41 year old G2P1L1 female patient at 8 weeks of gestation with a history of decreased appetite and pain abdomen. Retroviral positive on ART.
41 year old G2P1L1 female patient at 8 weeks of gestation with a history of decreased appetite and pain abdomen. Retroviral positive on ART.
On examination:
- Hepatomegaly.
- Abdominal distension
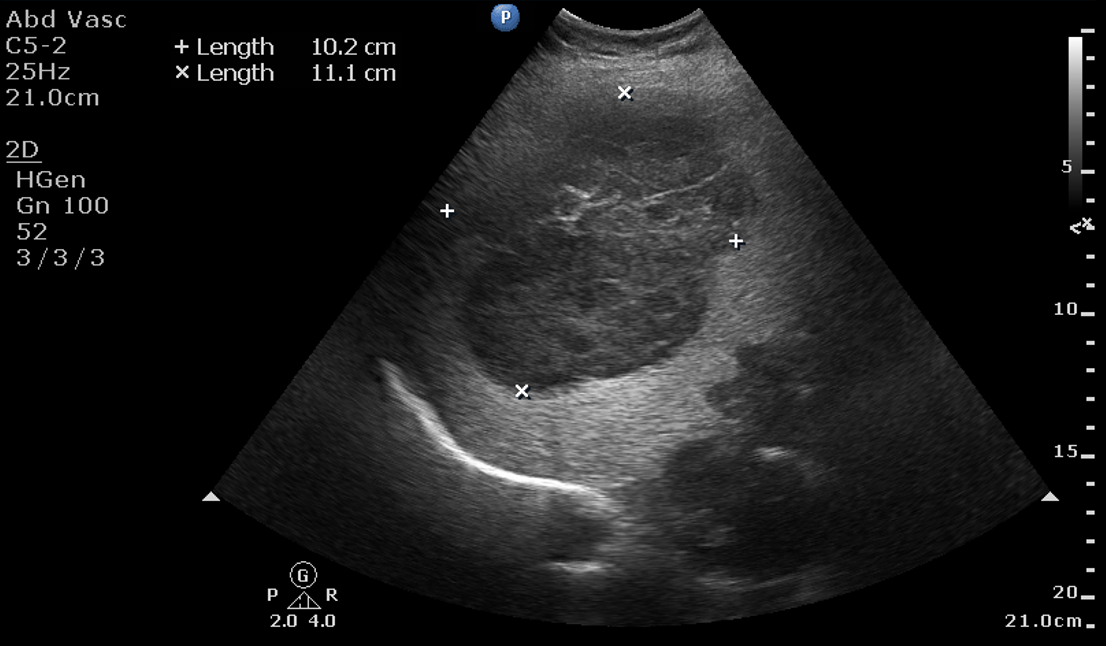
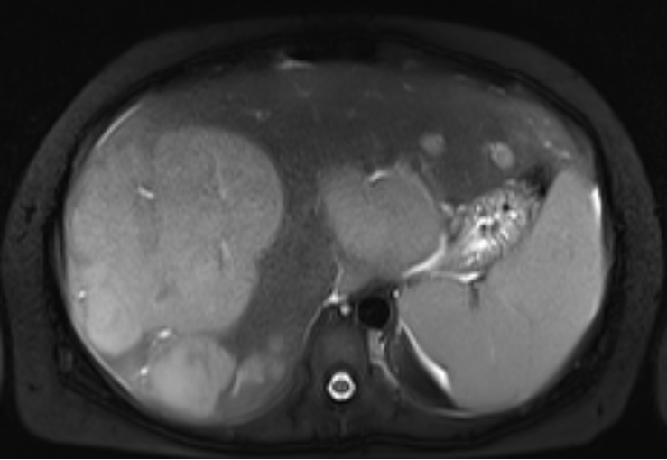
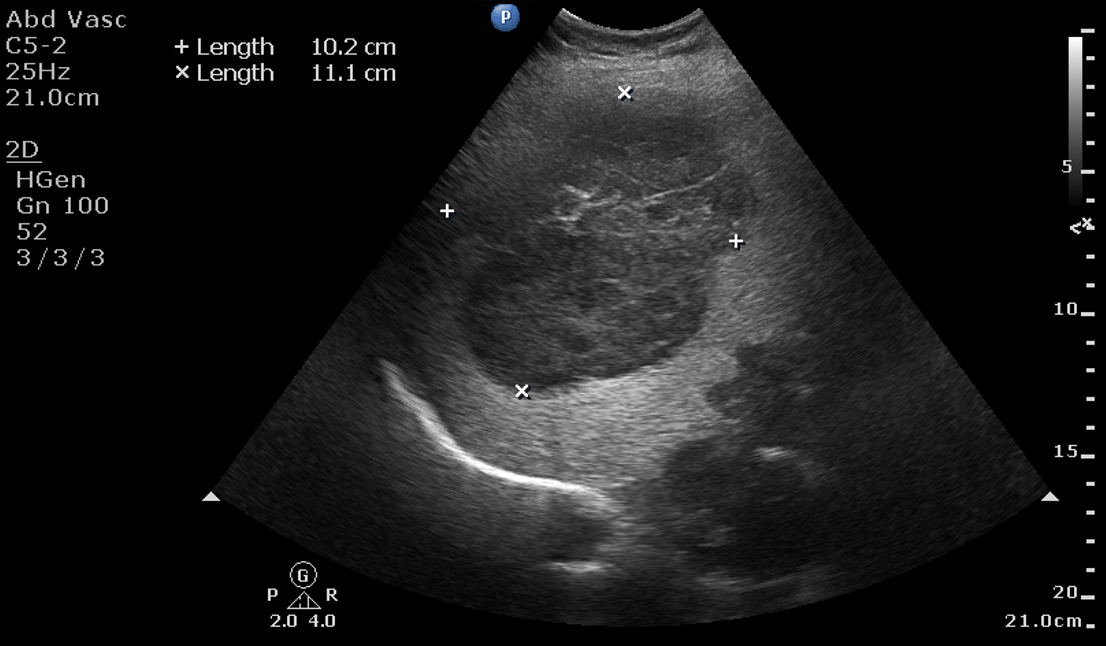
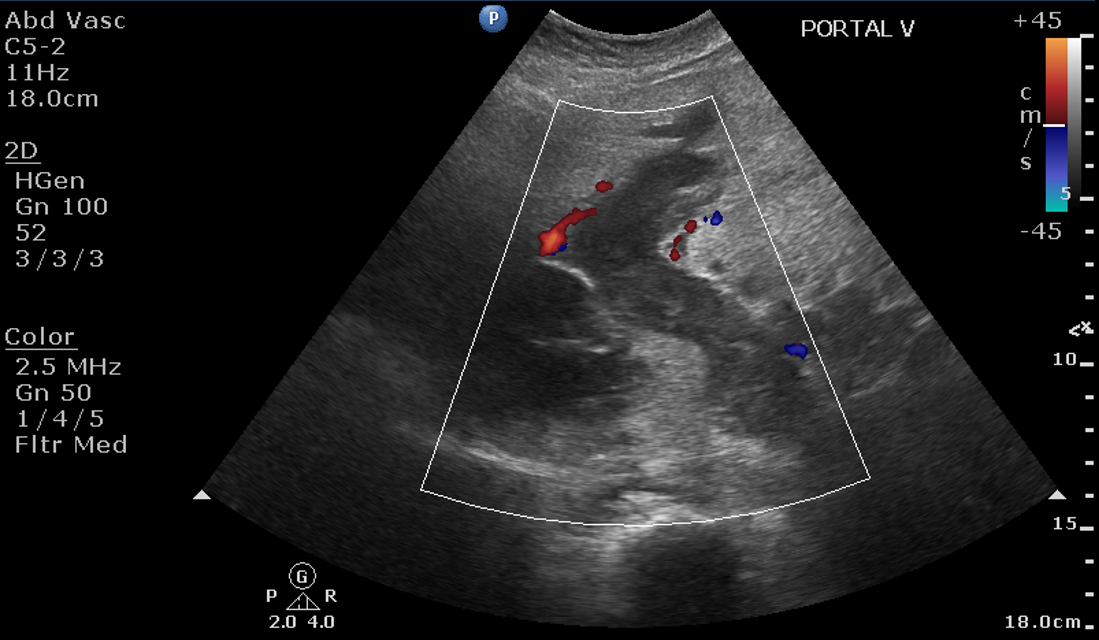
A.
