A 67-year gentleman presents with triple-vessel disease. Echocardiography at outside facility revealed enlarged left ventricle with LVEF 45% and regional wall motion abnormality
A 67-year gentleman presents with triple-vessel disease. Echocardiography at outside facility revealed enlarged left ventricle with LVEF 45% and regional wall motion abnormality
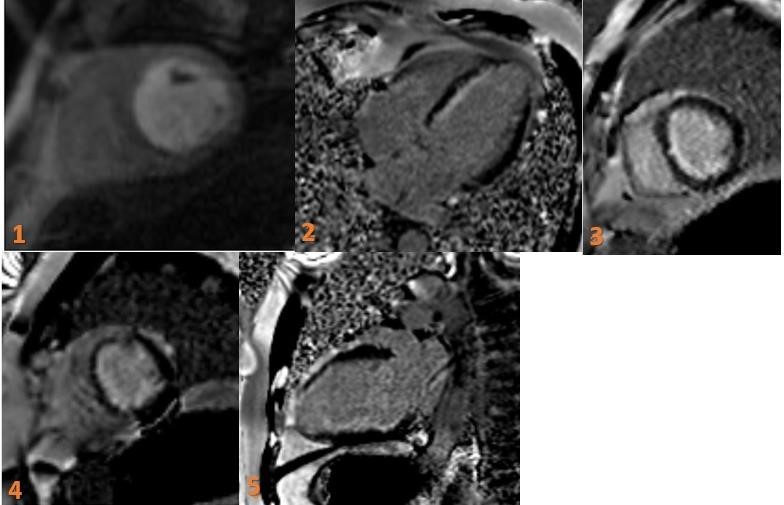
Fig 1. Short axis Rest perfusion defect involving Left ventricular (LV) subendocardial mid-ventricular and apical myocardium.
Fig 2. 4CH LV subendocardial (upto 25%) basal and mid interventricular septal and apical delayed gadolinium enhancement.
Fig 3,4. SA mid ventricular LV subendocardial delayed gadolinium enhancement involving mid interventricular septal and apical delayed gadolinium enhancement. Patchy involvement of anterolateral (red arrow) and posteromedial (green arrow) papillary muscles – infarction.
Fig 5. 2CH LV subendocardial (upto 25%) basal, mid inferior wall delayed gadolinium enhancement.
DIAGNOSIS:
- Viable Left anterior descending artery territory infarction.
- Infarction of anterolateral and posterolateral papillary muscles.
- Viable infarction- involving PDA/RCA territory.
DISCUSSION:
Following terminologies need to be kept in mind:
- Stunned myocardium: Stunned myocardium refers to a state in which there is wall dysfunction but the perfusion (resting and stress) is normal.
- Myocardial ischemia: Myocardial ischemia refers to a state in which there is decreased perfusion of the myocardium when stressed (such as during exertion) but normal perfusion during rest (seen as reversible perfusion defect). These patients will significantly benefit from treatment.
- Hibernating myocardium: With hibernating myocardium, the myocardium shows decreased perfusion on both stress and resting phase (seen as a fixed defect) but the myocytes are viable and will benefit from revascularization.
- Myocardial infarction: In myocardial infarction, there is absent perfusion both when the heart is stressed and at rest (a fixed defect) and the myocytes are not viable. There will be no benefit from revascularization:
-
- If the myocardial damage is partial, subendocardial hyperenhancement can be seen on delayed-enhancement images
- If the ischemia continues, necrosis gradually progresses outward to involve the epicardium, with ensuing transmural delayed hyperenhancement.
- In accordance with the clinical definition, viability is deemed as a present when below 50% of the area of the affected segment is seen, and absent when greater than 50% which is assessed by delayed myocardial enhancement on post-contrast T1w images.
REFERENCES:
- Souto AL, Souto RM, Teixeira IC, Nacif MS. Myocardial viability on cardiac magnetic resonance. Arquivos brasileiros de cardiologia. 2017 May;108(5):458-69.
- Rajiah P, Desai MY, Kwon D, Flamm SD. MR imaging of myocardial infarction. Radiographics. 2013 Sep;33(5):1383-412.
Dr. Deepali Saxena,
DNB, Fellowship Cardiothoracic Imaging (USA)
Lead Cardiothoracic Imaging
Manipal Hospitals Radiology Group.
Unit coordinator, Whitefield
Dr. Vivek Jirankali,
MD
Senior resident and cross-sectional fellow
Manipal Hospitals Radiology Group.