66-year-old with left side hearing loss
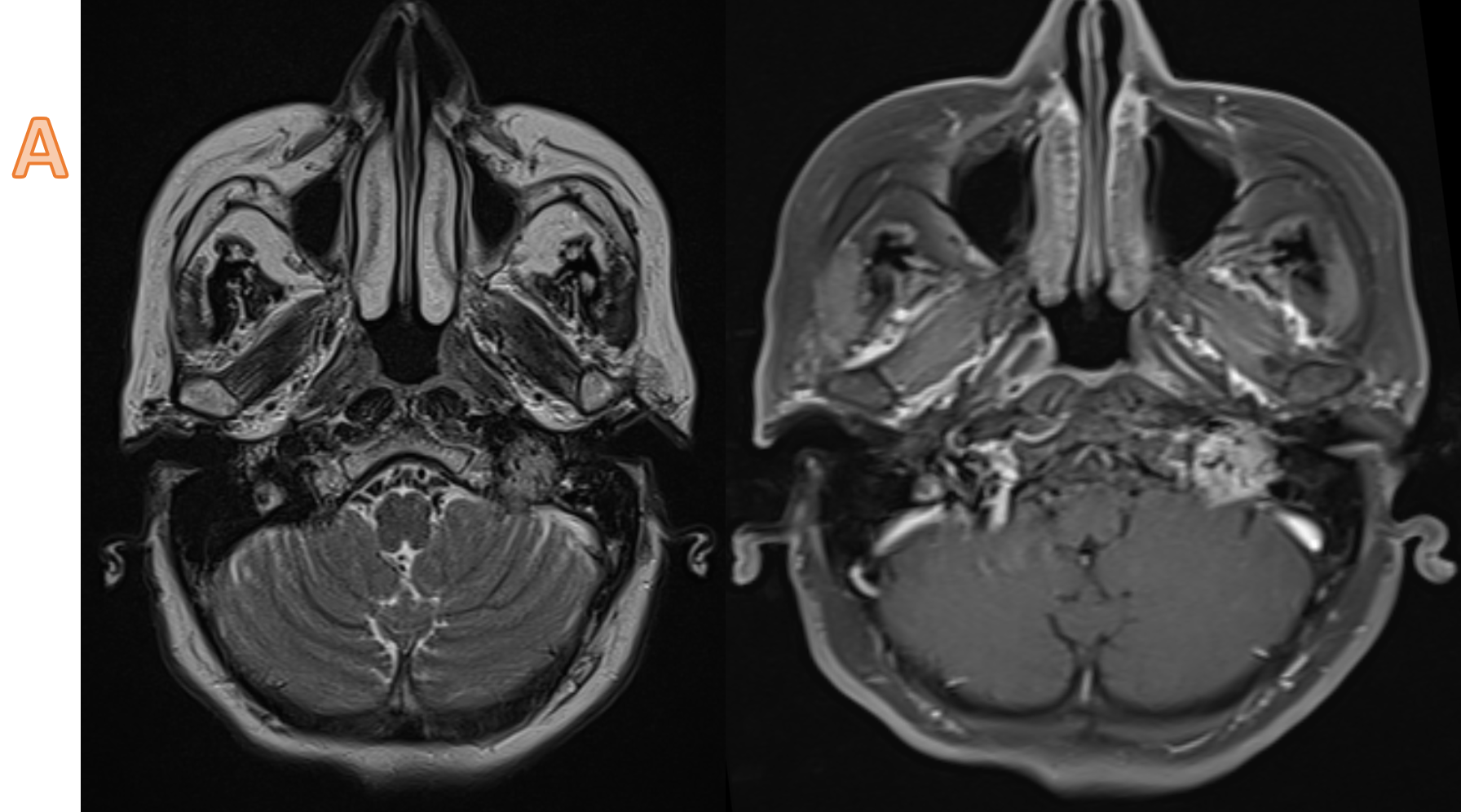
A. A well defined T2 heterogeneous signal intensity lesion centered in the left jugular foramen. The lesion enhances vividly and demonstrates multiple flow voids creating a salt and pepper appearance.