- Liver is enlarged in size showing diffusely increased echotexture with a large heterogeneously hypoechoic lesion in the right lobe measuring 10.2 x 11.1 cm.
- Multiple similar echotexture lesions in the right lobe around the above lesion and in the left lobe.
- Dilated main portal vein, right and left branches of portal vein filled with echogenic intraluminal content - indicating complete portal vein thrombosis.
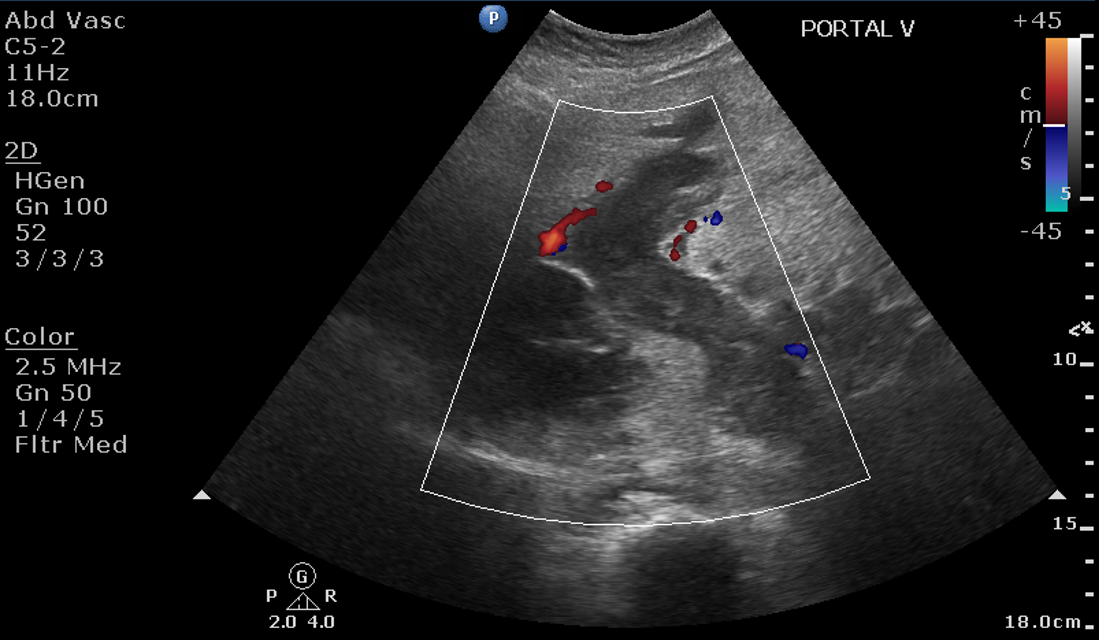
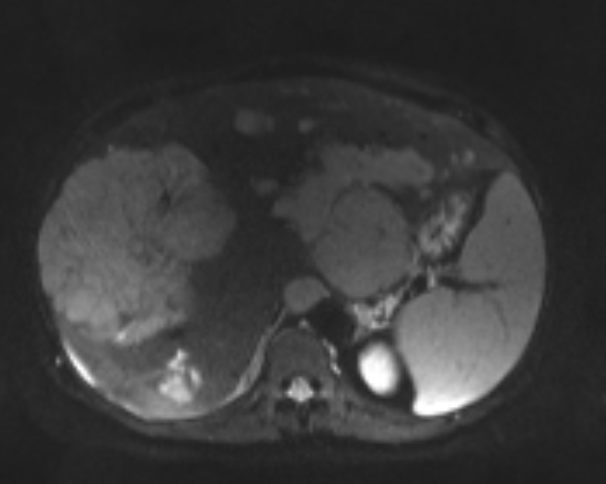
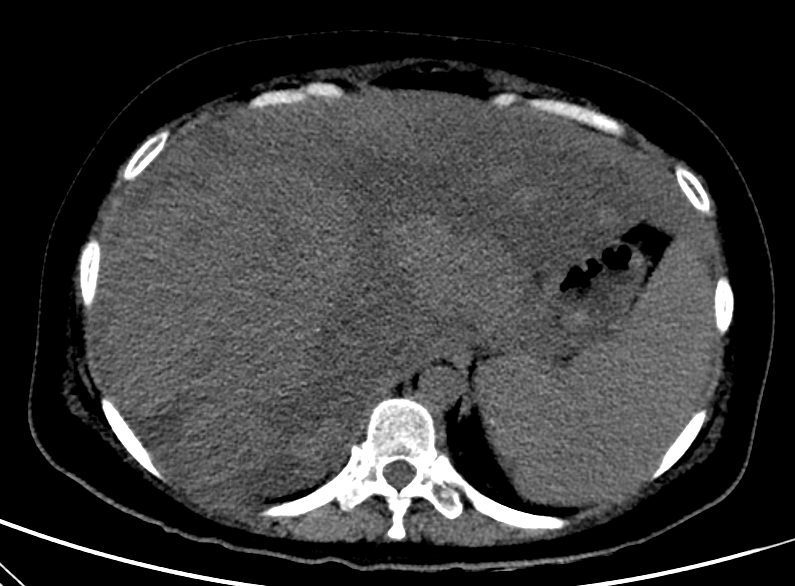
B.
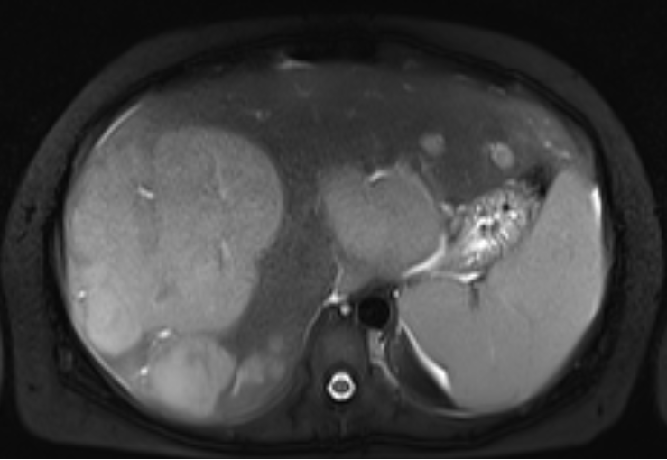
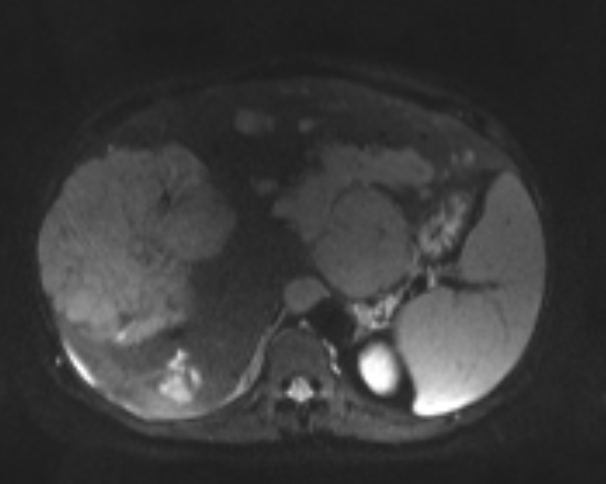
- Gross hepatomegaly.
