A 54-year-old woman, post-cholecystectomy -10 days back, now came with complaints of abdominal pain and vomiting.
A 54-year-old woman, post-cholecystectomy -10 days back, now came with complaints of abdominal pain and vomiting.
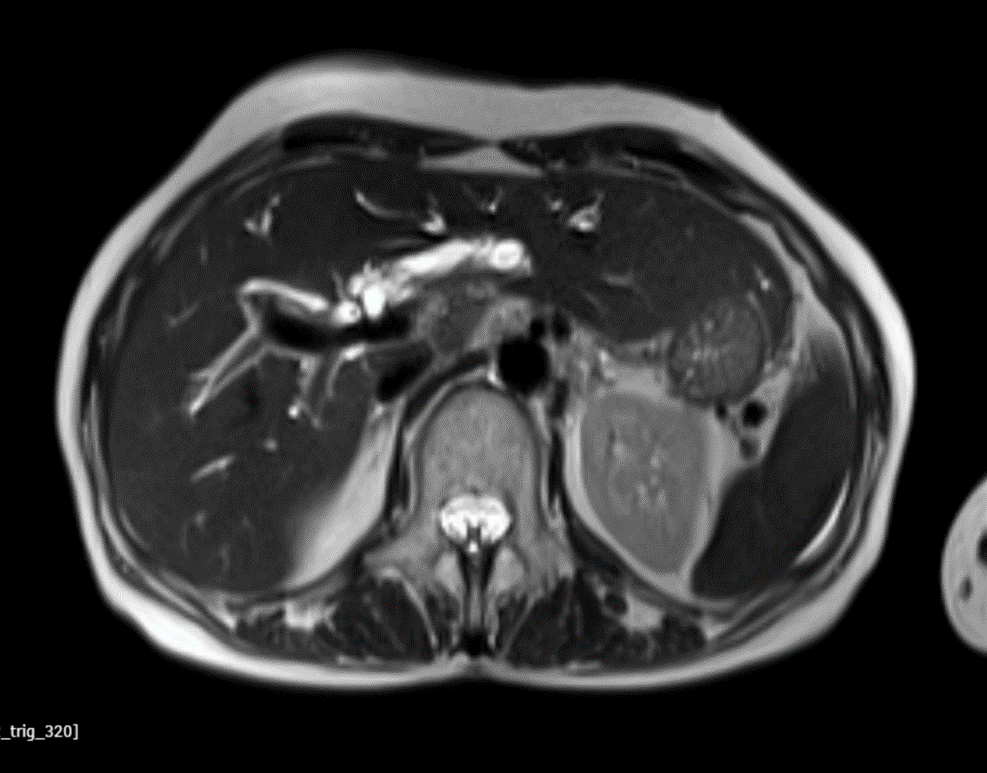
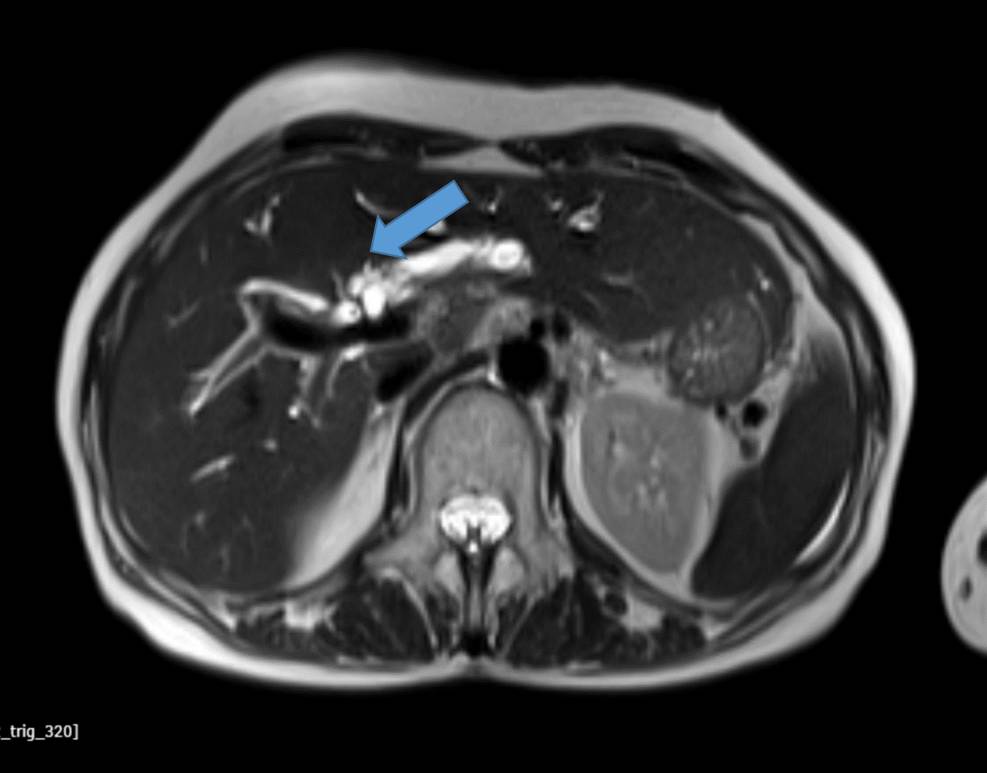
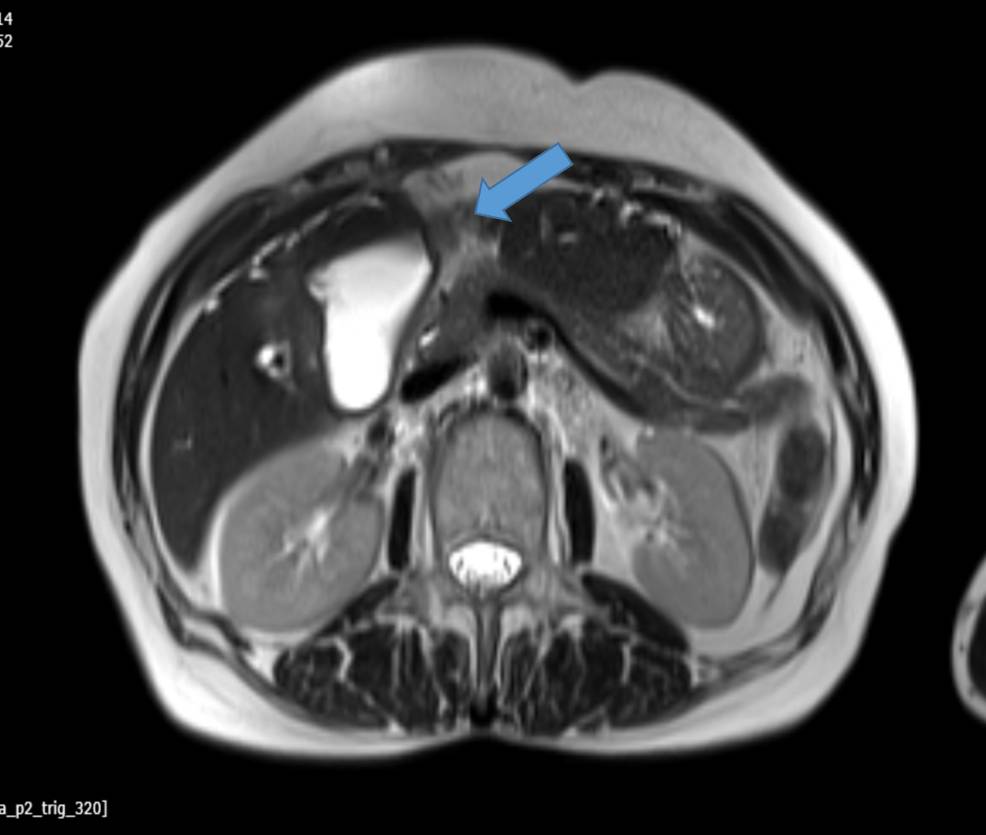
A: Postcholecystectomy status
