50-year-old gentleman with pain in upper abdomen
- 50-year-old gentleman with pain in upper abdomen since a year
- There was no history of vomiting, gastrointestinal bleed, jaundice, anorexia and weight loss
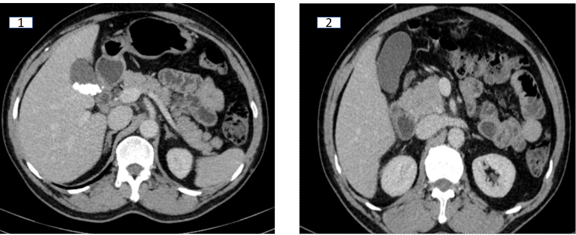
The head, neck, and body of the pancreas appear normal in morphology. The pancreatic duct is not dilated (Image 1 and 2 ).
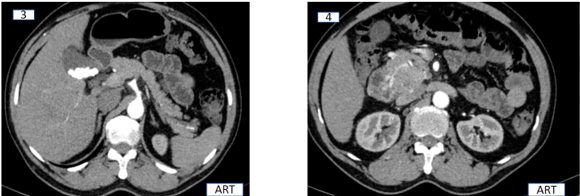
A solid enhancing mass lesion appears to be arising in continuity with/ flush with the uncinate process. It is supplied by the gastroduodenal artery (Image 3 ,4).
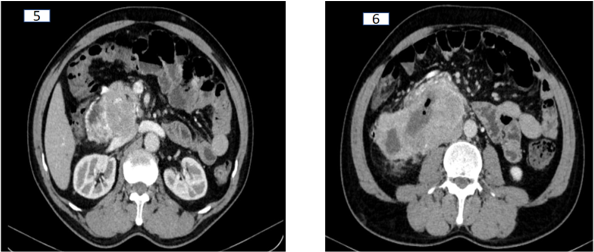
Inferiorly the mass appears large and fairly well circumscribed, extending posteriorly to abut and lie on the right renal vein and IVC. The mass retains maintained fat planes with portal vein, celiac and superior mesenteric artery (Images 5 and 6)
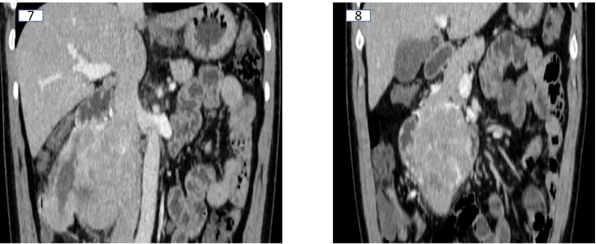
The mass enlarges inferiorly with a necrotic component and foci of air. It displaces the second and third part of duodenum anteriorly. There is extension in the wall of the second part of the duodenum, obliteration of the pancreaticoduodenal groove ( image 7 and 8 )
DIAGNOSIS:
Duodenal GIST arising from the 2nd/3rd part of duodenum
CLINICAL SIGNIFICANCE:
- All tumors in the region of the pancreas are not pancreatic in origin.
- This case highlights the importance of negative findings which help differentiate the origin of this tumor, namely : absence of PD dilatation, absence of vessel encasement/ involvement, absence of infiltrating retroperitoneal soft tissue / nodes in the presence of such a large mass .
- Anterior displacement of the 2nd and 3rd part of the duodenum as well as early pattern of enhancement , directs the features in favour of duodenal GIST/ neuroendocrine tumors, as opposed to a pancreatic adenocarcinoma.
DISCUSSION:
- GISTs in the duodenum are rare (less than 5%).
- As they are slow growing tumour, encasement of vessels is rare and they often contain areas of necrosis and air.
- Surgical resection with tumour free margin is the mainstay of treatment for the patients with primary GISTs without distant metastasis.
- Various parameters are described to predict the malignant potential of GIST, such as tumor size, mitotic activity, tumor location, non-radical resection, tumor rupture, peritoneal dissemination, metastasis, and invasion into adjacent organs.
- National Institute of Health (NIH) consensus criteria (Fletcher’s criteria) proposed risk stratification of tumor behavior based upon its size and mitotic activity. Tumors larger than 10 cm in size with any mitotic count or of any size with mitotic count more than 10/50 HPF are at high risk of aggressive behavior Adjuvant therapy with imatinib has been recommended in patients with substantial risk of relapse. Risk of relapse is increased in tumors of large size, increased mitotic activity and resection with positive margins. Adjuvant therapy with imatinib has been shown to increase the relapse-free survival but not overall survival
Conclusion:
- Duodenal gastrointestinal stromal tumors can grow exophytically into a large mass, involving the pancreas without infiltrating it and present as pancreatic head mass.
- In a large periampullary tumor with no jaundice, duodenal GIST should be considered.
