12-year-old female patient with history of a painless neck swelling on the left side for the past 2 weeks. No history of difficulty in swallowing, breathing or changes in voice.
12-year-old female patient with history of a painless neck swelling on the left side for the past 2 weeks. No history of difficulty in swallowing, breathing or changes in voice.
On examination:
- A firm swelling of size approximately 4 x 4cm in the left posterior triangle.
- No palpable pulsation over the swelling
- Restricted neck mobility
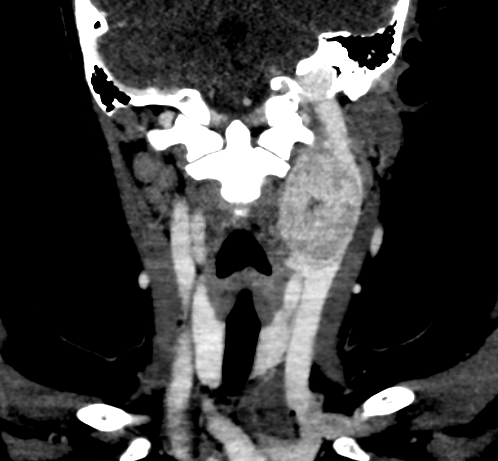
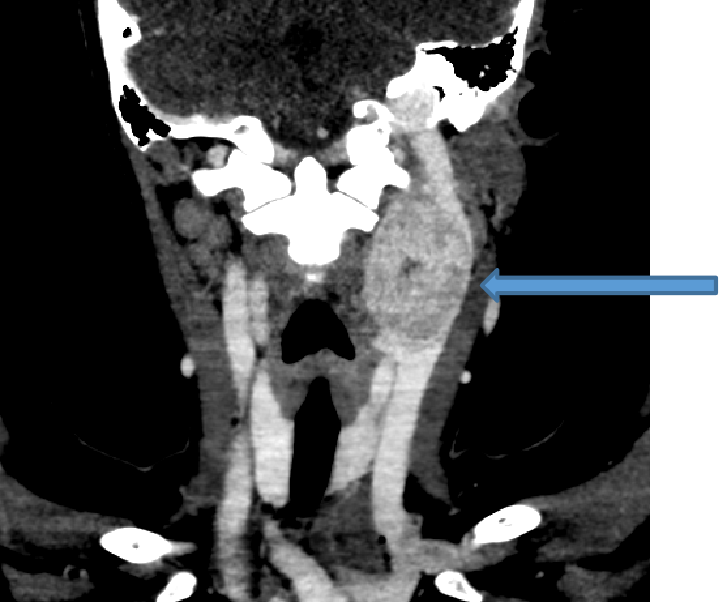
A.
- Well defined avidly enhancing soft tissue lesion in left carotid space.
- Extends from C2 till the superior border of C5.
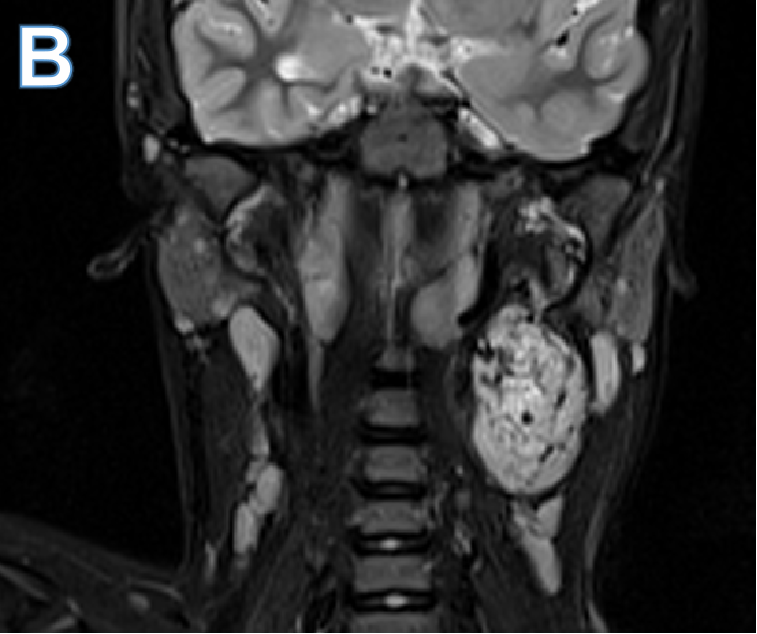
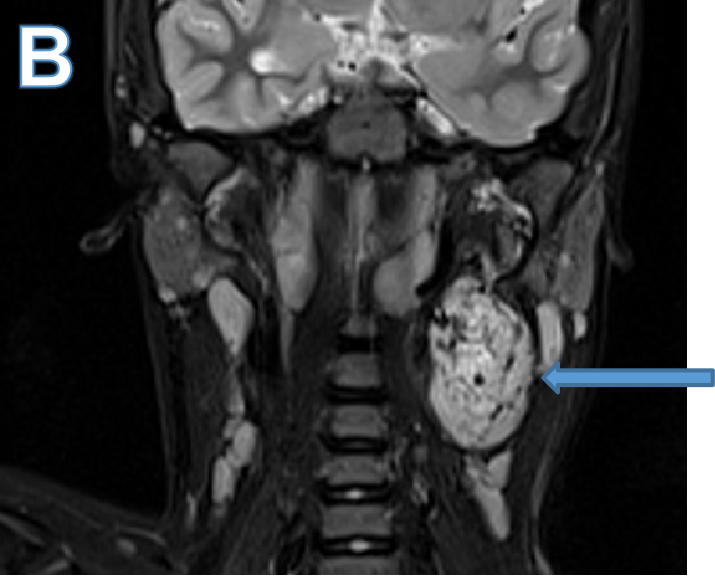
B.
