28-year-old with the history of abdomen pain with multiple episodes of vomiting.
- NCCT abdomen and pelvis coronal image (A) demonstrates diffusely oedematous small bowel loops (yellow arrows) with distended hyperdense portal vein. CECT pelvis axial image (B) demonstrates moderate ascites with dependent debris, suggestive of hemoperitoneum.
- NCCT abdomen coronal MIP image (C) demonstrates a distended hyperdense portal vein, SMV, and its tributaries (yellow arrows). CECT venous phase coronal image (D) demonstrates a filling defect in the portal vein, SMV, and its tributaries – thrombosis.
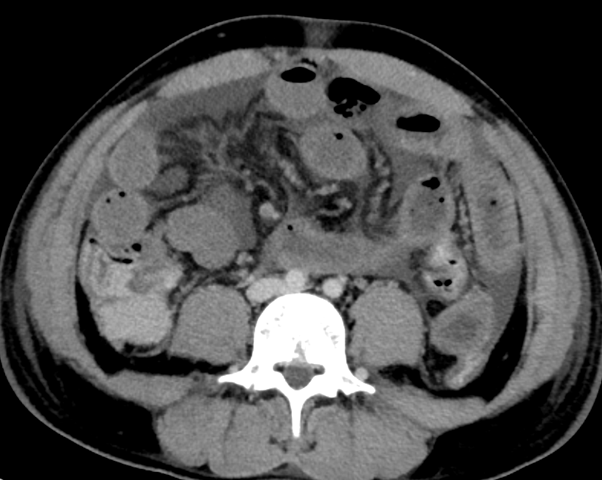
- CECT axial image (E) demonstrates diffusely oedematous small bowel loops (yellow arrow) and intraluminal hyperdense content in the cecum (green arrow) with inter bowel loop free fluid and mesenteric congestion.
- Post-operative image (F) shows long segment gangrenous small bowel loops.
Diagnosis:
Acute veno-occlusive mesenteric ischemia.
Discussion:
- Acute mesenteric ischemia is a rare life-threatening condition. The causes of AMI include arterial embolism, arterial thrombosis, venous thrombosis, and nonocclusive mesenteric ischemia.
- The prognosis for patients with AMI depends on the time to diagnosis and initiation of management. The mortality rate increases to 80%–100% with a delay of more than 24 hours after symptom onset.
- Patients with suspected AMI, CECT should be the first-line imaging modality for correct diagnosis and to exclude other causes of acute abdomen.
Mesenteric Venous Thrombosis:
- 5%–10% of all AMI cases. MVT usually occur in younger populations.
- Obstructed venous flow secondary to thrombosis, bowel wall oedema and luminal distention, which decrease arterial inflow and consequently lead to bowel ischemia.
- Most commonly underlying cause of MVT are portal hypertension, hypercoagulable states, right-sided heart failure, abdominal trauma, abdominal infection, acute pancreatitis, malignancies, nephrotic syndrome, cirrhosis, or splenomegaly.
Imaging findings:
- Luminal filling defects surrounded by rim-enhanced venous walls.
- Bowel wall thickening is often prominent, and fat stranding in the mesentery and ascites are common findings.
- The bowel wall typically shows a halo or target pattern of enhancement and rarely hyperenhancement. Bowel wall enhancement is absent or diminished in cases with severe ischemia.
- Key findings indicating irreversible ischemia in MVT include (a) absent bowel wall enhancement, (b) pneumatosis and/or porto-mesentric venous gas, and (c) extra bowel gas.
Differential diagnosis:
- Inflammatory bowel disease.
- Infectious enterocolitis.
- Graft-versus-host disease.
- Radiation enteritis.
- Portal hypertension.
REFERENCES:
- Kanasaki S, Furukawa A, Fumoto K et al.Acute Mesenteric Ischemia: Multidetector CT Findings and Endovascular Management. Radiographic 2018;38 (3):945–961.
- Fitzpatrick, L. A., Rivers-Bowerman, M. D., Thipphavong, S., Clarke, S. E., Rowe, J. A., & Costa, A. F. (2020). Pearls, Pitfalls, and Conditions that Mimic Mesenteric Ischemia at CT. RadioGraphics, 40(2), 545–561. doi:10.1148/rg.2020190122.
- Contrast-Enhanced CT for the Diagnosis of Acute Mesenteric Ischemia. Lorenzo Garzelli1, Alexandre Nuzzo2,3, Pauline Copin1,2, Paul Calame4, Olivier Corcos3, Valérie Vilgrain1,2,5 and Maxime Ronot1,2,5. doi.org/10.2214/AJR.19.22625.
Dr. Bhupendar Singh
Radiology resident- Manipal Hospitals Radiology Group.
Dr. Vikhyath Shetty,
MD RD
Consultant Radiologist
Manipal Hospitals Radiology Group.
Dr. Sunita Gopalan
DMRD, FOR
Senior Consultant Radiologist
Manipal Hospitals Radiology Group.