15years old female came with history of cough, shortness of breath and asthma.
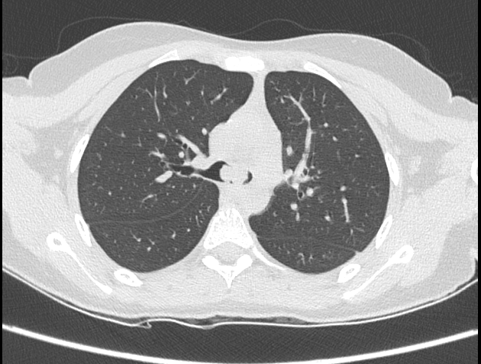
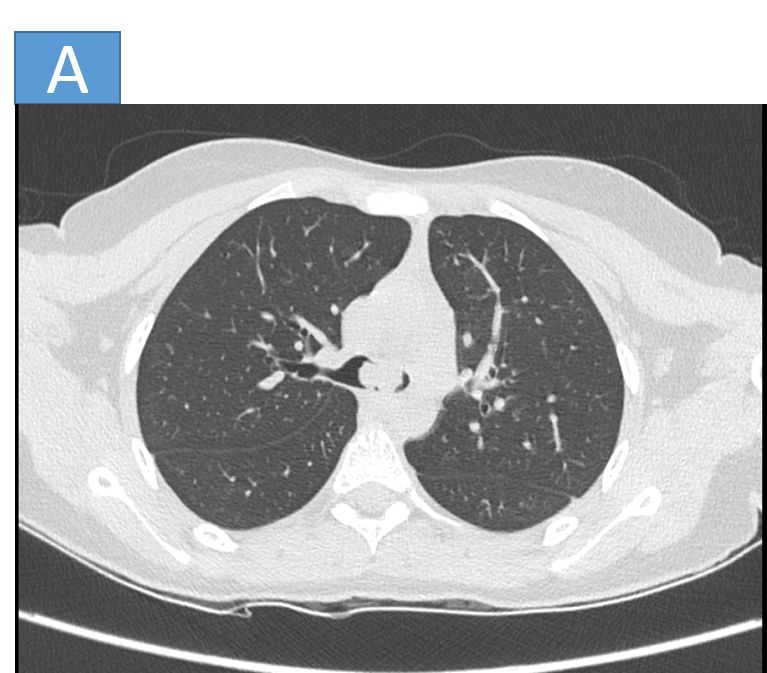
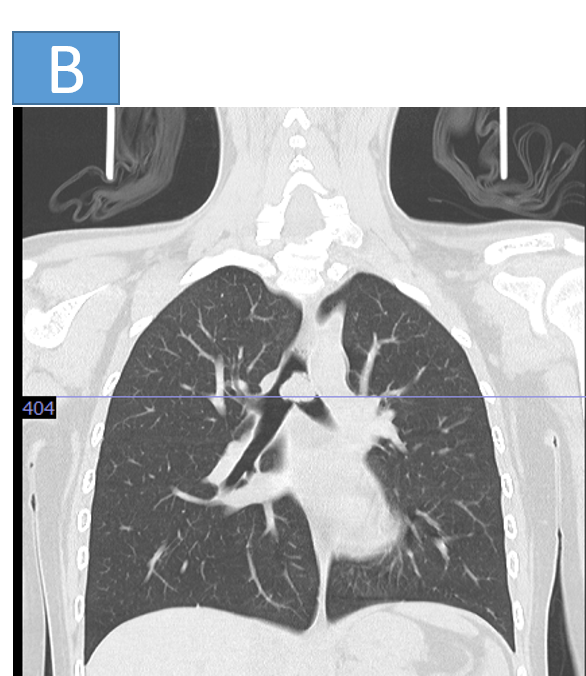
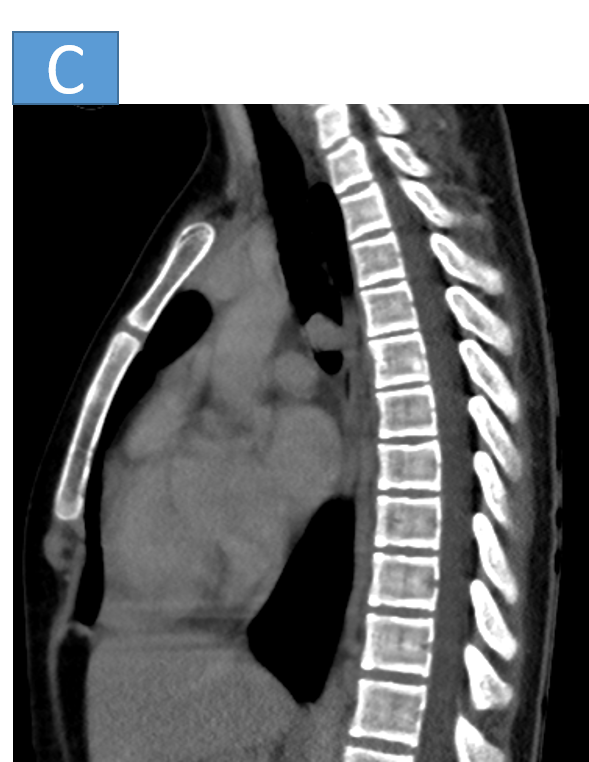
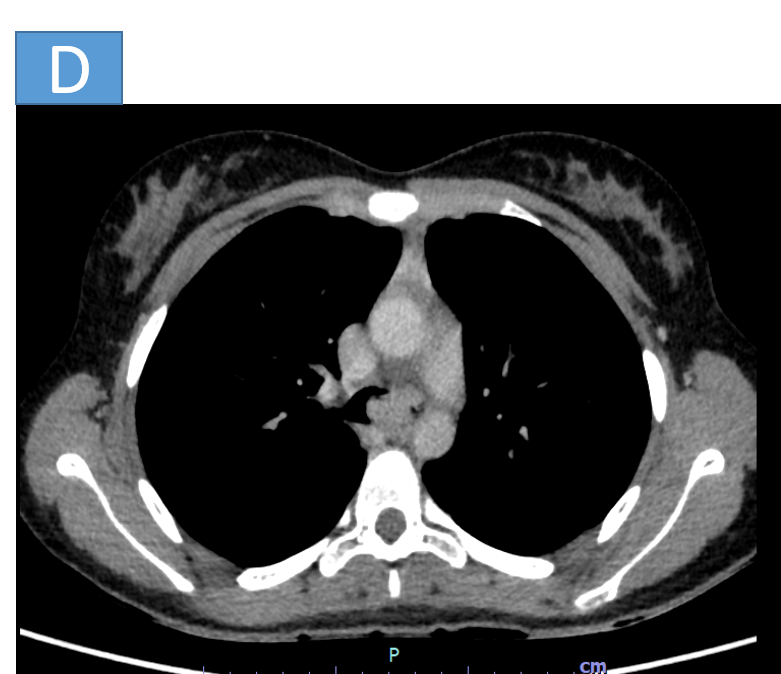