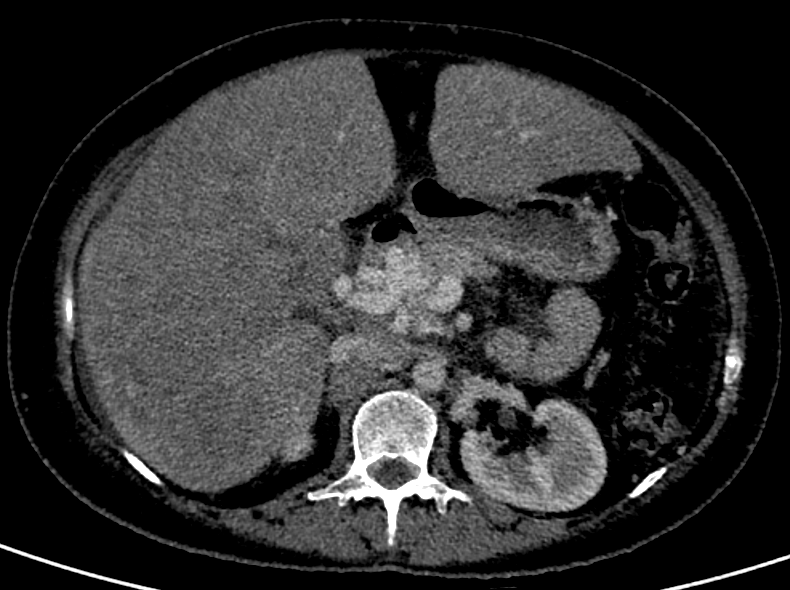
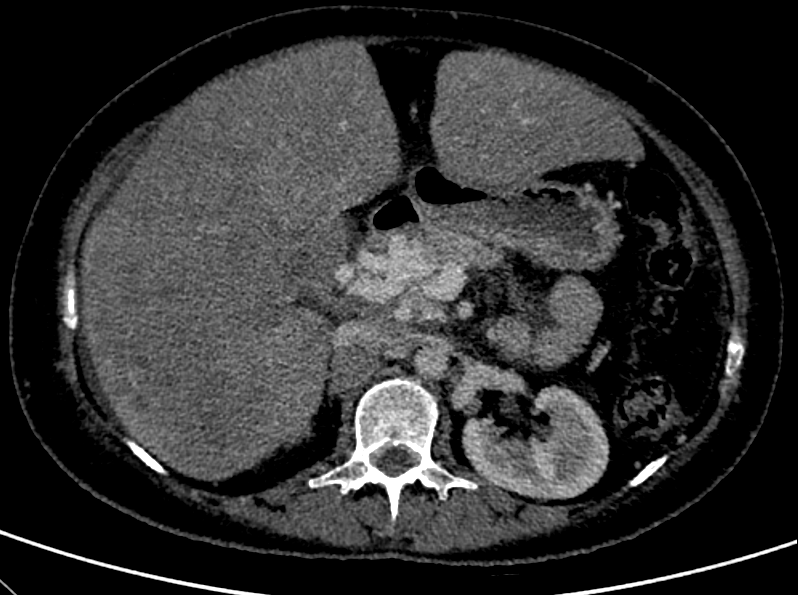
- Multiple varying sized but large lobulated coalescing lesions scattered in both lobes of the liver predominantly the right lobe.
- The lesions appear hyperdense on plain CT, with mild arterial phase hyperenhancement and no washout on delayed phase.