T2WI shows a fluid collection in the gall bladder fossa with dilatation of bilobar intrahepatic biliary radicles
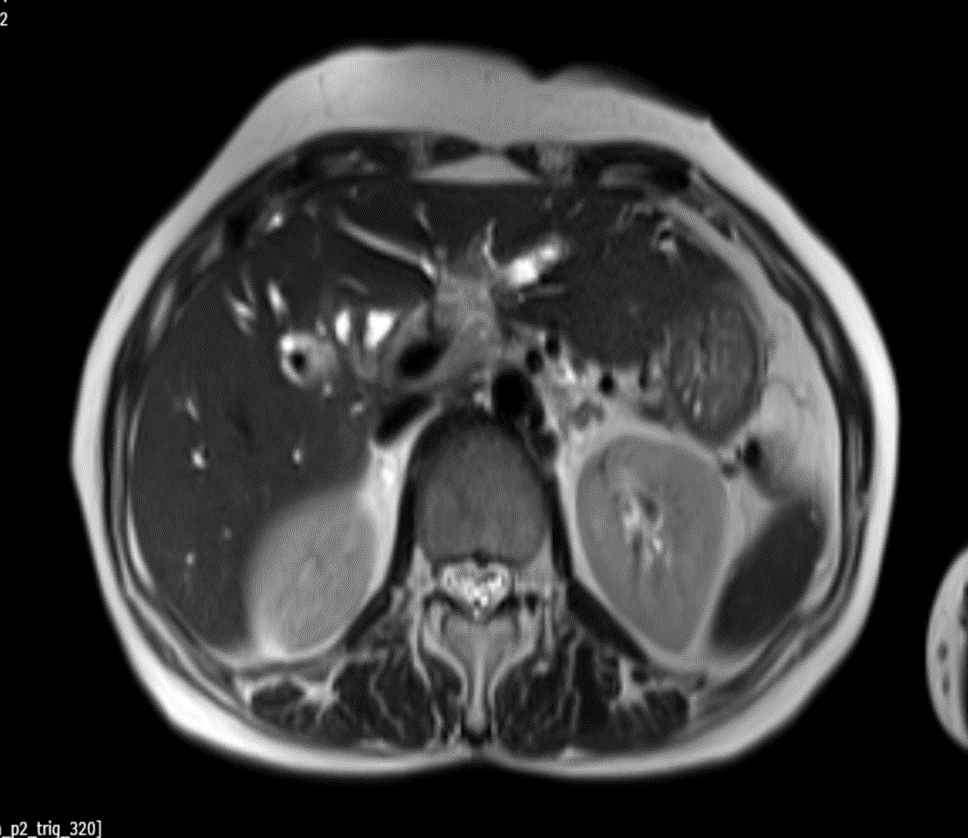
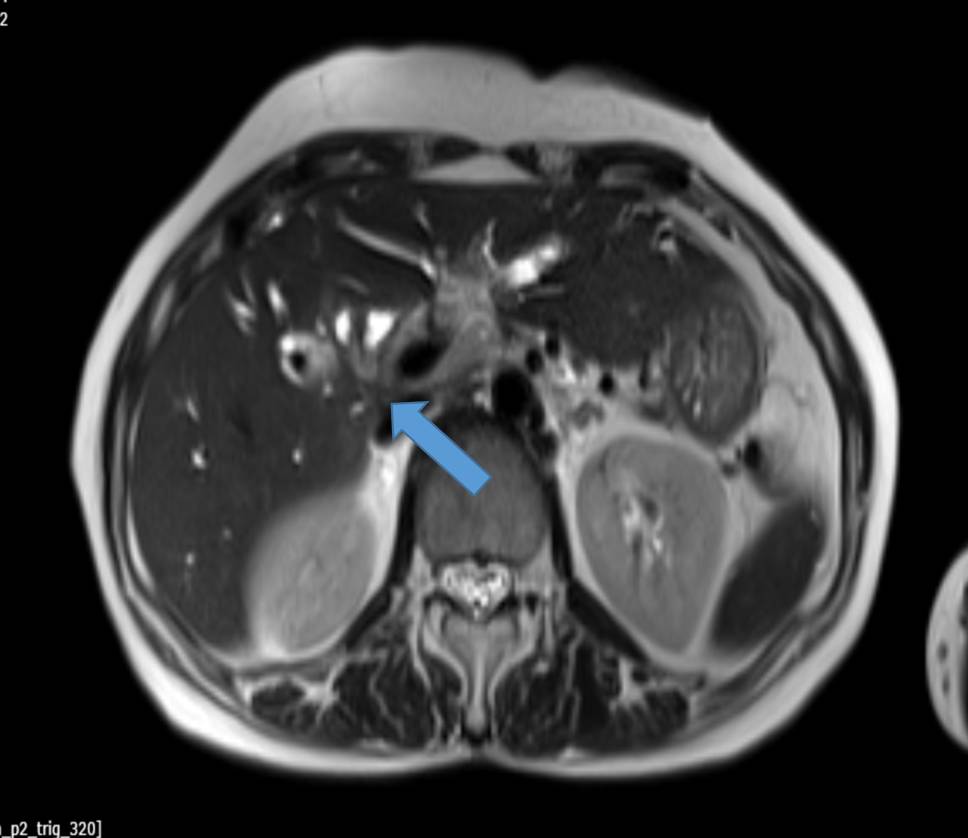
