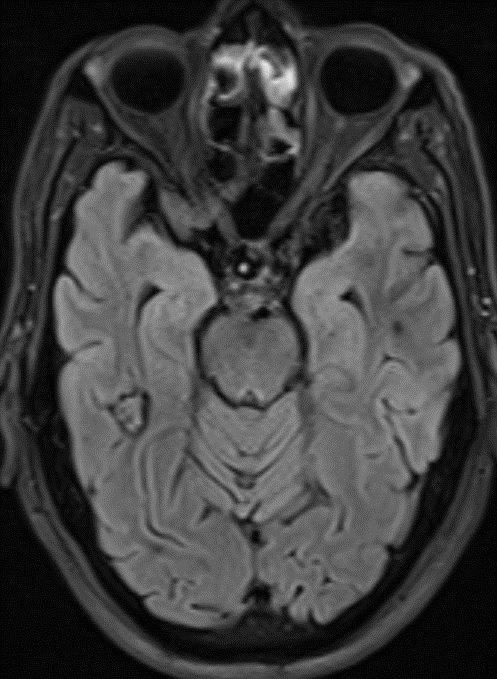
68 year old male, presenting with Chronic headache and giddiness.
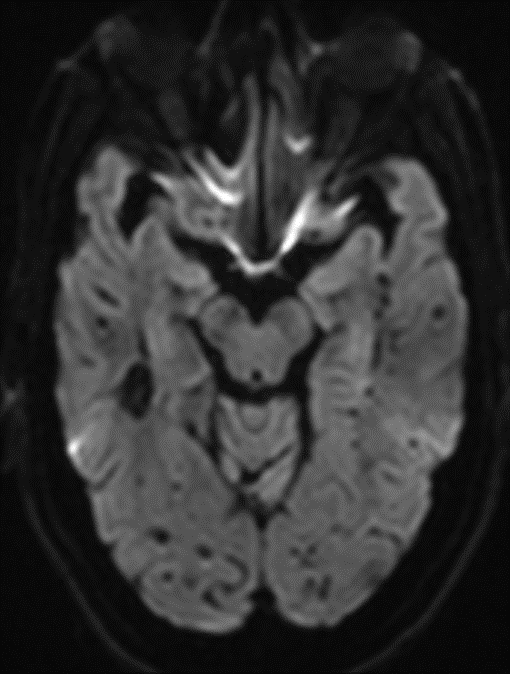
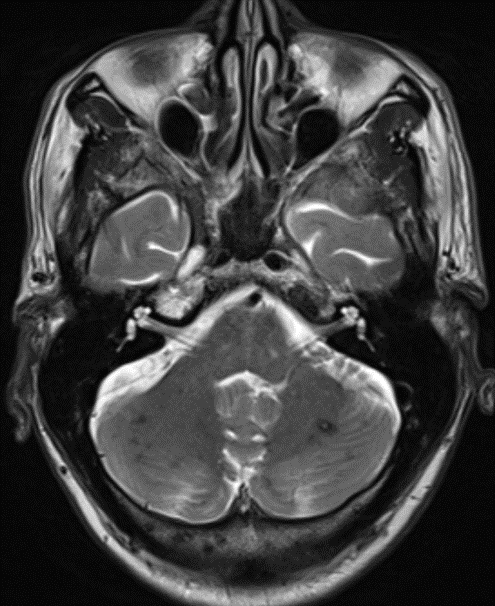
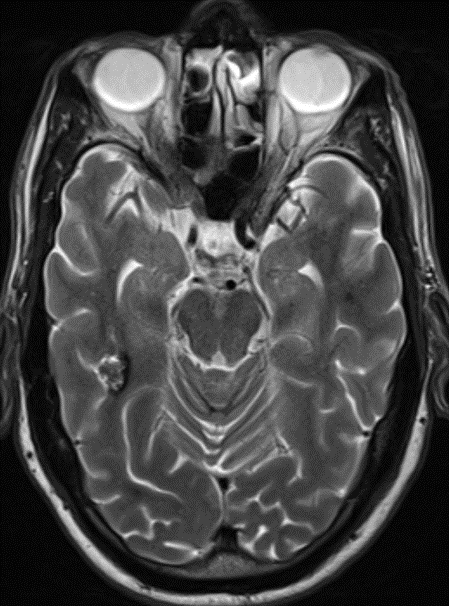
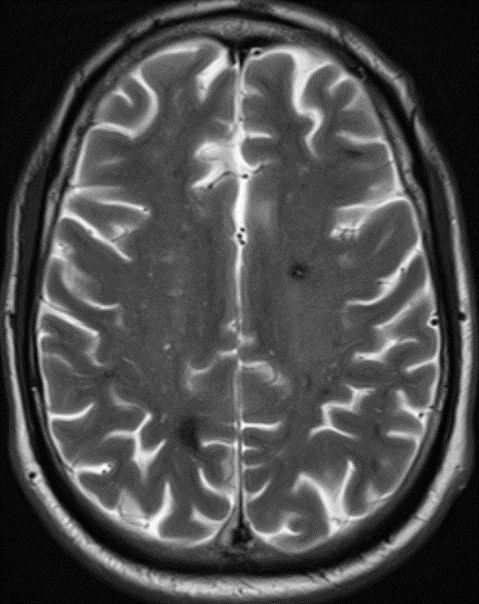
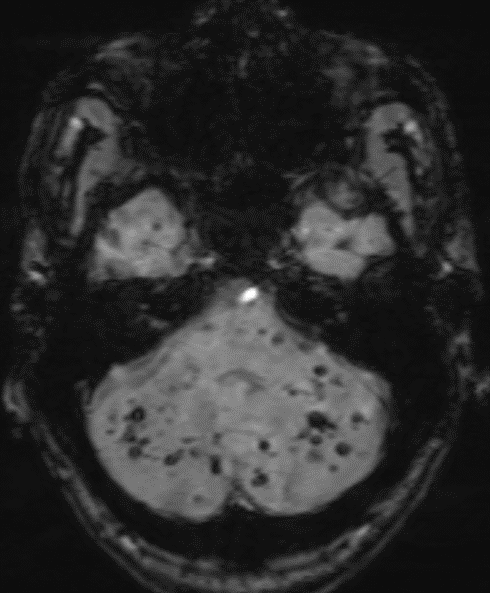
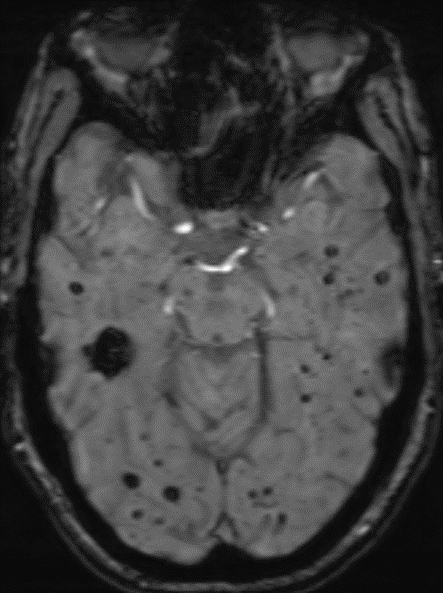
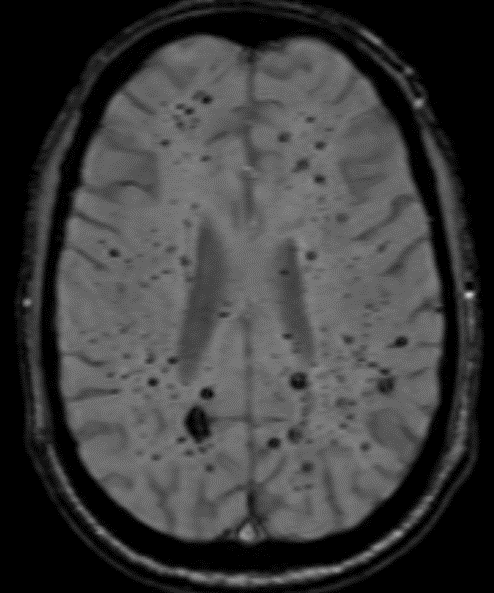
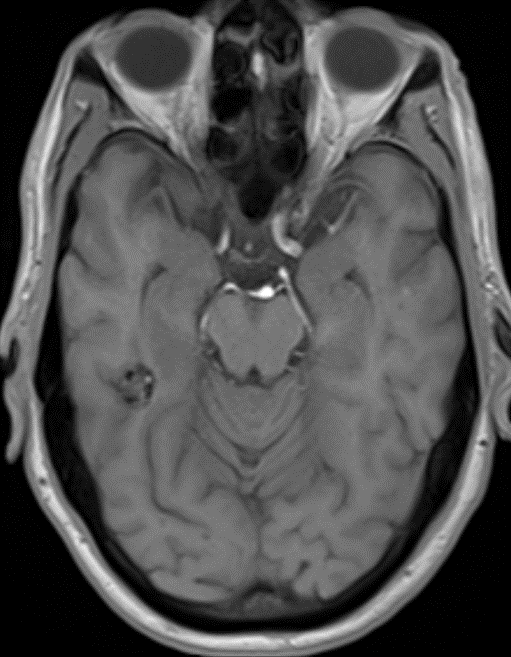
1. Multiple variable-sized lesions scattered in bilateral cerebral and cerebellar hemispheres, brainstem appearing mixed signal intensity lesions with the hypointense rim on T2 with and show blooming on SWI (suggestive of hemorrhage).
2. The lesion also shows hypo intense rim on T1W and FLAIR images with mixed signal intensity in the centre.
3. No diffusion restriction and no surrounding perilesional edema.
DIAGNOSIS:
Multiple Cavernomas.