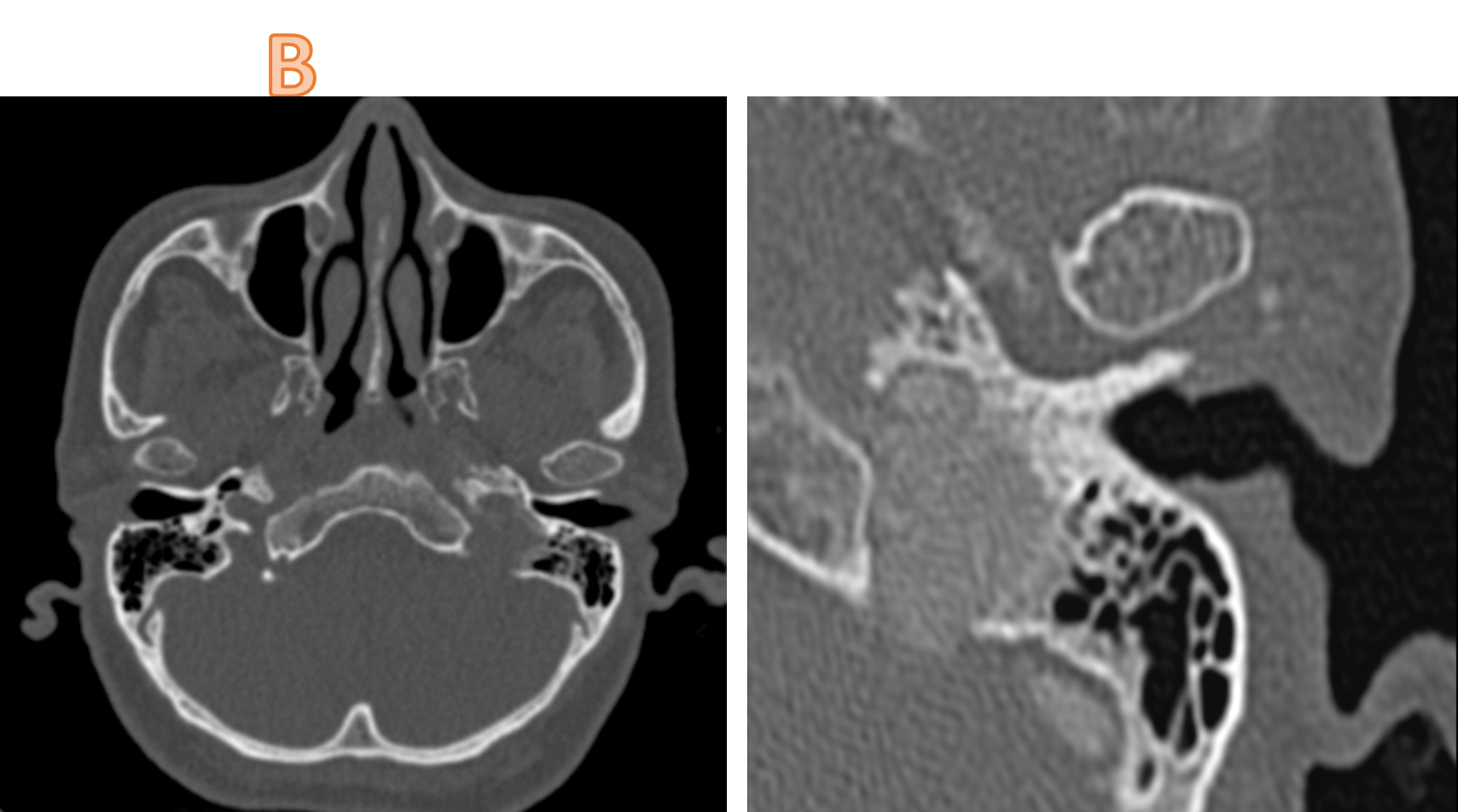
B. Circumferential expansion of the jugular foramen with bony destruction of jugular bulb. Erosion of the caroticojugular spine (between the carotid canal and jugular fossa) – Phelp sign (BLUE ARROW), normal carotico-jugular spine on the right (ORANGE ARROW). The lesion abuts and partially encases the cervical internal carotid artery, in adjoining short segment petrous carotid canal.
