80-year-old female presenting with chest pain and shortness of breath.
History
80-year-old female presenting with chest pain and shortness of breath. Past history of coronary stenting.
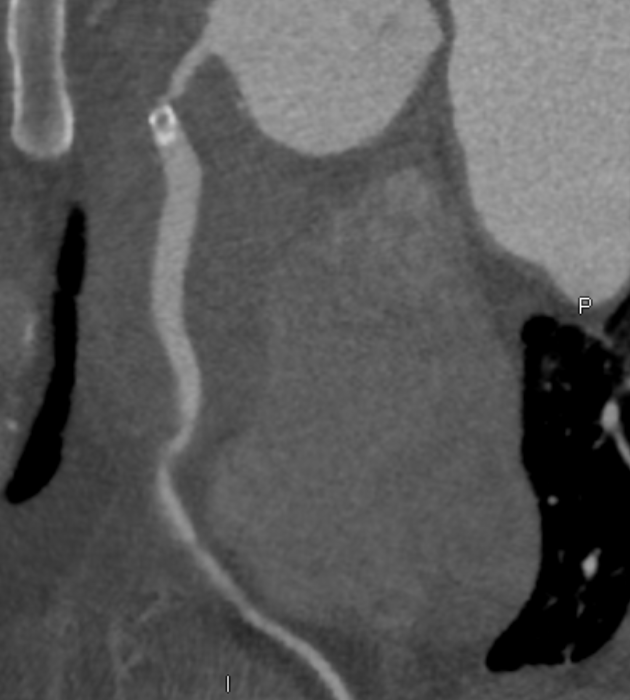
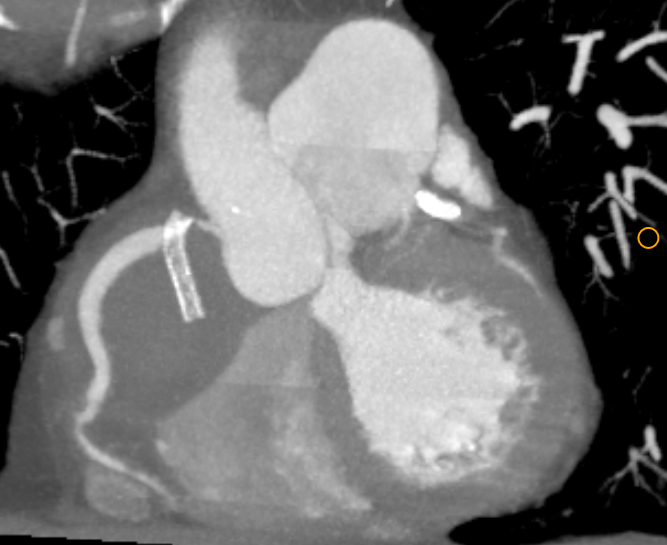
A. RCA stent (blue arrow) is extra-luminal in location with proximal tip in the proximal RCA and rest of the stent in the AV groove, no contrast opacification within the stent. Non enhancing soft tissue is seen around the extruded stent (asterix). No evident cardiac tamponade by soft tissue mass. Rest of the RCA shows normal opacification ( green arrow)
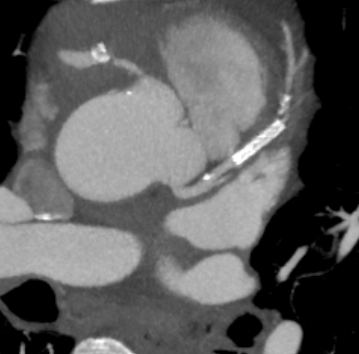
B. In-stent (orange arrow) and distal stent re-stenosis in mid LAD with 50-69% maximal stenosis (just distal to the stent, blue arrow) with good opacification of rest of the distal LAD.
DIAGNOSIS:
Coronary artery stent complication
- Extruded RCA stent into epicardial space with an inflammatory mass/granulation tissue around.
