10-year-old boy presented with soft non-tender compressible swelling in the left infraorbital region and the swelling increase in size while leaning forward
- 10-year-old boy presented with soft non-tender compressible swelling in the left infraorbital region and the swelling increase in size while leaning forward
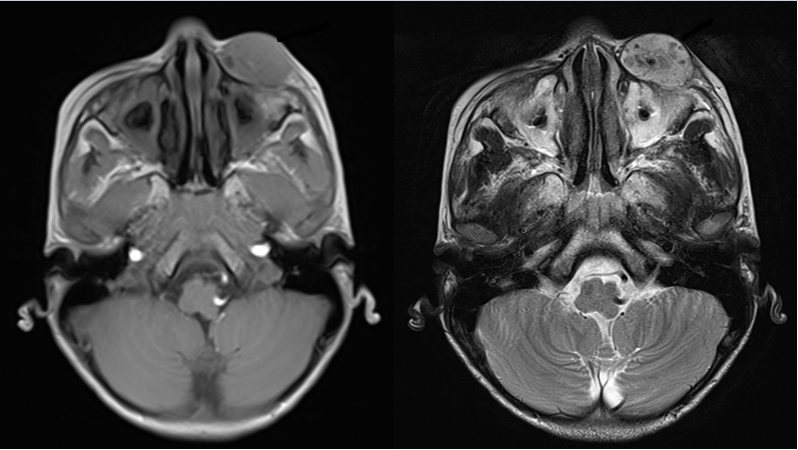
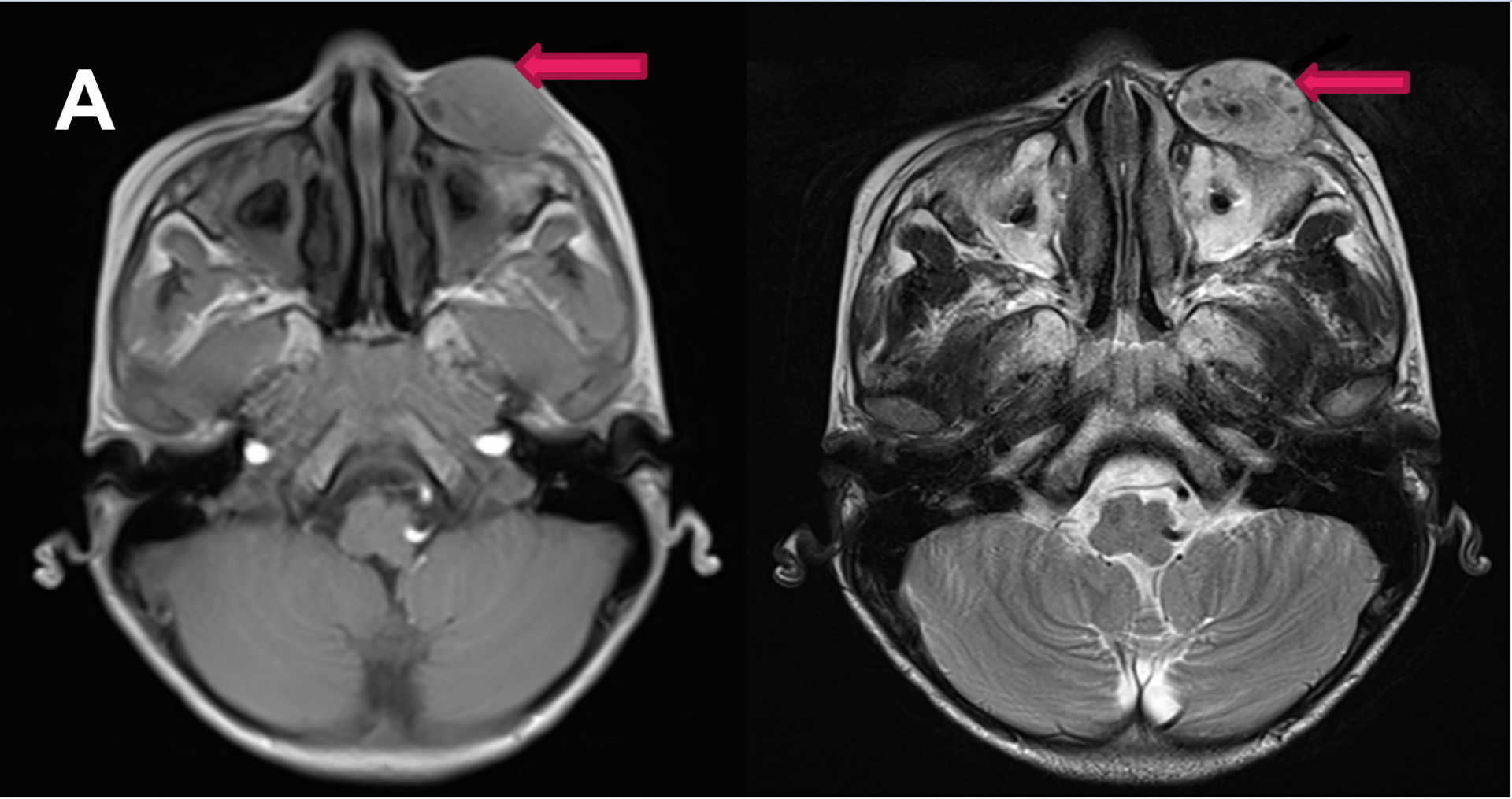
- A. A well defined T1 isointense, T2 hyperintense lesion with internal T1/T2 hypointense foci (Phleboliths) in the left infraorbital region.