B.-T2WI shows narrowing noted involving the hepatic duct and primary biliary confluence for a length of 1.4 cm
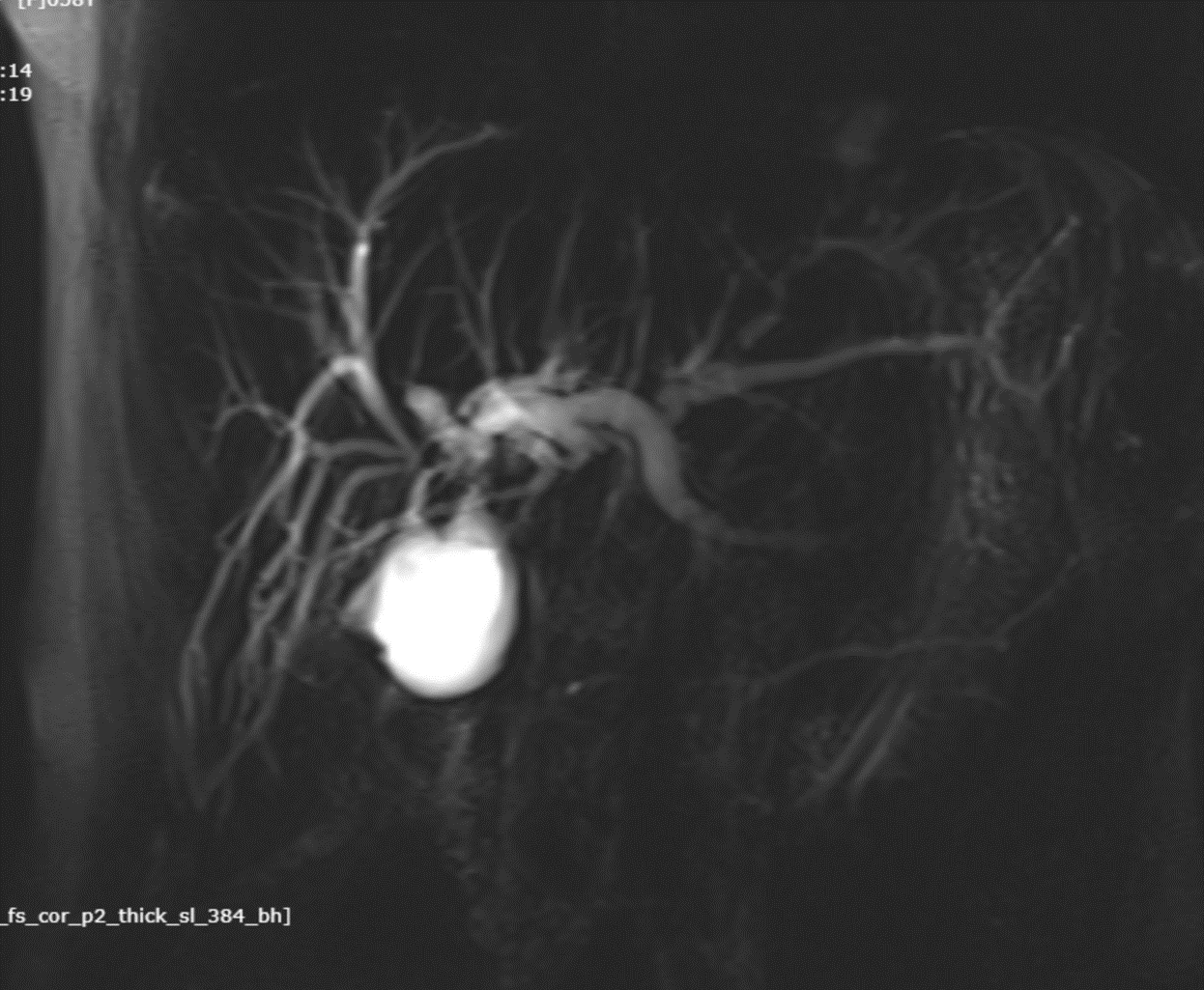
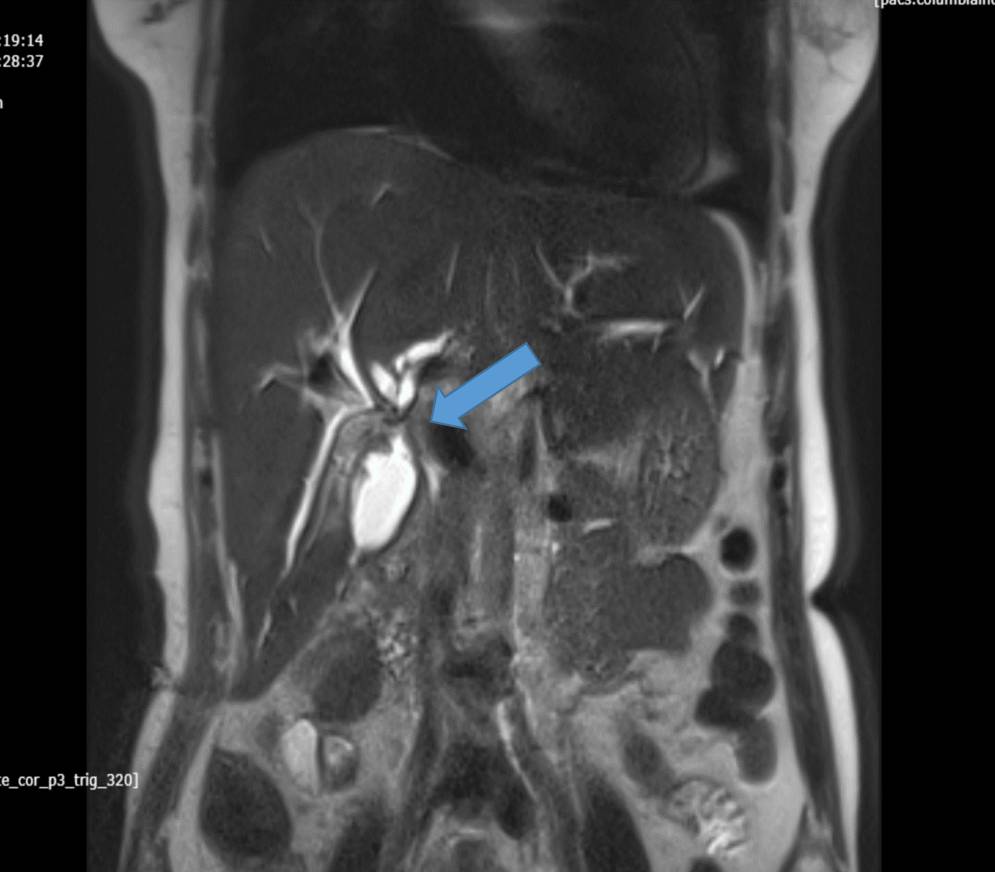