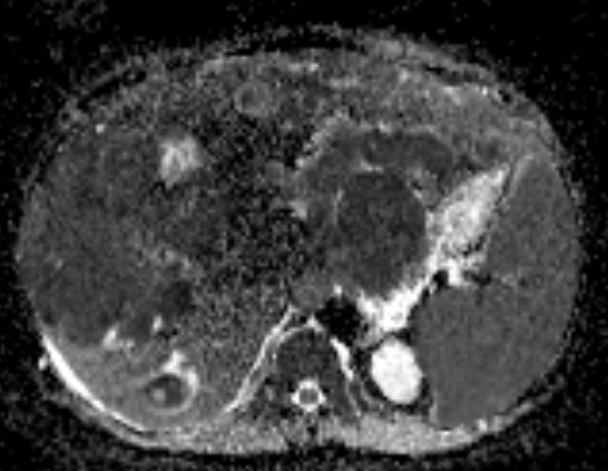
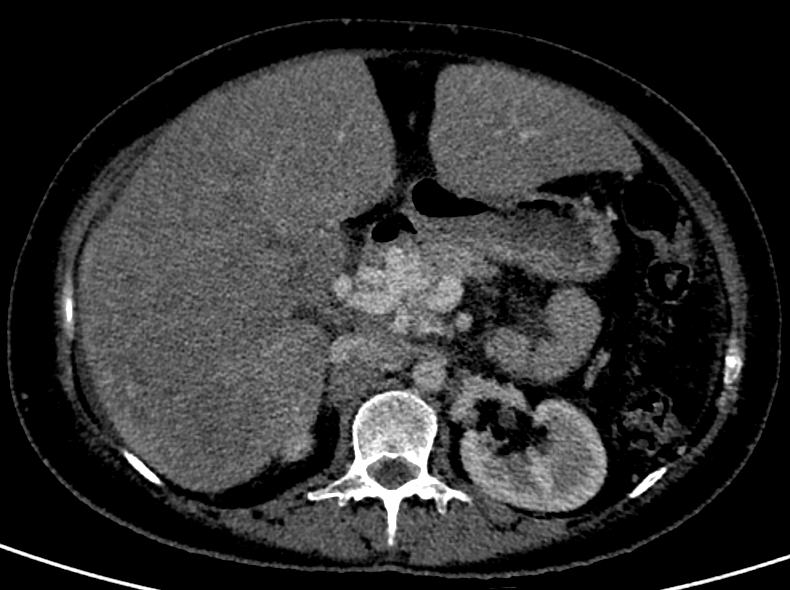
C.
- The main portal vein, right and left branches and the segmental branches of the portal vein to both lobes of the liver are dilated, show intraluminal content which has similar attenuation and enhancement pattern to the liver lesions – malignant portal vein thrombosis.
- Cavernous transformation of the main portal vein with multiple periportal and peripancreatic, tortuous and dilated collaterals.
- Mild splenomegaly.
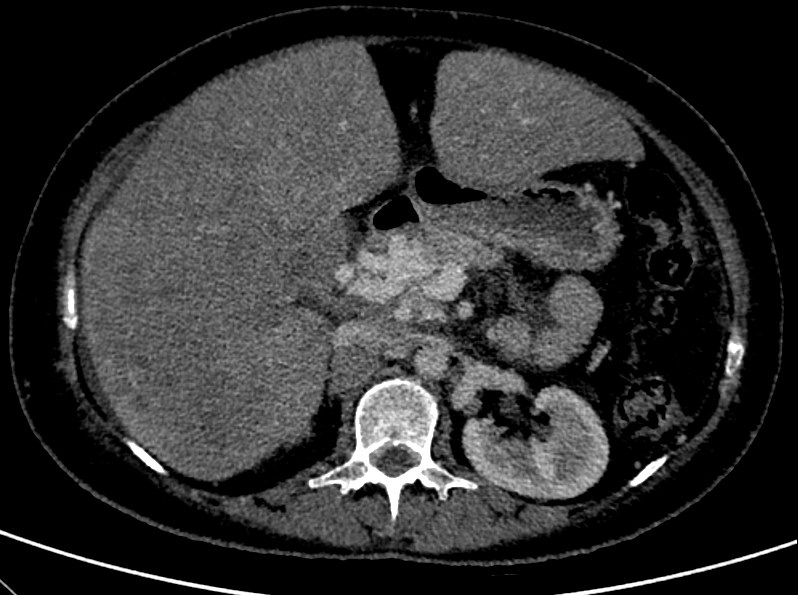
D.
- Multiple enlarged non-necrotic peripancreatic, para-aortic, aortocaval and mesenteric lymph nodes.
E.
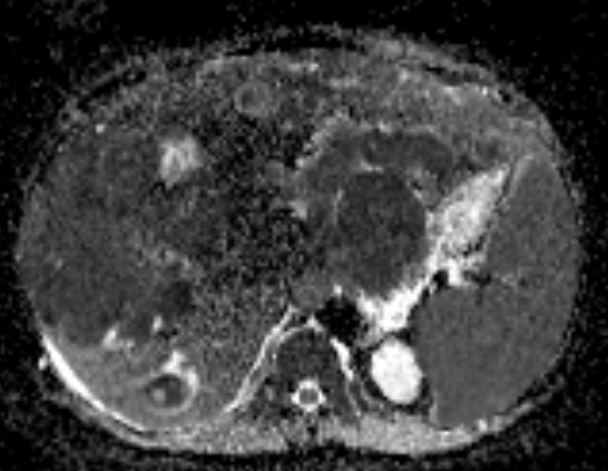
- Profound diffusion restriction of the lesions as well as the portal vein thrombus.