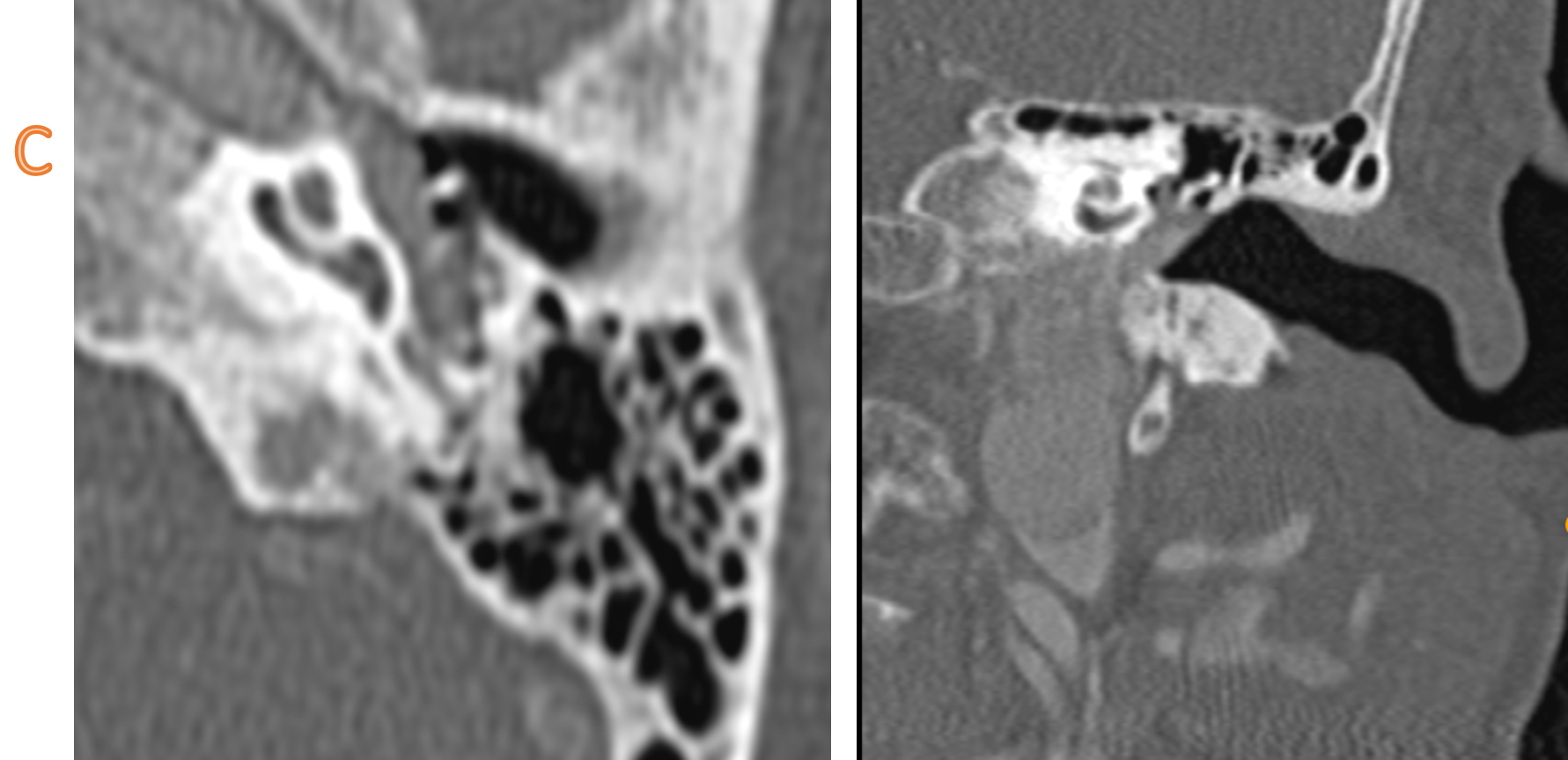
C. The enhancing lesion is seen extending to the hypotympanum and mesotympanum, with partial encasement of the ossicular chain.