DISCUSSION:
Cerebral cavernous venous malformations, also commonly known as cavernomas, are common cerebral vascular malformations.
ØIt is the third most common cerebral vascular malformation after developmental venous anomaly and capillary telangiectasia.
ØAccording to newer nomenclature (ISSVA classification of vascular anomalies) these lesions are now officially termed slow flow venous malformations.
Epidemiology:
- Most patients who present symptomatically do so at 40-60 years of age and are incidental findings on neuro-imaging
- Most commonly present with single lesion.
- Multiple lesions may be familial: Familial multiple cavernous malformation syndrome
- Cavernoma and capillary telangiectasias, are commonly seen following cerebral radiotherapy.
Clinical presentation:
- The majority of lesions remain asymptomatic throughout life and are found incidentally.
- Presentation due to hemorrhage may cause a headache, seizure or focal neurological deficit.
Pathology:
- Histologically cavernous malformations are composed of a “mulberry-like” cluster of hyalinized dilated thin-walled capillaries, with surrounding hemosiderin.
- These vessels are thrombosed to varying degrees.
- Unlike AVMs, there is no normal brain between the interstices of these lesions.
Associations:
- If associated with a developmental venous anomaly (DVA) they are known as a mixed vascular malformation.
Radiographic features
- Most commonly supratentorial (~80% cases).
- Usually solitary.
CT
- Difficult to see on CT.
- They do not enhance.
- If large they appear as a region of hyper density resembling blood products and speckles of calcification.
- If there has been a recent bleed then they may be surrounded by a mantle of edema.
MRI
MRI is the modality of choice, demonstrating a characteristic “popcorn” or “berry” appearance with a rim of signal loss due to hemosiderin.
Cavernous malformations can be grouped into four types based on MRI appearances using the Zabramski classification.
T1: Varied signal depending on the age of the blood products, small fluid-fluid levels may be evident
T2
- hypointense rim
- varied signal internally depending on the age of blood products
- blood locules with fluid-fluid levels may be seen
- if a recent bleed has occurred, surrounding edema may be present
GRE T2*/SWI
- prominent blooming
- useful for detecting smaller lesions
T1 C+ (Gd): No enhancement.
Angiography (DSA)
Do not demonstrate arteriovenous shunting.
DSA is useful to differentiate a cerebral cavernous malformation from an arteriovenous malformation.
Differential diagnosis
The differential, when cavernous malformations are numerous, is that of other causes of cerebral micro haemorrhages:
- Cerebral amyloid angiopathy: usually numerous small foci
- Chronic hypertensive encephalopathy: more common in the basal ganglia
- Diffuse axonal injury (DAI)
- Cerebral vasculitisHaemorrhagic metastases
Familial multiple cavernous malformation syndrome
Diagnostic criteria:
- Multiple cerebral cavernous malformations
1. five or more cavernomas, or
2. one cavernoma and at least one other family member with one or more cavernomas
- Mutations in one of the three genes, KRIT1, CCM2 or PDCD10, which are associated with this disease
REFERENCES
- Bergui M & Bradac G. Uncommon Symptomatic Cerebral Vascular Malformations. AJNR Am J Neuroradiol. 1997;18(4):779-83. PMC8338472 – Pubmed
- Blitstein M & Tung G. MRI of Cerebral Microhaemorrhages. AJR Am J Roentgenol. 2007;189(3):7205. doi:10.2214/ajr.07.2249
- Jain R, Robertson P, Gandhi D, Gujar S, Muraszko K, Gebarski S. Radiation-Induced Cavernomas of the Brain. AJNR Am J Neuroradiol. 2005;26(5):1158-62. PMC8158583 – Pubmed
- Brunereau L, Labauge P, Tournier-Lasserve E, Laberge S, Levy C, Houtteville J. Familial Form of Intracranial Cavernous Angioma: MR Imaging Findings in 51 Families. Radiology. 2000;214(1):20916. doi:10.1148/radiology.214.1.r00ja19209 – Pubmed
- Vilanova J, Barceló J, Smirniotopoulos J et al. Hemangioma from Head to Toe: MR Imaging with Pathologic Correlation. RadioGraphics. 2004;24(2):367-85. doi:10.1148/rg.242035079 – Pubmed
- Zhu W, Qi J, Zhan C et al. Magnetic Resonance Susceptibility Weighted Imaging in Detecting Intracranial Calcification and Hemorrhage. Chin Med J (Engl). 2008;121(20):2021-5. – Pubmed
- Pinker K, Stavrou I, Knosp E, Trattnig S. Are Cerebral Cavernomas Truly Nonenhancing Lesions and Thereby Distinguishable from Arteriovenous Malformations? Magnetic Resonance Imaging. 2006;24(5):6317. doi:10.1016/j.mri.2005.10.037 – Pubmed
Dr. Harsha Chadaga
Lead Neuroradiologist.
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.
Dr. Srinivas P
Fellow in Radiology
Manipal Hospital Radiology Group (MHRG)
Manipal Hospital, Bengaluru.