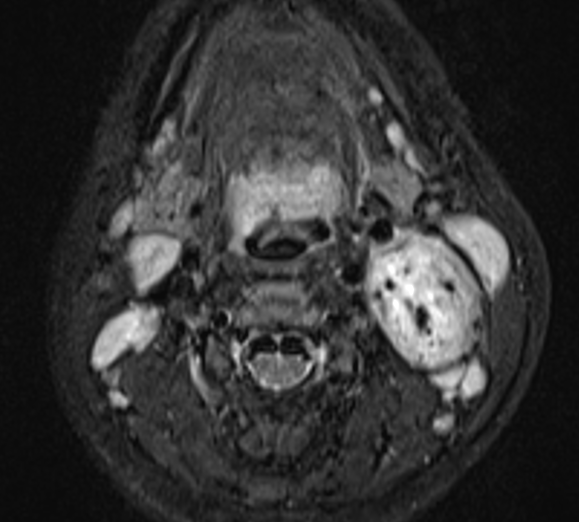
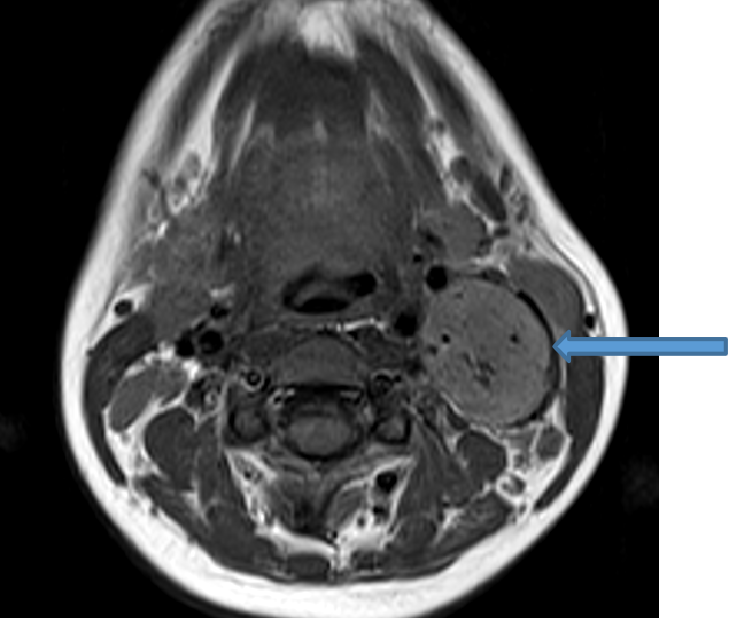
- Large well defined T2 hyperintense ovoid lesion in the left carotid space with multiple prominent internal flow voids.