- Focal In-stent and distal stent re-stenosis in LAD
Complications of Percutaneous Coronary Interventions:
- Restenosis
- Stent Thrombosis
- Stent Deployment Failure
- Stent Fracture
- Coronary Artery Dissection
- Coronary Perforation or Rupture
- Stent Embolism or Migration
- Reperfusion Injury
DISCUSSION:
- CT is the mostly commonly used noninvasive imaging modality for evaluation of complications of coronary artery intervention.
- Restenosis is reduction in luminal diameter after PCI and is caused by either neointimal hyperplasia or neoatherosclerosis.
- For optimal evaluation of stents, strategies such as higher tube voltage, increased spatial resolution, a sharp kernel, a wider window, and iterative reconstruction can be used.
- Restenosis is higher with bare-metal stents and with first-generation drug-eluting stents than it is with second-generation drug-eluting stents.
- Stent embolism or migration is a rare complication of PCI that is predominantly caused by balloon dislodgement during implantation. Migration of an already-deployed stent is even more rare.
- Localization of the coronary stent may be challenging at ICA because some of the stents are radiolucent.
- MRI may not allow direct visualization of the stent, but the loss of signal intensity, resulting in local alteration of the magnetic field, can be used to localize the stent on gradient-echo images.
- In our case, Cardiac MRI may be useful to assess the epicardial soft tissue around the extruded stent and differentiate it from hematoma.
Case from literature



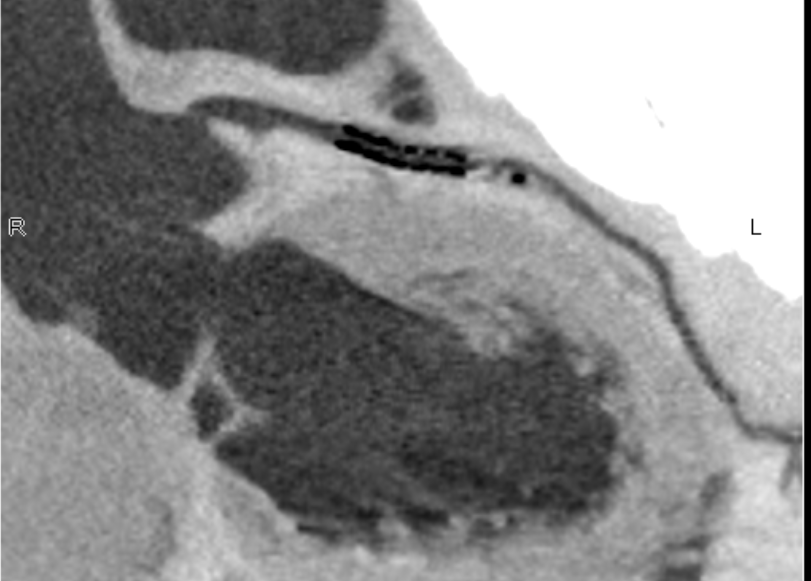
CT and MRI images showing (i) extruded right coronary artery stent with collection around it. (ii) right hypochondrial collection. (iii) fibrous tract extending from right ventricle
[From A typical presentation of extruded right coronary artery stent, S Subrahmanyam Adapa S, Karthikeyan Ranjith B, Kodali Rajesh, Sambandham Kamalkkannan GYear: 2021 | Volume: 24 | Issue Number: 3 | Page: 369-371 to right hypochondrium]
REFERENCES
- Goerne H, de la Fuente D, Cabrera M, Chaturvedi A, Vargas D, Young PM, Saboo SS, Rajiah P. Imaging Features of Complications after Coronary Interventions and Surgical Procedures. RadioGraphics. 2021 May;41(3):699-719.
- Andreini D, Pontone G, Mushtaq S, Bartorelli AL, Bertella E, Trabattoni D, Montorsi P, Galli S, Foti C, Annoni A, Bovis F. Coronary in-stent restenosis: assessment with CT coronary angiography. Radiology. 2012 Nov;265(2):410-7.
Dr Deepti H V
Consultant Radiologist
MHRG
Dr Vikas H P
Radiology resident
MHRG