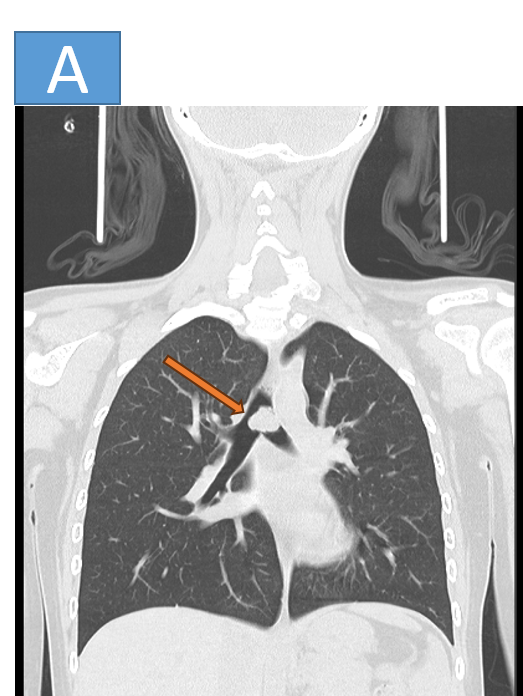
- Fig 1 & 2. A solid endotracheal lesion (orange arrow) showing homogeneous contrast enhancement involving distal trachea immediately above the carina, extending into left main bronchus and significantly compromising the left main bronchial airway.