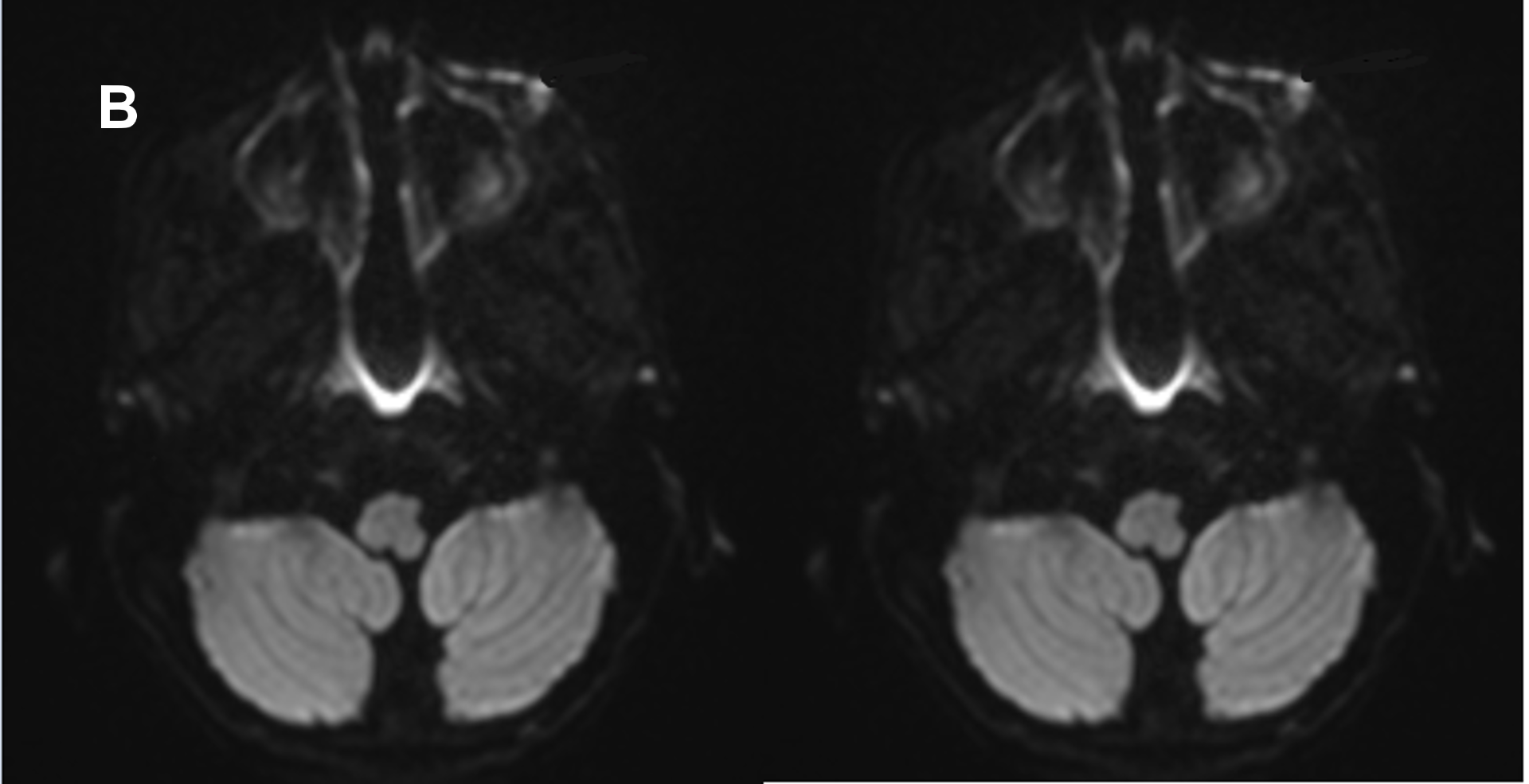
- B. No features of diffusion restriction in DWI/ ADC images.
