility or obstruction.
- Serosal EGE -Ascites is most common feature and may be accompanied by thickened omentum and mesentery.
Diffuse thickening and hyperenhancment of the gastric mucosa Thickening of the antrum
- Although the imaging appearances of eosinophilic duodenitis and eosinophilic enteritis are nonspecific.
- Two radiologic signs help to distinguish it from malignant process: the “halo” sign and the araneid limb like sign.
- Neither of these signs is specific for eosinophilic enteritis, and both can be seen with several inflammatory and
infective disorders.
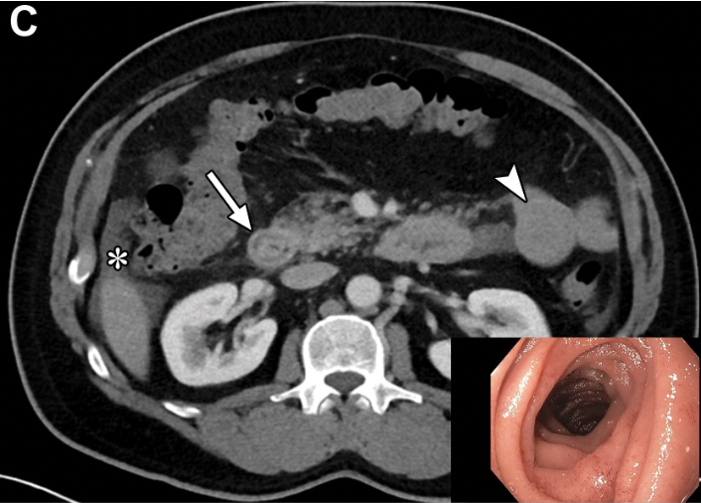
Halo sign refers to the layered gut wall appearance secondary to submucosal edema on contrast-enhanced cross-sectional images
The araneid limb like sign is produced when orally administered positive contrast material coats the thickened mucosal folds and sinks into the sinuses between the folds, resembling the appearance of spider legs
- The diagnosis of EGID is based on clinical suspicion, supportive imaging findings, and histologic
confirmation of eosinophil-rich inflammation in the tissue or organ. - Diet modification and use of oral corticosteroids are the major therapeutic approaches.
References
Dr. MADHU KUMAR SB
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. SHIKHA JOSHI
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.