DIAGNOSIS
- Gross hepatomegaly showing multiple large lobulated lesions in both lobes, largest in the right lobe which show mild arterial phase hyperenhancement, with no washout.
- Dilated main portal vein, right and left branches and the segmental branches of the portal vein to both lobes of the liver filled with completely occluding thrombus which has similar attenuation and enhancement pattern to the liver lesions - indicating extensive intrahepatic malignant portal vein tumour thrombus. Secondary cavernous transformation of the main portal vein with multiple periportal and peripancreatic tortuous and dilated collaterals.
- Splenomegaly
- Peripancreatic and periportal lymphadenopathy.
- Mild ascites.
Features are likely suggestive of a malignant multifocal hepatic neoplasm. The following differentials need to considered : 1. Lymphoma 2. Kaposi sarcoma 3. Hepatocellular carcinoma.
HISTOPATHOLOGY
HPE AND IHC - High grade 'B' cell non-Hodgkin lymphoma expressing CMYC.
DISCUSSION:
- Hepatic lymphoma can be divided into its primary and secondary forms. To be classified as primary hepatic lymphoma, the disease should be limited to the liver and hilar lymph nodes, with no distant involvement (to the bone marrow or other sites).
- Primary hepatic lymphoma is defined as lymphoma that is confined to the liver and perihepatic lymph nodes, without evidence of involvement of other visceral organs, distant lymph nodes or bone marrow for at least 6-months after the onset of hepatic disease.
- The most common extra-nodal site of involvement by non-Hodgkin lymphoma is the gastrointestinal tract, secondary hepatic lymphoma being observed in nearly half of all patients with such involvement.
- Associated with prolonged immunosuppression (including that caused by infection with HIV) and Epstein-Barr virus, as well as with hepatitis B and C. The most common subtype of primary hepatic lymphoma is diffuse large B-cell lymphoma
- It can appear as a solitary (homogeneous or heterogeneous) mass or as multiple lesions, with or without a dominant lesion, or even in a miliary pattern characterized by multiple small discrete nodules. Other patterns include diffuse infiltration (with or without hepatomegaly) and a mass in the porta hepatis.
- Two different types of enhancement patterns have been recognized in lymphomatous nodules – 1. Minimal to no enhancement on all the phase 2. Enhancement of the rim of the lesion with a central non-enhancing area giving a target-like appearance
- Multiple vascular channels can often be seen coursing through the lesion. This has been referred to as the “vessel penetration sign”.
REFERENCES
- [1] Alves AMA, Torres US, Velloni FG, Ribeiro BJ, Tiferes DA, D'Ippolito G. The many faces of primary and secondary hepatic lymphoma: imaging manifestations and diagnostic approach. Radiol Bras. 2019 Sep-Oct;52(5):325-330. doi: 10.1590/0100-3984.2018.0013. PMID: 31656351; PMCID: PMC6808615.
- [2] Rajesh S, Bansal K, Sureka B, Patidar Y, Bihari C, Arora A. The imaging conundrum of hepatic lymphoma revisited. Insights Imaging. 2015 Dec;6(6):679-92. doi: 10.1007/s13244-015-0437-6. Epub 2015 Oct 6. PMID: 26443451; PMCID: PMC4656246.
- [3] Jiang, Minzhi MMa; Jiang, Shudian MMa; Yang, Yu MMa; Yao, Rucheng MDb; Hu, Mingzheng MDb,*. Primary hepatic lymphoma a case report and literature review. Medicine 102(50):p e36688, December 15, 2023. | DOI: 10.1097/MD.0000000000036688
Dr Y VIKHYATH SHETTY
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr PRIYANKA ROUT
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.