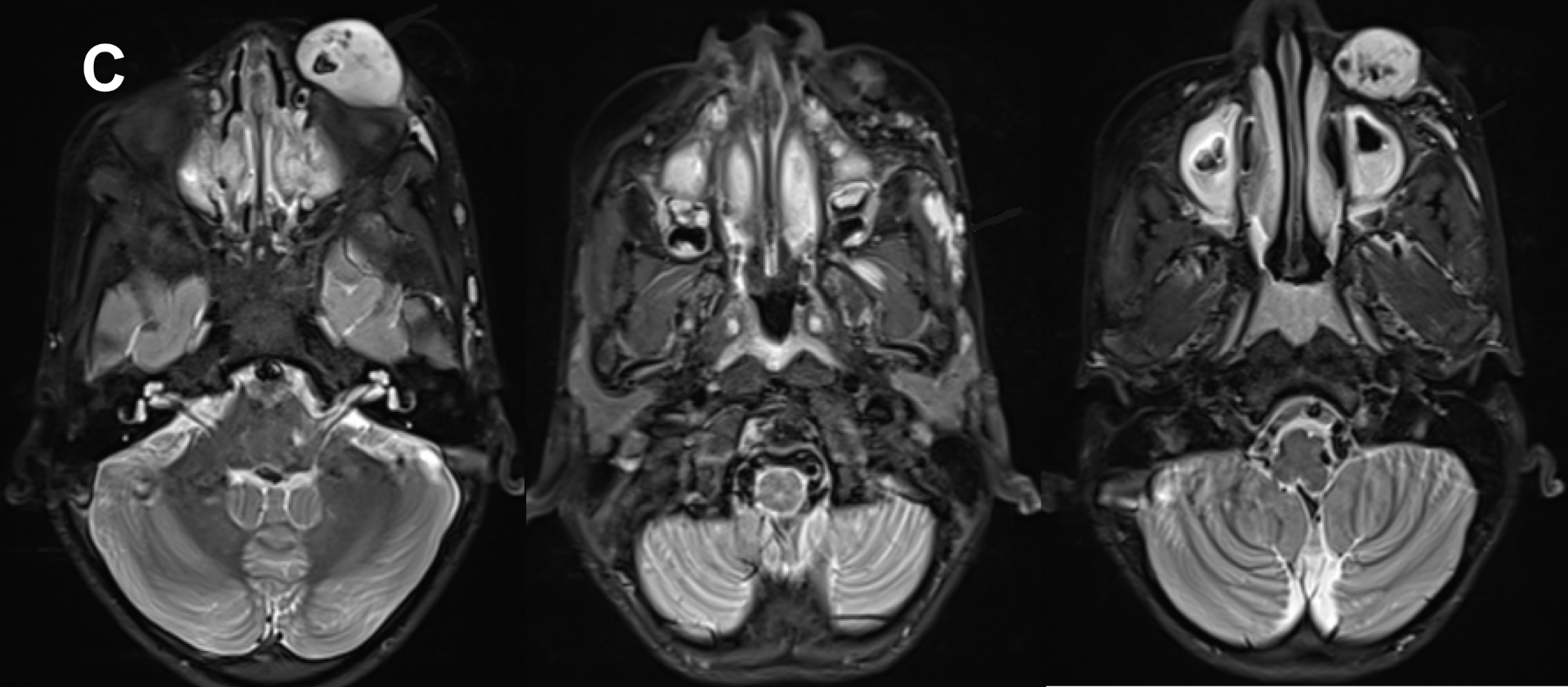
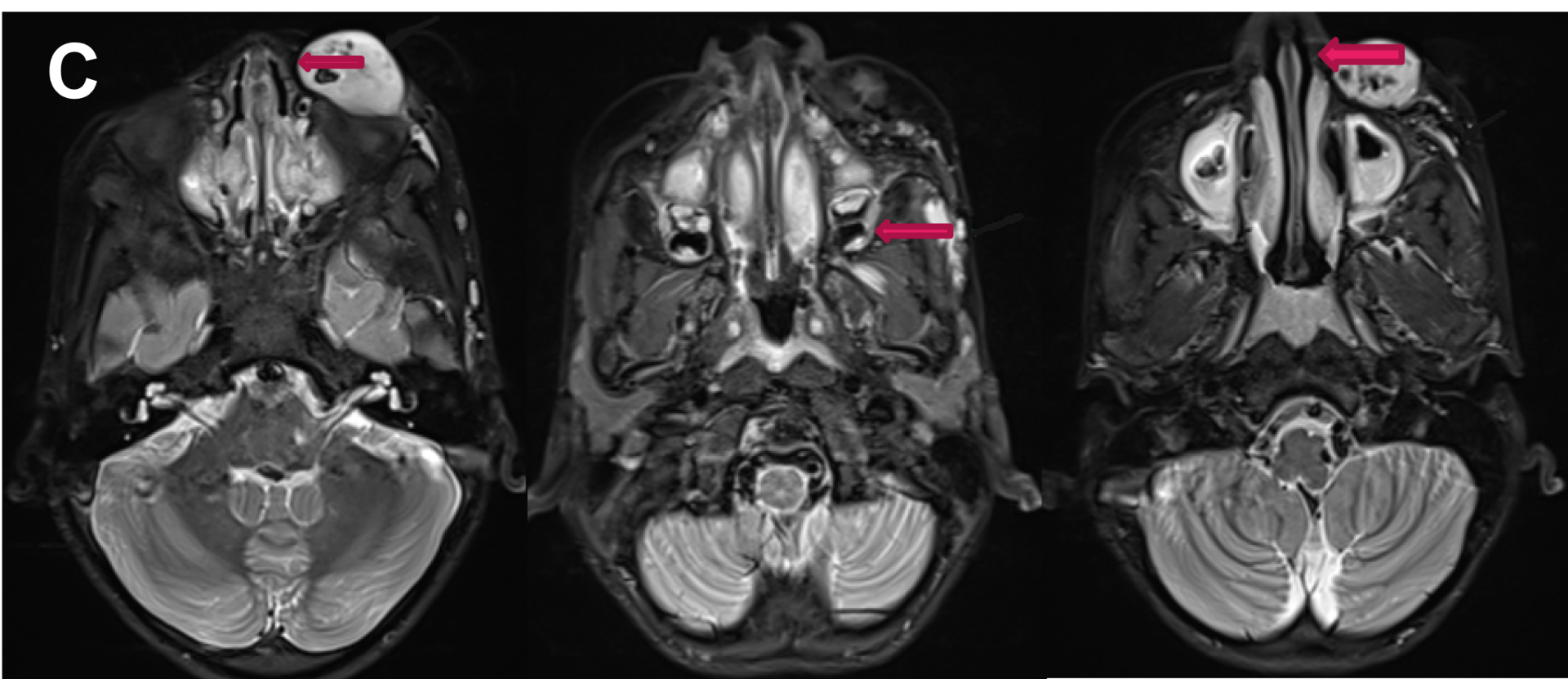
- C. STIR sequences showing similar signal intensity tubular foci superficial to left temporalis and masseter muscles with a T2 hyperintense tubular structure connecting these foci to the lesion in the infraorbital region.