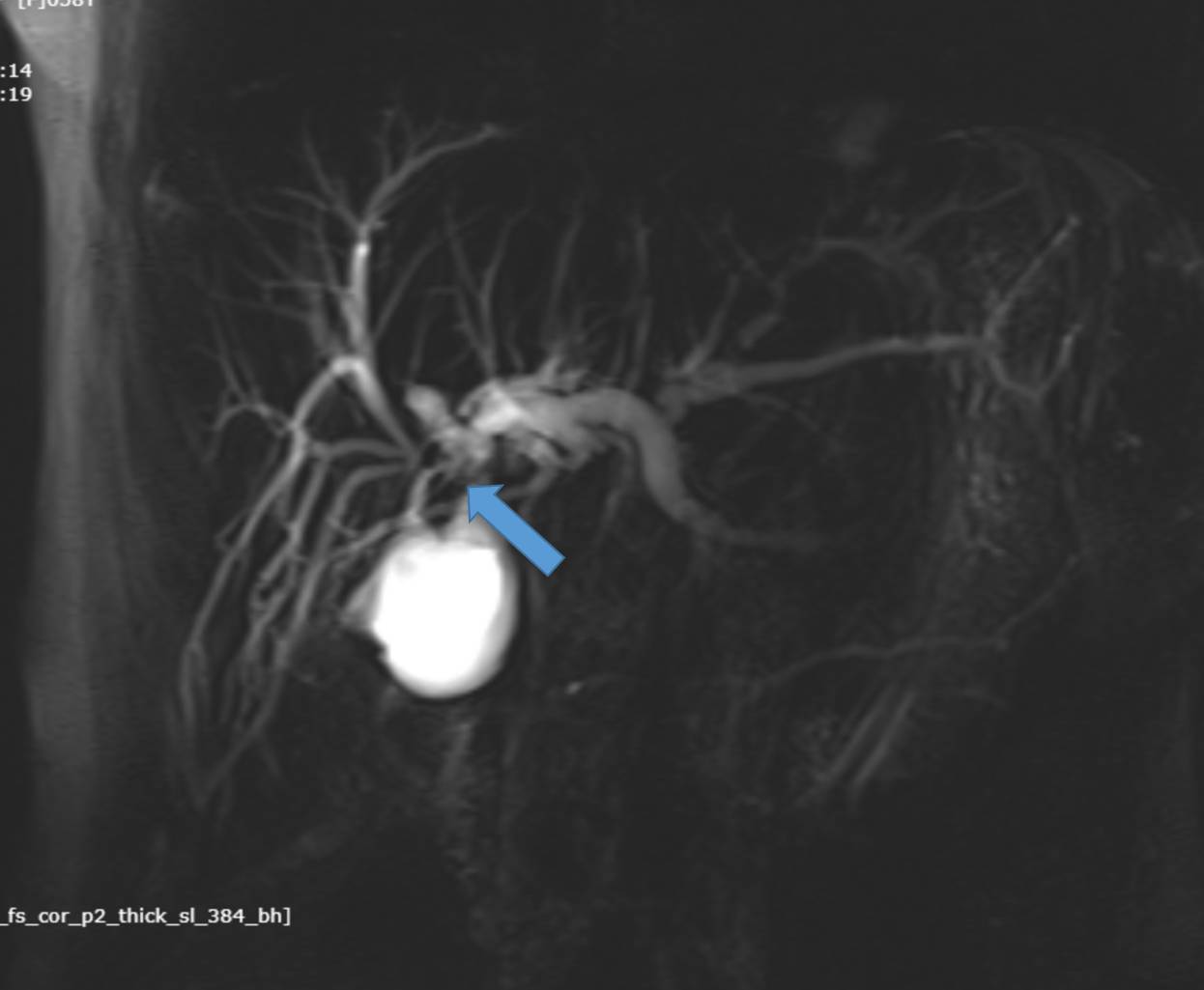
C.- MRCP shows a suspicious communication between the gall bladder fossa collection and left hepatic duct
Post operative Iatrogenic biliary duct injury with bile leak
(Strasberg classification – Type E- E4 )
Discussion:
- Iatrogenic bile duct injuries (IBDI) remain an important problem in gastrointestinal surgery.