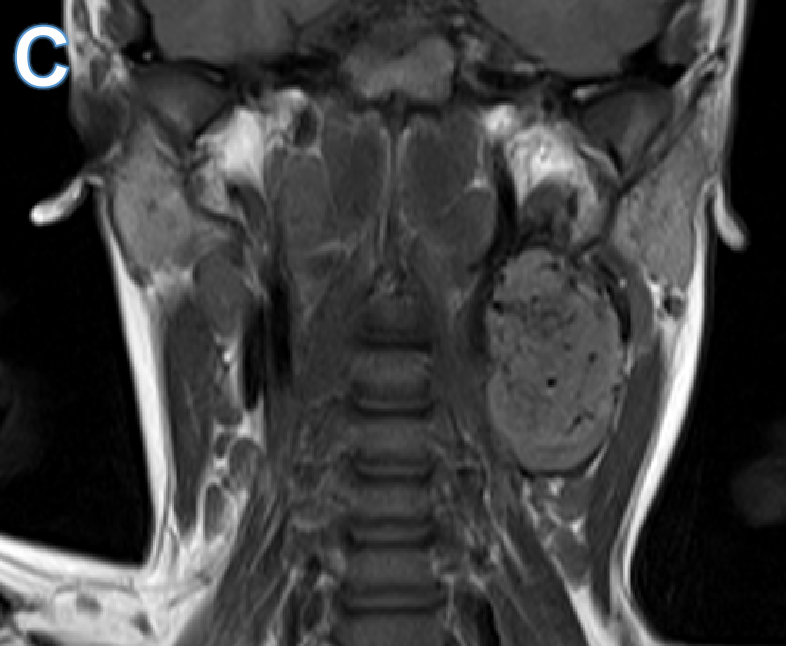
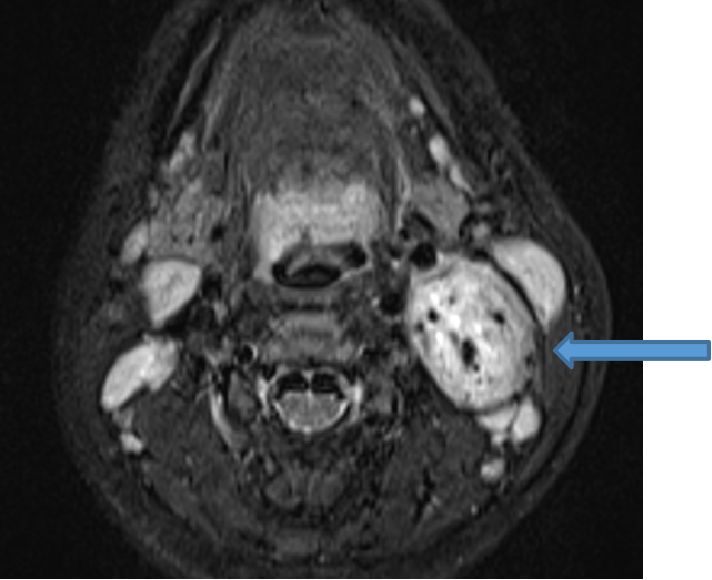
C.
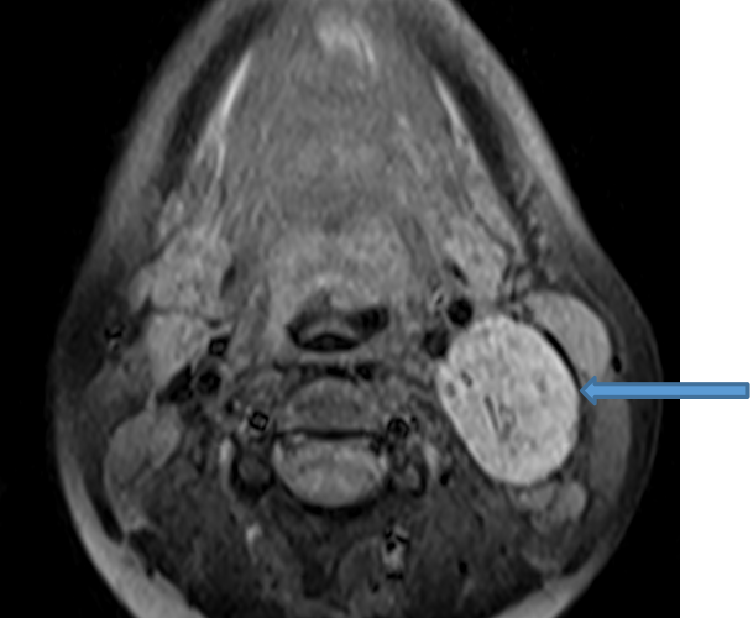
- Isointense on T1 sequences.
- Lesion abuts and displaces the distal left common carotid, proximal internal and external carotid arteries anteromedially.
- No widening of carotid bifurcation.