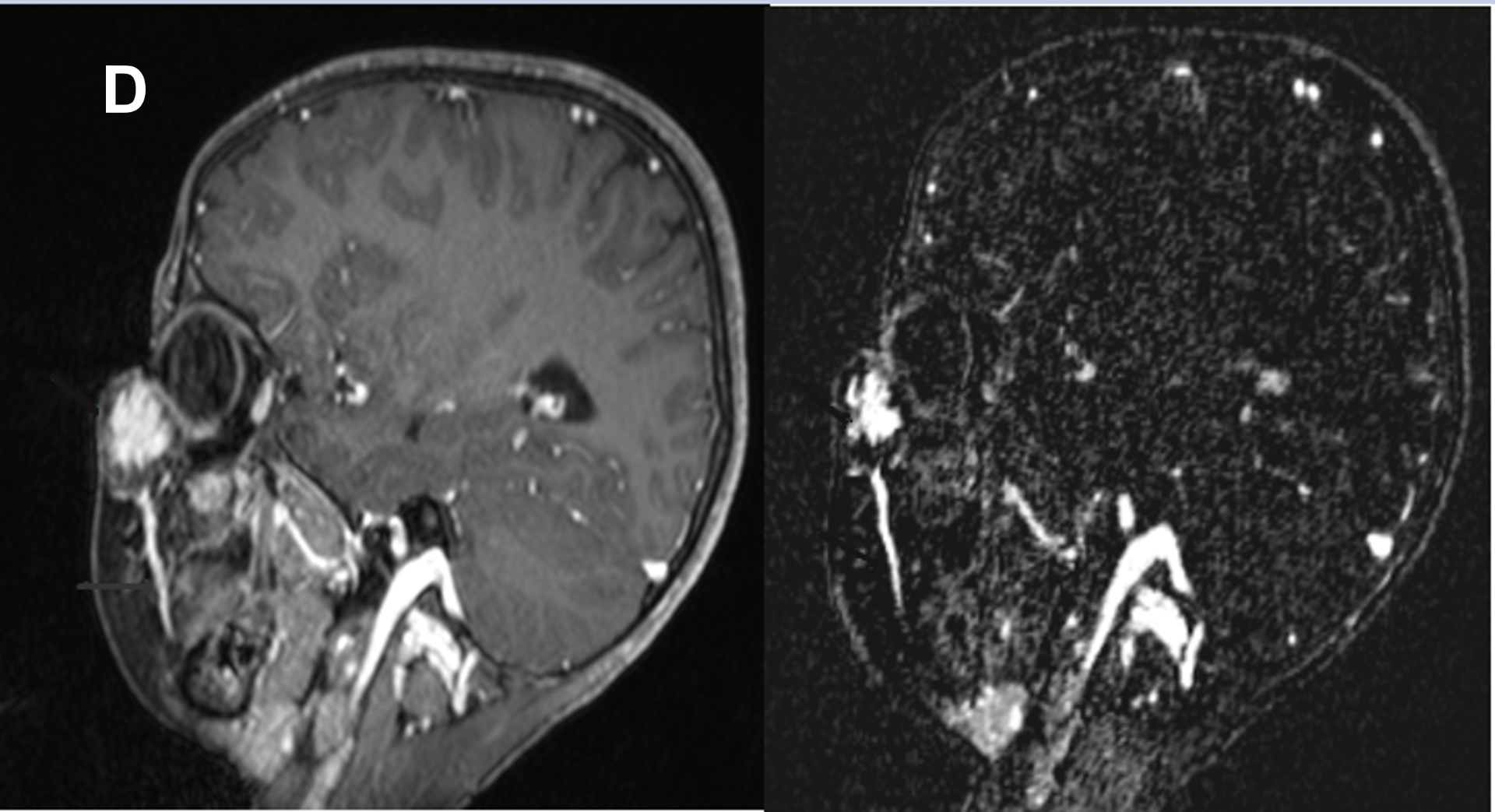
- D. Contrast enhanced and MR angiographic images reveals homogeneous contrast enhancement and the lesion draining into left facial vein which in turn draining into internal jugular vein.