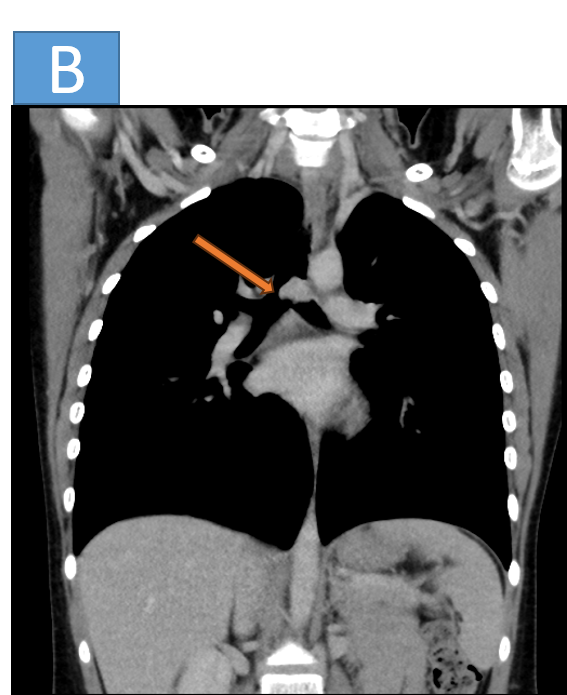
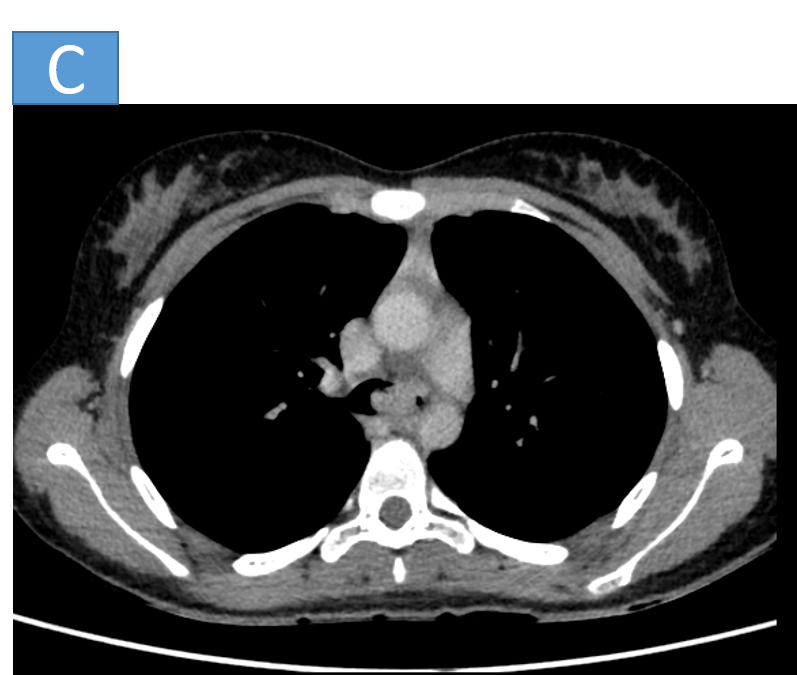
- Fig 3. The lesion is irregularly attached to the left anterolateral wall of distal trachea from 1-3 o'clock position. No obvious extraluminal extension.
DIAGNOSIS:
- Inflammatory myofibroblastic tumor (Histopathology proven)
DISCUSSION:
Inflammatory myofibroblastic tumours:
Constitute a rare group of neoplasms composed of a mixture of spindle-shaped myofibroblasts or fibroblasts and a variable amount of inflammatory cells
Different etiologies have been proposed:
- Chronic infections,
- Autoimmune diseases,
- Trauma,
- Specific inflammatory diseases, such as IgG4 disease
In some cases, an aggressive behaviour with metastases has been described.
Histopathological identification is crucial in diagnosis as it is often misdiagnosed and confused with other neoplasms even by experienced pathologists owing to its low occurrence and a wide variety of presentation.
Tracheal IMF is very rare, accounting for less than 1% of all respiratory tract tumors [1]. It has been reported in the pediatric age group.
Clinical features:
- The clinical symptoms are usually nonspecific, and include chronic cough, hemoptysis, pleuritic chest pain, stridor, and post-obstructive pneumonia.
Imaging:
- Chest X-ray is usually noncontributory to any diagnosis. Cross-sectional imaging studies such as CT and MRI help in assessing the overall extent of the lesion as well as the degree of airways involvement.
- CT scan often reveals a well-defined, circumscribed, polypoidal endotracheal soft-tissue mass lesion. The lesion usually causes significant tracheal luminal obliteration.
- Broad basal nodule with significant enhancement.
- Calcification and necrosis are less commonly seen findings. Exophytic component is not associated.
- Even though the tumor is mostly benign, recurrence is common. Considering the higher recurrence rate, that ranges from 18% to 40%, locally invasive behavior of the lesion and its metastatic potential, complete margin free surgical resection of the lesion is the gold standard.
Reference:
- Pavithran K, Manoj P, Vidhyadharan G et-al. Inflammatory myofibroblastic tumor of the lung: unusual imaging findings. World J Nucl Med. 2013;12 (3): 126-8. doi:10.4103/1450-1147.136739
- Van den Heuvel DA, Keijsers RG, van Es HW et-al. Invasive inflammatory myofibroblastic tumor of the lung. J Thorac Oncol. 2009;4 (7): 923-6. doi:10.1097/JTO.0b013e3181a76e28
Dr Pravin kumar M
MBBS, DMRD, DNB
Senior Consultant Manipal Hospitals Radiology Group Hebbal.
Dr Sanjana.N
MBBS, M.D.
Cross section imaging fellow - MHRG