References:
- Miki Y, Kurokawa Y, Hirao M, Fujitani K, Iwasa Y, Mano M, Nakamori S, et al. Survival analysis of patients with duodenal gastrointestinal stromal tumors. J ClinGastroenterol 2010 ;44:97- 101.[ PMID 19809358]
- Eisenberg BL, Trent JC. Adjuvant and neoadjuvantimatinib therapy: current role in the management of gastrointestinal stromal tumors. Int J Cancer 2011 ;129:2533-42. [PMID: 21671474]
- Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, et al Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol 2002; 33:459-465. [PMID:12094370]
- Agaimy A. Gastrointestinal stromal tumors (GIST) from risk stratification systems to the new TNM proposal: more questions than answers? A review emphasizing the need for a standardized GIST reporting. Int J ClinExpPathol. 2010; 3:461-71. [PMID: 20606727]
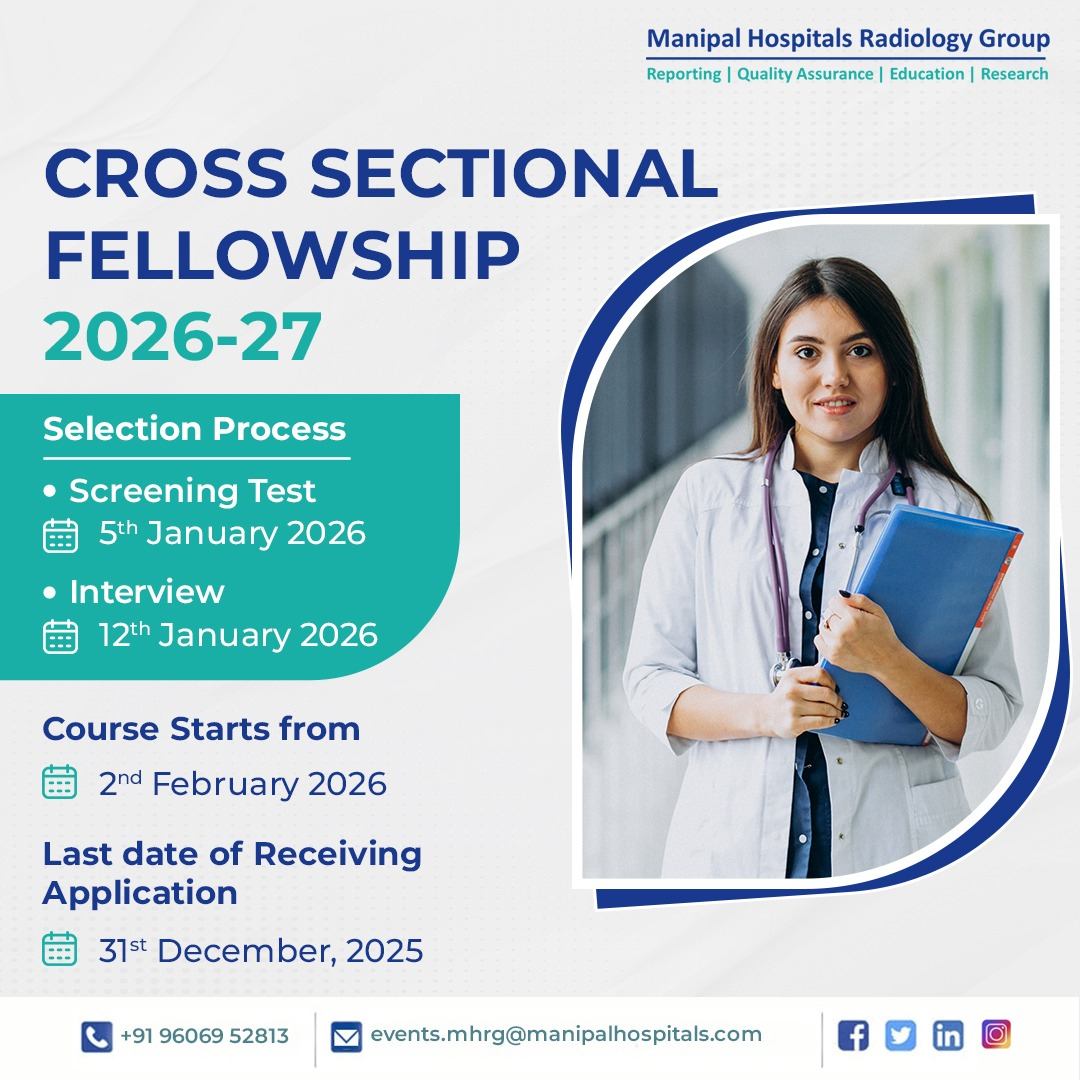
Dr Ankur Chandra
Cross Sectional Imaging Fellow
Manipal Hospitals Radiology Group.
Dr Sunita Gopalan,
DMRD, FRCR
Senior Consultant Radiologist
Manipal Hospitals Radiology Group.