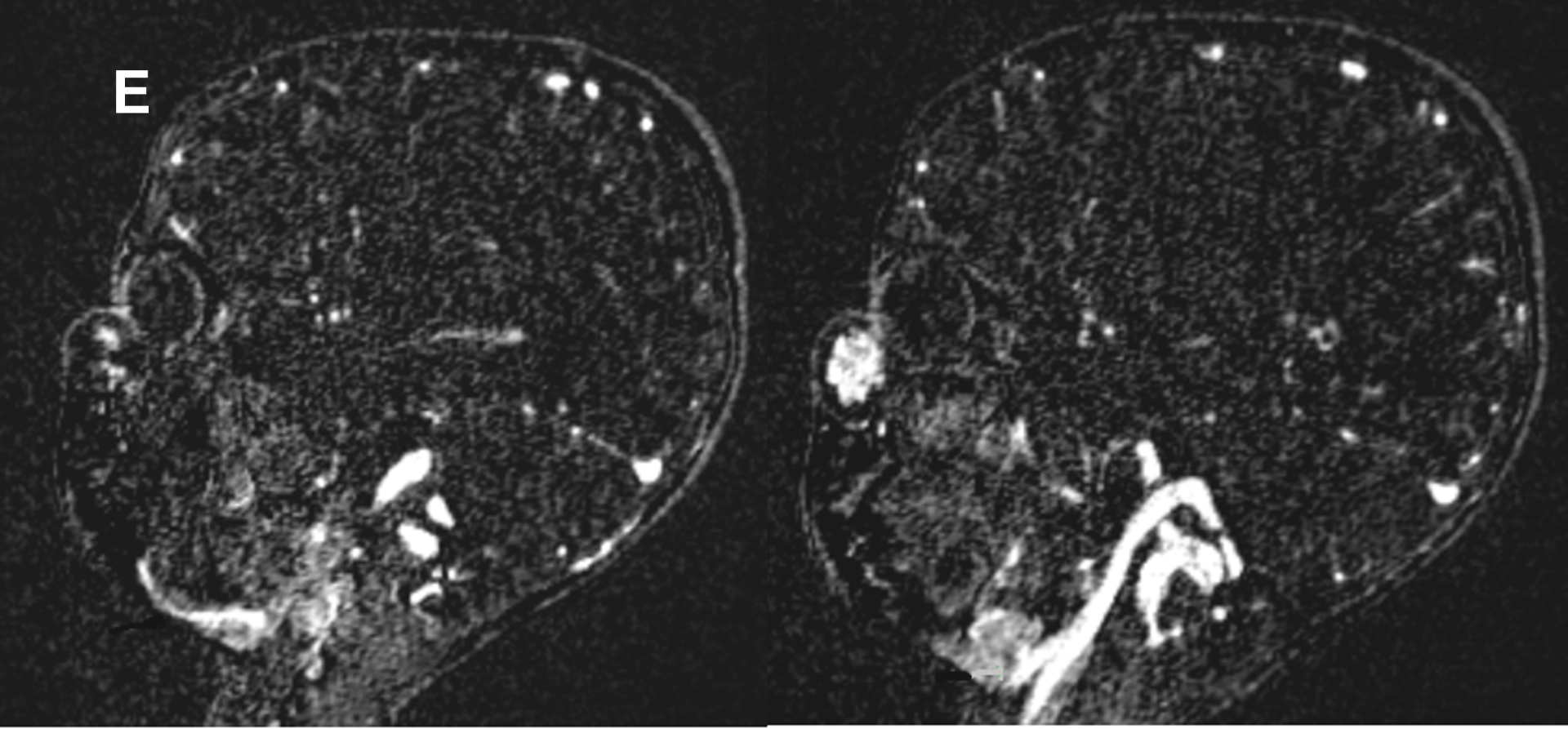
- E. No features of arterial feeders.
RADIOLOGICAL DIAGNOSIS
- A well defined T1 isointense, T2 hyperintense lesion with internal T1/T2 hypointense foci (Phleboliths) in the left infraorbital region.
- The lesion shows contrast enhancement. No features of diffusion restriction.
- A prominent vessels noted draining the lesion into left facial vein.
- No dilated or prominent arterial feeders.
- Few similar T2 hyperintense tubular foci (vascular loops) noted superficial to left temporalis and masseter muscles.
- There is vascular channel noted connecting these foci to lesion in the infraorbital region.
- No features of communication into cerebral venous plexus. No cavernous sinus thrombosis.
Imaging features suggestive of low flow venous malformation in left infraorbital region with drainage into left facial vein and few similar intercommunicating venous malformations superficial to left temporalis and masseter muscle.
DISCUSSION
- Venous malformations (VMs) are congenital endothelial malformations that result from errors in vascular morphogenesis.
- Composed of vascular channels sometimes containing intraluminal thrombus, are lined by thin endothelium.
- It is subtype of low flow vascular malformations.
- They are usually present at birth but are not always apparent and grow in proportion to the child's growth until puberty.
Clinical presentation
- Located superficially within the head and neck (40%), trunk (20%), or limbs (40%) and can also be found in the viscera
- Presenting complaints include cosmetic, swelling from dependent stasis, pain from localized thrombosis, or limitation of activities and even altered limb growth
- Usually presents as nonpulsatile, compressible, discrete soft-tissue mass that causes no alteration in skin temperature, thrill, or bruit
- Increase in size and coloration during a Valsalva maneuver, with dependent positioning, and sometimes with the application of a tourniquet
- If the skin is involved, a blue-purple hue or superficial veins can be seen.
- Sudden enlargement can happen after trauma, intralesional thrombosis, puberty, pregnancy, and oral contraceptive intake.
- Elevated level of d-dimers can be seen secondary to thrombosis.
- It has a variable appearance at presentation ranging from solitary to multiple, small circumscribed to extensive infiltrative lesion crossing multiple tissue planes.
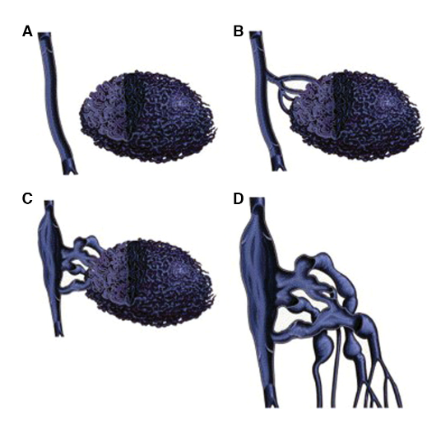
- Three main venographic patterns—cavitary, spongiform, and dysmorphic
- Dubois et al. and Puig et al. further subdivided these patterns into the following four types based on patterns of venous drainage
- A- type I,isolated malformations without venous drainage;
- B- type II, malformations that drain into normal veins;
- C- type III, malformations that drain into dysplastic veins
- D- type IV, malformations consisting primarily of venous ectasia
US:
- Ultrasound with colour Doppler is the first line imaging to diagnose low flow venous malformation.
- Superficial venous malformations are compressible with heterogeneous echotexture (98%) and can be hypoechoic (82% ), hyperechoic (10%) or isoechoic (8% ).
- Calcified phleboliths are seen only in 16% of the cases.
- Tubular anechoic structures indicative of vascular channels are seen in 4% of cases.
- On colour Doppler monophasic flow typical for venous channels.
- About 16% of the cases very low flow below the detectable limits or thrombosis can cause a diagnostic confusion.
MR:
- Hypointense to isointense on T1
- Intralesional fat or thrombi appears hyperintense on T1, and phleboliths appears scattered punctate T1 low-signal intensity.
- T2- markedly hyperintense, Areas of low signal represents thrombosis or phleboliths
- Fat saturation sequences useful for determining lesion extent
- Gradient-echo sequences demonstrates hemosiderin and calcification
- May have fluid-fluid levels representing layering hemorrhage
- Circulatory portions of VMs have a wide range of contrast enhancement - homogeneous to heterogeneous, faint to vivid, and rapid to delayed
Diagnostic difficulties
Intravascular papillary endothelial hyperplasia:
- Venous malformations are prone to stasis because of the low flow which leads to clot formation.
- This intraluminal clot well late to formation of exuberant intralesional intraluminal capillary ingrowth, also known as intravascular papillary endothelial hyperplasia or Masson tumor
- On imaging these will have variation in proportions of internal solid components and septa and low-flow vascular channels result in variable amounts of vascular flow at Doppler imaging and no reliable intensity, homogeneity, or contrast-enhancement which can be confused with neoplasms
Purely intramuscular vascular malformations
- Purely intramuscular vascular malformations will have late presentation because of the decreased intralesional venous stasis secondary to muscle contraction.
- Increased risk of local intravascular coagulation and thrombosis leads to higher morbidity
- Higher rate of pain as the presenting symptom and cause greater limitation of physical activity which can be confused clinically with soft-tissue neoplasms
- Well defined, oval, or round and often are adherent to neurovascular bundles will mimic peripheral nerve sheath tumors and soft-tissue sarcomas
- Few intramuscular vascular malformations have higher rates of calcification then their non-intramuscular counterparts.
Reference
Low-Flow Vascular Malformation Pitfalls: From Clinical Examination to Practical Imaging Evaluation- Brandon Olivieri, et al- AJR article
Dr Harsha Chadaga
Senior Consultant and Head of Radiology
Manipal Hospital, Yeshwanthpur Bengaluru
Dr. Dhinesh kumar T
Radiology resident
Manipal hospital, Yeshwanthpur, Bengaluru.