- They are most frequently caused by laparoscopic cholecystectomy, which is one of the commonest surgical procedures in the world.
- The early and accurate diagnosis of IBDI is very important for surgeons and gastroenterologists, because unrecognized IBDI lead to serious complications such as biliary cirrhosis, hepatic failure and death
- IBDI present about 95% of all benign biliary strictures
Clinical presentation:
The common clinical symptoms are jaundice, fever, chills, and epigastric pain
Jaundice is observed in patients with stricture rather than bile leak
Diangnostic approach:
- Imaging diagnostics in IBDI involve ultrasonography of the abdominal cavity, cholangiography, endoscopic retrograde cholangiopancreatography (ERCP), computed tomography, and magnetic resonance-cholangiography.
- Magnetic resonance cholangiography is a sensitive (85%-100%) and non-invasive imaging modality for the biliary tract. Currently, it is the “gold standard” in preoperative diagnosis of IBDI in patients qualifying for surgical reconstruction
CLASSIFICATION OF IBDI:
- The Strasberg classification of bile duct injuryis a widely used system to anatomically define these injuries by location
Classification
- type A: injury to the cystic duct or from minor hepatic ducts draining the liver bed
- type B: occlusion of the biliary tree, commonly aberrant right hepatic duct(s)
- type C: transection without ligation of aberrant right hepatic duct(s)
- type D: lateral injury to a major bile duct
- type E: injury to the main hepatic duct; classified according to the level of injury
- E1 (Bismuth type 1): injury more than 2 cm from the confluence
- E2 (Bismuth type 2): injury less than 2 cm from the confluence
- E3 (Bismuth type 3): injury at the confluence; confluence intact
- E4 (Bismuth type 4): destruction of the biliary confluence
- E5 (Bismuth type 5): injury to the aberrant right hepatic duct
Surgical management:
Different surgical reconstructions are performed in patients with IBDI. According to the literature, Roux-en-Y hepaticojejunostomy is the most frequent surgical reconstruction and recommended by most authors. In the opinion of some authors, a more physiological and equally effective type of reconstruction is end-to-end ductal anastomosis.
Conclusion
- Iatrogenic bile duct injuries remain an important problem in gastrointestinal surgery.
- They are most frequently caused by laparoscopic cholecystectomy, which is one of the commonest surgical procedures in the world.
- Clinical symptoms like jaundice is observed in patients with stricture rather than bile leak
- The Strasberg classification of bile duct injuryis a widely used system to anatomically define these injuries by location
References
- Strasberg S, Strasberg HM, Strasberg SN, Strasberg. An Analysis of the Problem of Biliary Injury During Laparoscopic Cholecystectomy. (1995) Journal of the American College of Surgeons. doi:– Pubmed
- Bernhard W. Renz, Florian Bösch, Martin K. Angele. Bile Duct Injury after Cholecystectomy: Surgical Therapy. (2020) Visceral Medicine. 33 (3): 184. doi:10.1159/000471818– Pubmed
- Hariharan D, Hariharan PE, Hariharan SJ, Hariharan LD, Hariharan. Quality of Life and Medico-Legal Implications Following Iatrogenic Bile Duct Injuries. (2017) World journal of surgery. doi:10.1007/s00268-016-3677-9– Pubmed
- Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001;234:549–558; discussion 558-559. [PMC free article] [PubMed] [Google Scholar]
- Negi SS, Sakhuja P, Malhotra V, Chaudhary A. Factors predicting advanced hepatic fibrosis in patients with postcholecystectomy bile duct strictures. Arch Surg. 2004;139:299–303. [PubMed] [Google Scholar]
- Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture. Patterns of recurrence and outcome of surgical therapy. Am J Surg. 1984;147:175–180. [PubMed] [Google Scholar]
Dr. JAISHILPA
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr. SHARNITHA JOHNSON
Senior Resident
Manipal Hospital, Yeshwanthpur, Bengaluru.