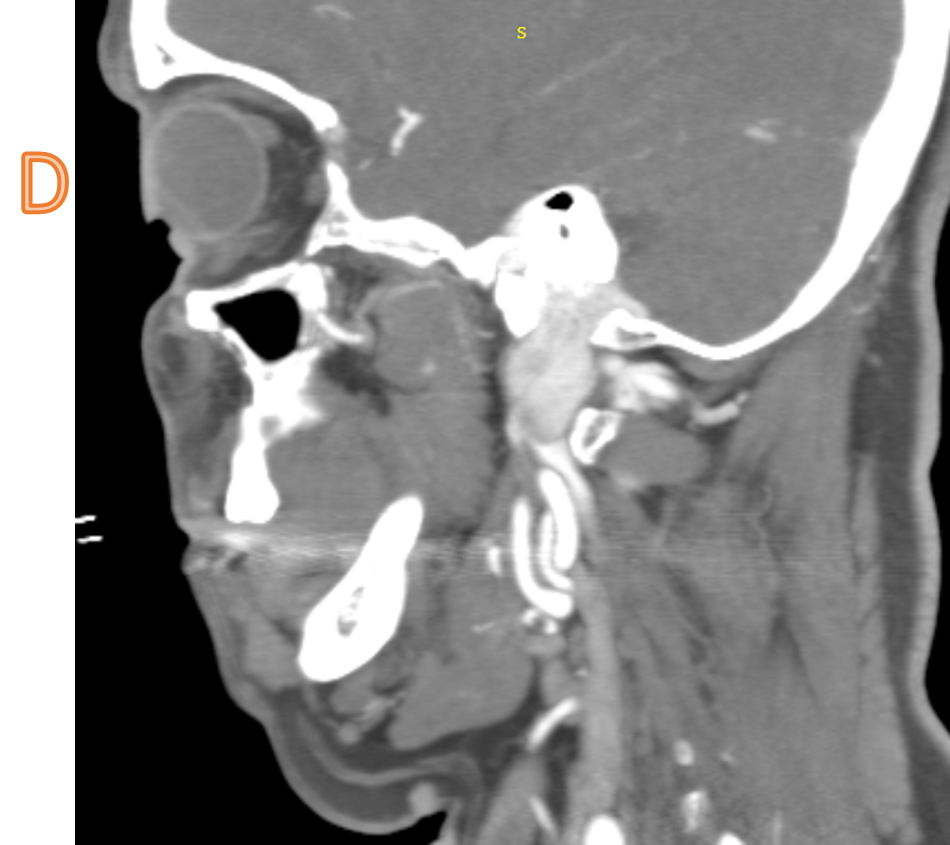
D. Hypertrophied left ascending pharyngeal artery. Early venous drainage (high density in left IJV on arterial phase).
DIAGNOSIS:
Glomus jugulare paraganglioma
DISCUSSION:
- Glomus jugulare paraganglioma is a paraganglioma of the head and neck that is confined to the jugular fossa.
- Presentation depends on the degree of middle ear involvement. When significant involvement is present then the lesion may cause pulsatile tinnitus and hearing loss. Additionally, a number of patterns of cranial nerve palsies have been described due to the involvement of the nerves at the jugular foramen.
- Growth of these tumors is in a number of directions, typically extending into the mastoid air-cells, middle ear, and Eustachian tube.
- CT is most useful at assessing the bony margins of the tumor, which are typically irregularly eroded with a moth-eaten pattern. Eventually, as the tumor enlarges the jugular spine is eroded and the mass extends into the middle ear, as well as inferiorly into the infratemporal fossa. CT is excellent at assessing the integrity of the ossicles and bony labyrinth. Also, erosion of the caroticojugular spine between the carotid canal and jugular fossa may be present (Phelp sign).
- Angiography demonstrates an intense tumor blush, with the most common feeding vessel being the ascending pharyngeal. Early draining veins are also noted due to intra-tumoral shunting.
- Angiography also has a role to play in preoperative embolization, which is typically carried out 1-2 days prior to surgery, however, care must be taken to fully evaluate feeding vessels. Familiarity with vascular anatomy of the region is essential if complications are to be avoided
- Glomus jugulare paraganglioma is a paraganglioma of the head and neck that is confined to the jugular fossa.
- Presentation depends on the degree of middle ear involvement. When significant involvement is present then the lesion may cause pulsatile tinnitus and hearing loss. Additionally, a number of patterns of cranial nerve palsies have been described due to the involvement of the nerves at the jugular foramen.
- Growth of these tumors is in a number of directions, typically extending into the mastoid air-cells, middle ear, and Eustachian tube.
- CT is most useful at assessing the bony margins of the tumor, which are typically irregularly eroded with a moth-eaten pattern. Eventually, as the tumor enlarges the jugular spine is eroded and the mass extends into the middle ear, as well as inferiorly into the infratemporal fossa. CT is excellent at assessing the integrity of the ossicles and bony labyrinth. Also, erosion of the caroticojugular spine between the carotid canal and jugular fossa may be present (Phelp sign).
- Angiography demonstrates an intense tumor blush, with the most common feeding vessel being the ascending pharyngeal. Early draining veins are also noted due to intra-tumoral shunting.
MRI
- T1: low signal 3
- T2: high signal
- T1 C+ (Gd): marked intense enhancement 2-4
- Salt and pepper appearance is seen on both T1 and T2 weighted sequences; the salt representing blood products from hemorrhage or slow flow and the pepper representing flow voids due to high vascularity.
Treatment and prognosis
Surgery is the treatment of choice and if complete resection is achieved a cure can be expected. Complications are however not uncommon due to a large number of sensitive structures in the region and include:
- cranial nerve deficits
- CSF/endolymphatic leak
Differentials:
-
- Jugular schwannoma:
- Sharply demarcated smooth bony margins.
- No internal flow voids
- Not very vascular on angiography
- No salt and pepper appearance.
- Bony metastases
- Hypervascular tumors may be very similar in appearances (e.g. renal cell carcinoma, thyroid cancer)
- Meningioma
- Jugular schwannoma:
References:
- . Eldevik OP, Gabrielsen TO, Jacobsen EA. Imaging findings in schwannomas of the jugular foramen. AJNR Am J Neuroradiol. 21 (6): 1139-44. AJNR Am J Neuroradiol (full text)2. Vogl T, Brüning R, Schedel H et-al. Paragangliomas of the jugular bulb and carotid body: MR imaging with short sequences and Gd-DTPA enhancement. AJR Am J Roentgenol. 1989;153 (3): 583-7. AJR Am J Roentgenol.3. Rao AB, Koeller KK, Adair CF. From the archives of the AFIP. Paragangliomas of the head and neck: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 19 (6): 1605-32. Radiographics (full text)
4. Head and neck imaging. Ed. by Peter M. Som, Hugh D. Curtin. St Louis (Mo.): Mosby-Year Book, 2003.
Dr Soham Naik
DNB Resident
Manipal hospital, Yeshwanthpur
DNB resident
Manipal Hospital, Yeshwanthpur