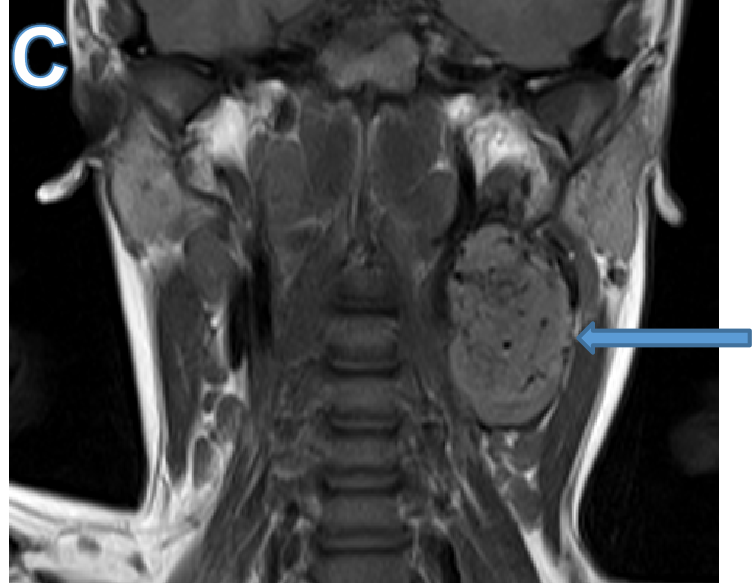
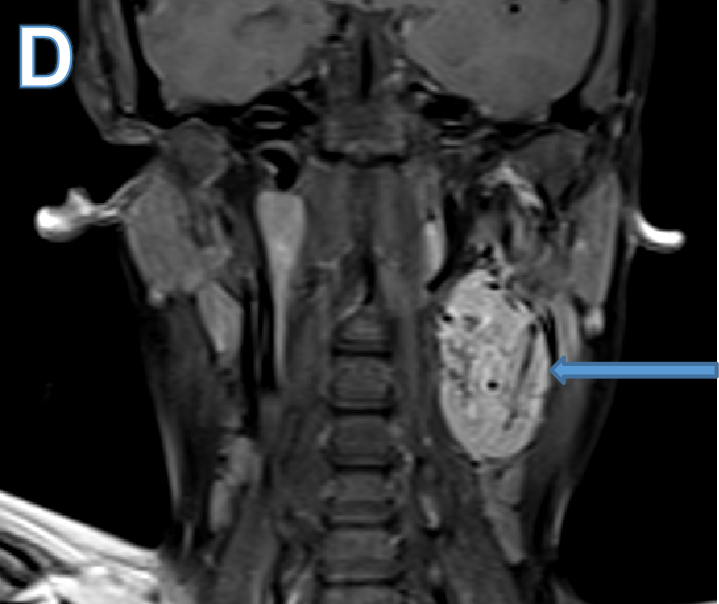
D.
- Intense post-contrast enhancement.
DIAGNOSIS:
- Large intensely enhancing mass lesion with left carotid space with multiple internal flow voids.
- Head and neck paraganglioma, likely glomus vagale/ sympathetic chain paraganglioma. (Netterville-Glasscock group A).
DISCUSSION:
- Paragangliomas are hypervascular neuroendocrine tumors arising from the paraganglia.
- Head and neck paragangliomas arise predominantly along branches of the glossopharyngeal nerve (CN IX) and vagus nerve (CN X), most commonly in the carotid body, followed by the middle ear, jugular foramen, ganglion nodosum, larynx, and cervical sympathetic chain.
- Vagal PGLs occur anywhere along the vagus nerve but most commonly arise from the ganglion nodosum or plexiform ganglion, which are located below the skull base but above and medial to the carotid bifurcation.
- Vagal PGLs displace the internal carotid artery anteromedially and jugular vein posterolaterally. When large, they can extend to the carotid bifurcation and invade the skull base.
- The Netterville-Glasscock classification categorizes vagal PGLs by degree of skull base involvement, with group A confined to the neck, group B extending to the jugular foramen, and group C invading beyond the jugular foramen.
- Gallium 68 Somatostatin receptor imaging has superior sensitivity over all other cross-sectional and functional imaging modalities in helping detect PGLs.
REFERENCES
- Lin, Edward P., et al. "Head and neck paragangliomas: an update on the molecular classification, state-of-the-art imaging, and management recommendations." Radiology: Imaging Cancer 4.3 (2022): e210088.
- Thelen J, Bhatt AA. Multimodality imaging of paragangliomas of the head and neck. Insights Imaging. 2019 Mar 4;10(1):29. doi: 10.1186/s13244-019-0701-2. PMID: 30830483; PMCID: PMC6399371.
- Graham NJ, Smith JD, Else T, Basura GJ. Paragangliomas of the head and neck: a contemporary review. Endocr Oncol. 2022 Nov 10;2(1):R153-R162. doi: 10.1530/EO-22-0080. PMID: 37435464; PMCID: PMC10259325.
Dr RAHUL KARTHIK LINGUTLA
Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr PRIYANKA ROUT
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.