27-year-old with long standing seizure.
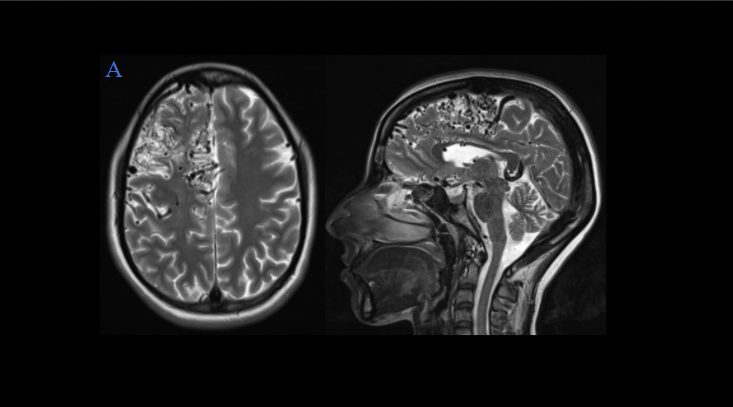
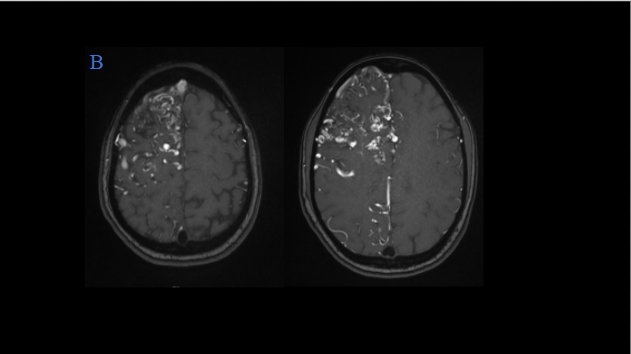
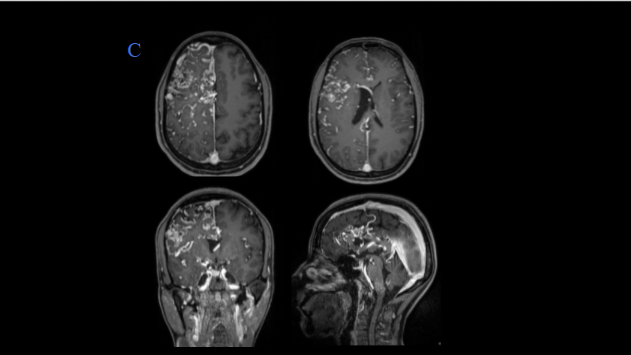
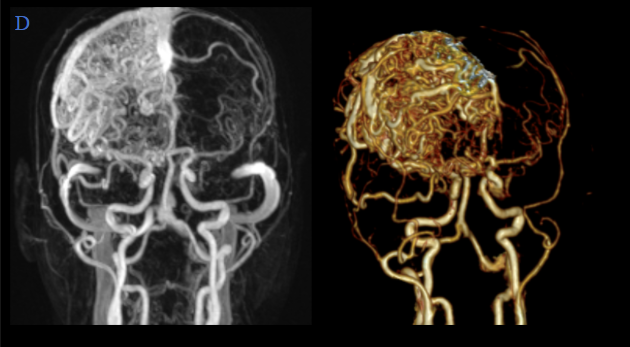
Representative T2W axial, and sagittal images, MR angiography, and post-contrast T1W with MIP/VR images show –
- Multiple prominent flow voids suggestive of nidus seen diffusely in right frontal lobe.
- Multiple hypertrophic arterial feeders are seen arising from right MCA and ACA branches.
- Multiple dilated draining cortical veins are seen draining into the superior sagittal sinus. Venous drainage also seen into the pericallosal vein which is draining to vein of Galen.
- No evident aneurysm/intracranial hemorrhage is seen.
- Significant adjacent gliosis and volume loss seen in the right frontal lobe.
DIAGNOSIS:
Cerebral proliferative angiopathy
DISCUSSION:
- Cerebral proliferative angiopathy, previously known as diffuse nidus type AVM, is present in an estimated 2%–4% of all brain AVMs. It is thought to be an entity separate from classic brain AVM.
- There is a female predilection of 2:1, with a rather young mean patient age (20 years).
- Progressive neurologic deficits, transient ischemic attacks, seizures, and headaches are the common presenting symptoms, with haemorrhage being extremely rare.
- Although its aetiology is unknown, the disease is characterized by endothelial proliferation and angiogenesis. The “nidus” is composed of multiple arteries as an angiogenetic response to cortical ischemia.
- The typical imaging findings include a diffuse proliferative type nidus in which normal brain parenchyma is interspersed between the abnormal vessels. Often, an entire lobe or even brain hemisphere is affected. MR imaging are seen as tubular flow voids on T1W and T2W sequences with abnormal, enlarged serpiginous vessels seen on contrast-enhanced images. Secondary features such as dilated proximal intracranial or extracranial arteries are also demonstrated. Chronic hemorrhage, gliosis, or both can be seen in the brain tissue adjacent to the abnormal vessels.
- Treatment options largely depend on the clinical presentation. There is a risk of permanent neurological damage to the normal interspersed brain parenchyma if surgery or radiosurgery is performed hence patients with controlled seizures and headaches can be monitored expectantly with the understanding that the patient would have small risk of hemorrhage (12%) or other neurological symptoms such as seizures or focal deficit. Limited arterial embolization in noneloquent areas can be performed for patients presenting with uncontrolled seizures and headaches. Pial synangiosis or burr-hole therapy to enhance supply to healthy brain tissue from the external carotid artery.
References:
1. Rohit, Goh PS. Diffuse Proliferative Cerebral Angiopathy: A case report and review of the literature. J Radiol Case Rep. 2015;9(9):1-10. Published 2015 Sep 30. doi:10.3941/jrcr.v9i9.2402.]
2. Lasjaunias PL, Landrieu P, Rodesch Get al. Cerebral proliferative angiopathy: clinical and angiographic description of an entity different from cerebral AVMs.
Dr. Sriram Patwari
MD, PDCC (Neuroradiology), EDiNR
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru
Dr Abhilash K
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru