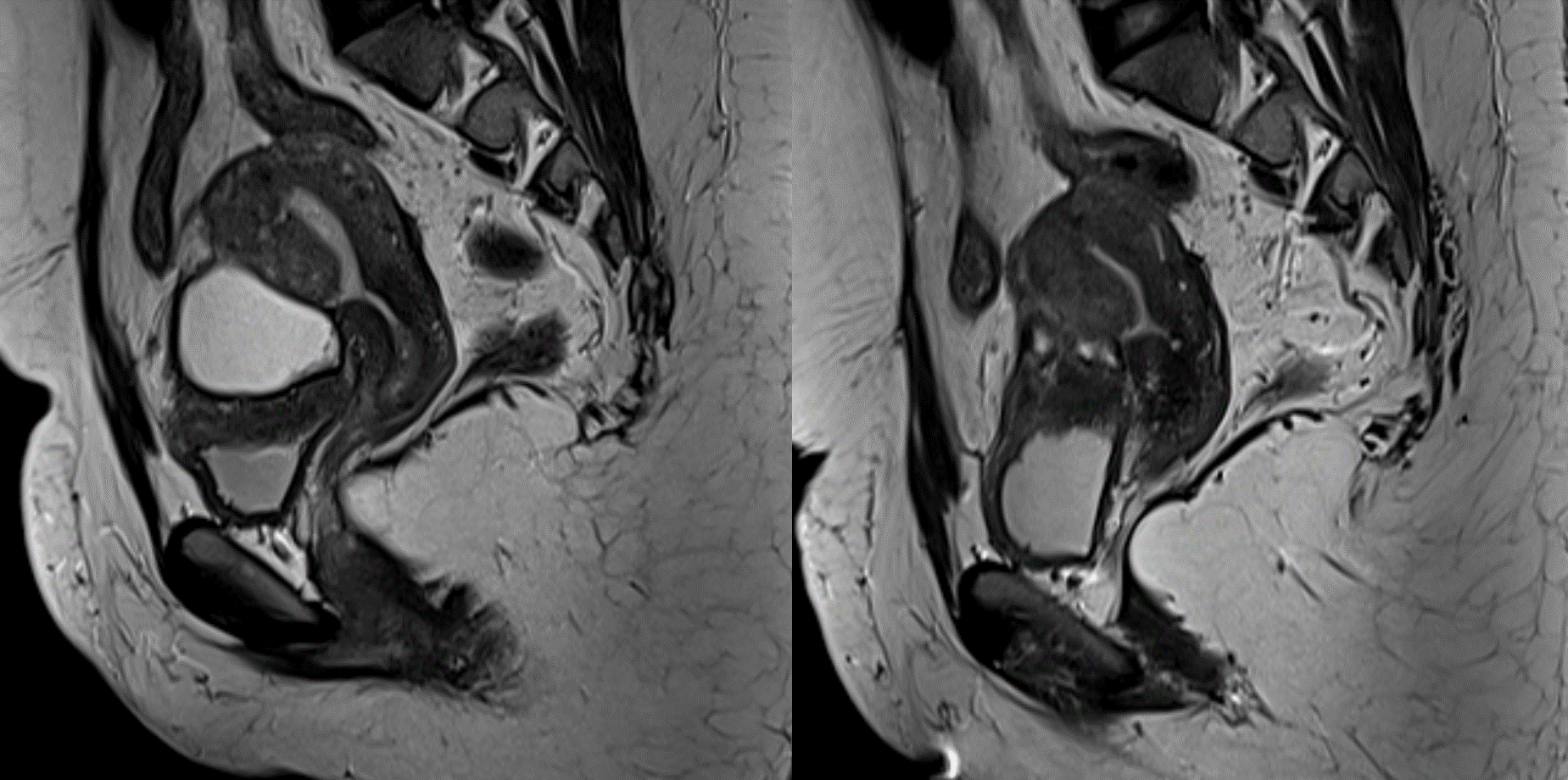
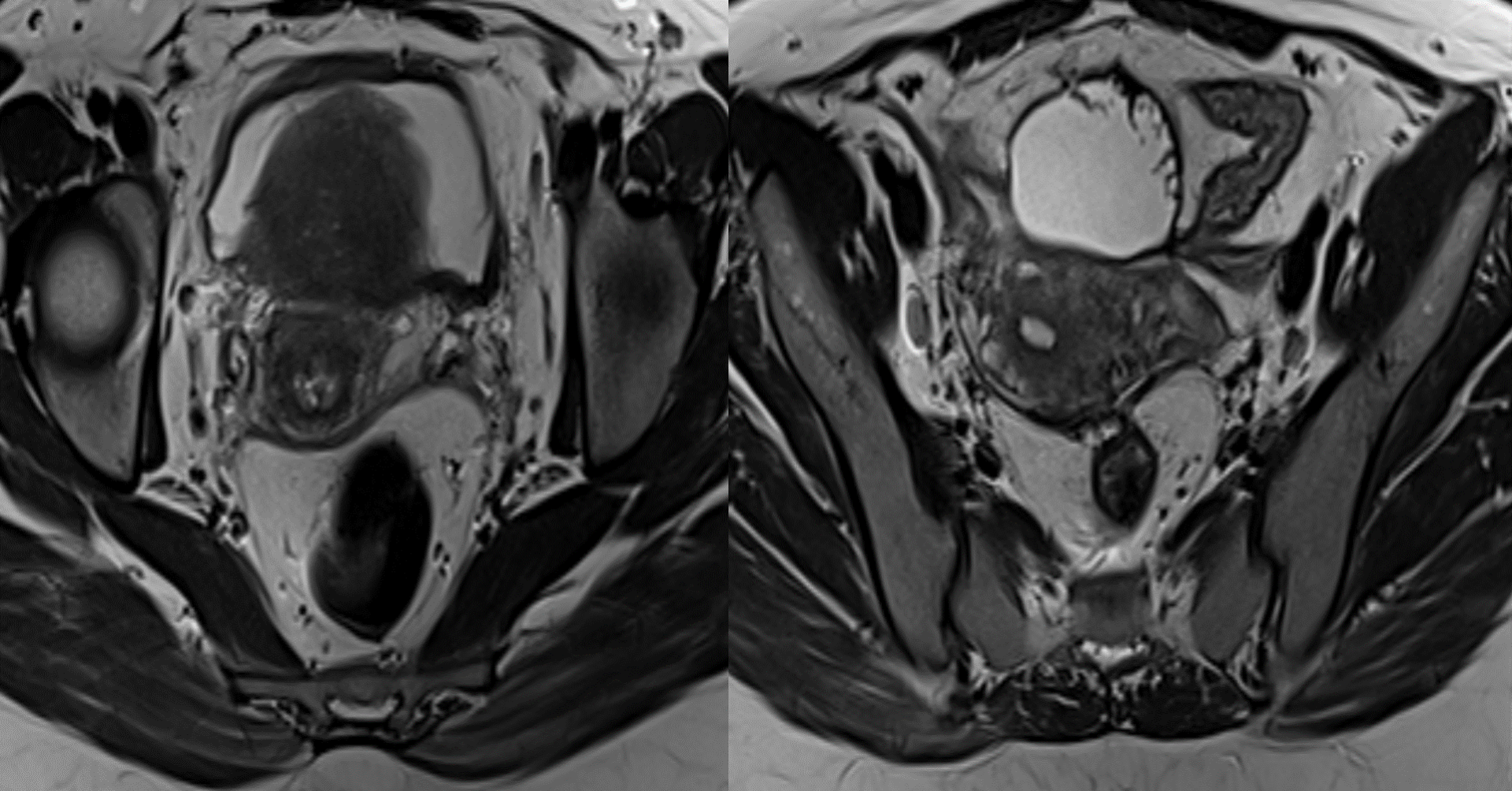
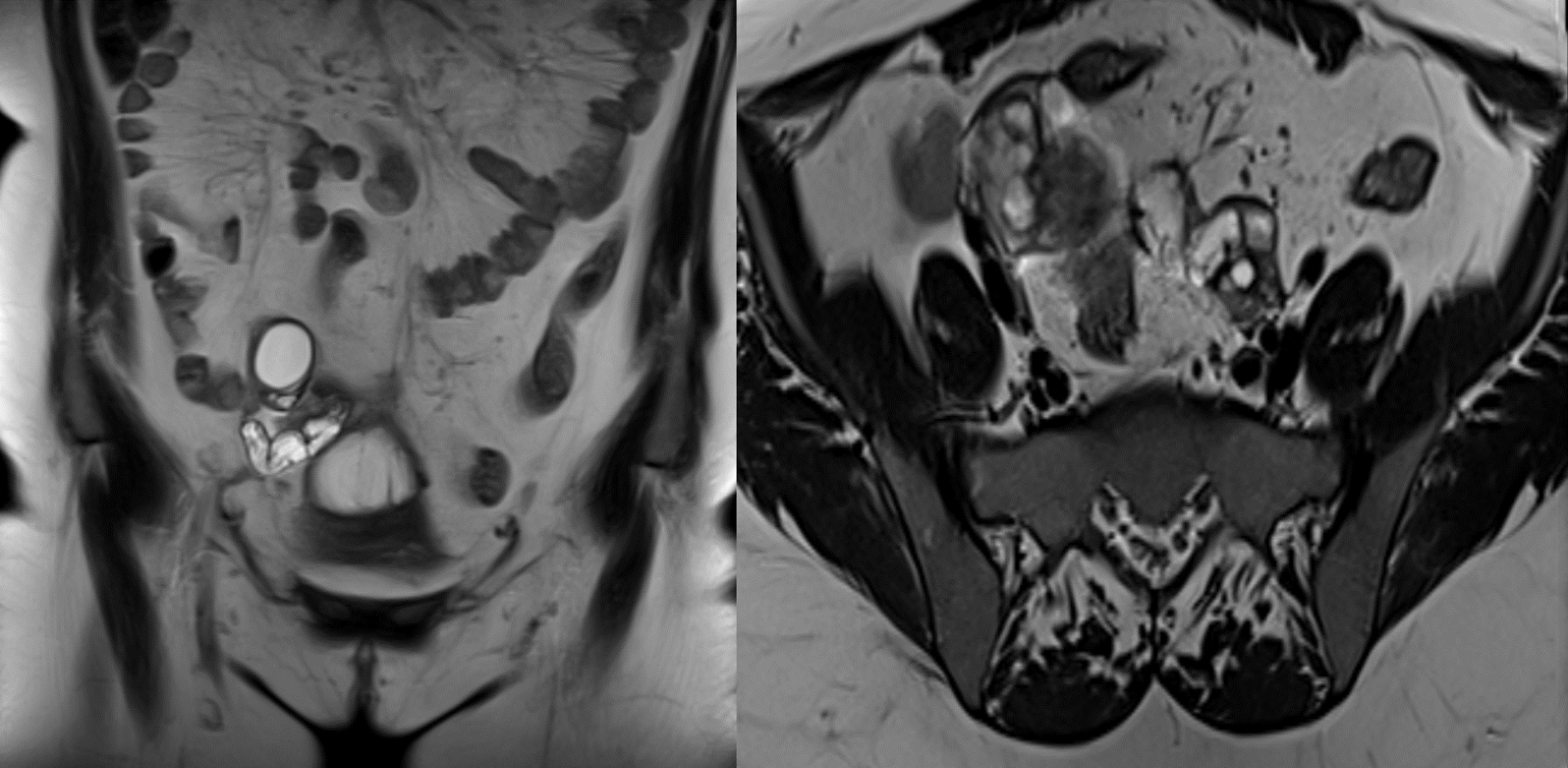
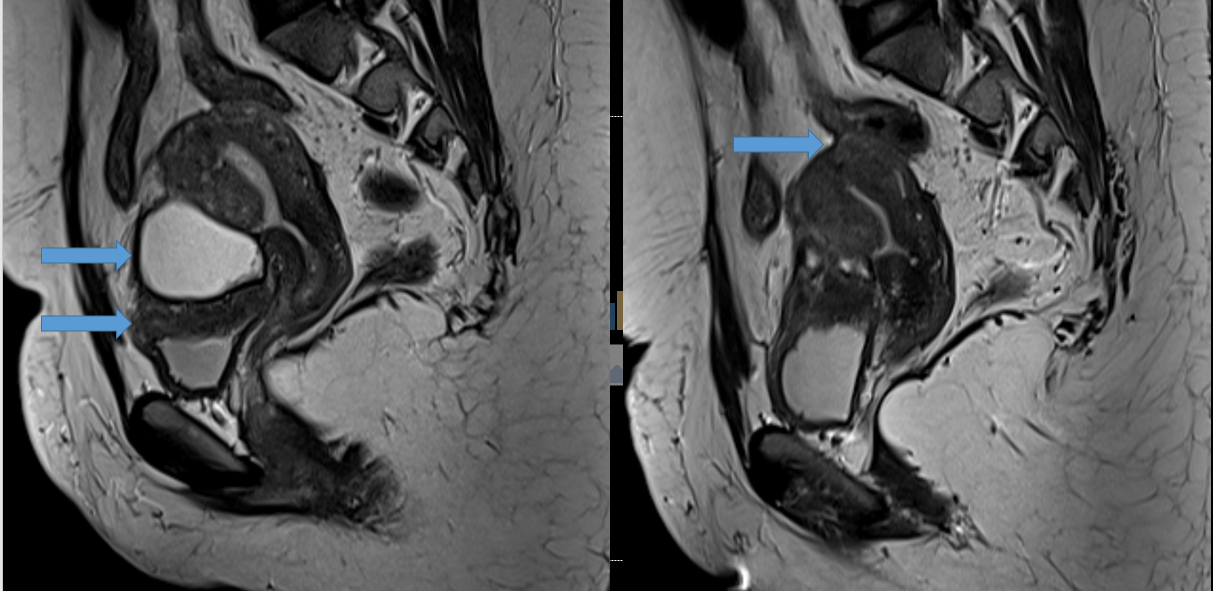
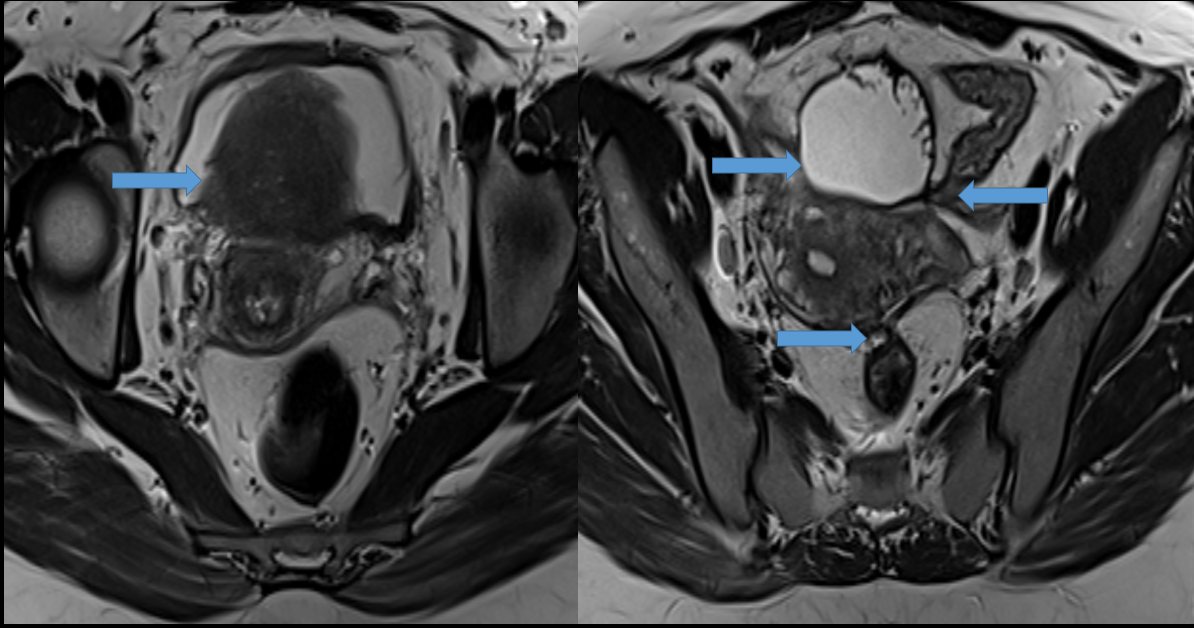
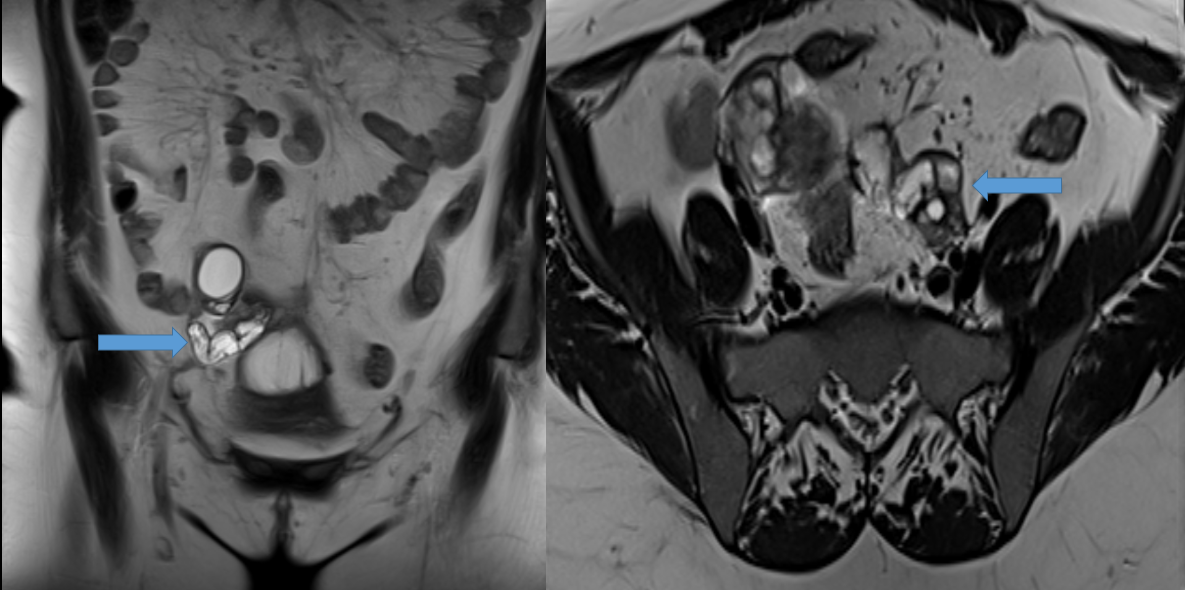
25-year-old female with dysmenorrhea
- T2 hypointense plaque-like thickening along the roof of the bladder with few internal T2 hyperintense foci.
- Similar T2 hypointense plaque-like thickening is also noted along the posterior wall of the torus uterus.
- Multiple pelvic adhesions.
- Moderate-sized T2 hyperintense well-marginated fluid collection was seen along the fundus and anterior surface of the body of the uterus in the vesicouterine pouch.
- Bilateral mild hydrosalpinx.
DIAGNOSIS AND DISCUSSION:
Deep pelvic endometriosis with endometrial deposit over the bladder, loculated vesico-uterine collection, adhesions in pelvis and bilateral mild hydrosalpinx.
Discussion:
- Deep pelvic endometriosis, also known as deep infiltrating endometriosis involvement, is defined as sub peritoneal invasion by endometriotic lesions that exceeds 5 mm in depth. It can affect fibromuscular pelvic structures, such as the recto- vaginal septum and uterosacral ligaments (69.2% of cases), as well as the vagina (14.5%), alimentary tract (9.9%), urinary tract (6.4%), and other extraperitoneal pelvic sites.
- Although peritoneal endometriosis is often asymptomatic, deep pelvic endometriosis is frequently associated with dysmenorrhea, dyspareunia, pelvic pain, urinary tract symptoms, and infertility. Unusual findings such as pneumothorax and epistaxis may be seen when endometriotic implants occur in atypical locations outside the pelvis.
- The anatomy of the female pelvis and perineum is best understood when these regions are sub- divided according to functional and clinical requirements into anterior, middle, and posterior compartments.
Role Of MRI :
- MRI has greater specificity for the diagnosis of endometriomas than the other non-invasive imaging techniques and thus has a role to play in the evaluation of adnexal masses, as well as assessing for the response to medical therapy potentially eliminating the need for follow-up laparoscopy. Typically, the lesions that can be detected with MRI are those that contain blood products.
- Hemorrhagic “powder burn”: Lesions appear bright on T1 fat-saturated sequences
- Small solid deep lesions may be hyperintense on T1 and hypointense on T2
- Adhesions and fibrosis
- Isointense to pelvic muscle on both T1 and T2 weighted images
- Spiculated low signal intensity stranding that obscures organ interfaces
- Distortion of normal anatomy
- Posterior displacement of the uterus
- Kissing ovaries sign: seen in the severe forms of the disease
- Angulation of bowel loops
- Elevation of the posterior vaginal fornix
- Loculated fluid collections
- Hydrosalpinx
Endometriomas:
- <5 mm: early-stage disease; >15 mm: advanced disease
- Shading sign: may be less likely to respond to medical treatment 28
- low T1 and T2 due to tissue and hemosiderin-laden macrophages
Diagnostic criteria:
- Multiple cysts with T1 hyperintensity OR
- One or more cysts with high T1 and shading on T2
Uterosacral involvement :
- Normal uterosacral ligaments are smooth and of regular contour
- Irregular margins
- Asymmetry
- Nodularity and thickening medially (>9 mm) 13
- Altered T2 signal: isointense (50%), hypointense (40%) or hyperintense (10%) compared to myometrium
- If bilateral uterosacral involvement with additional involvement, torus uterinus involvement results in an arciform abnormality.
Vaginal involvement
- Loss of hypointense signal of the posterior vaginal wall on T2
- Thickening, nodules, and/or masses are also potentially seen
Pouch of Douglas
- Partial to complete obliteration
- Suspended or lateralized fluid collections
Rectovaginal septum: nodules or masses that have passed through the lower border of the posterior lip of the cervix
Urinary tract
Bladder
- Localized or diffuse bladder wall thickening
- Signal intensity abnormality
- Nodules or masses usually located at the level of the vesicouterine pouch
- Involvement of bladder mucosa is rare
Other sites: GIT, URINARY BLADDER, CHEST CUTANEOUS NODULES.
References:
- MR Imaging in Deep Pelvic Endometriosis- Antônio Coutinho et al.
https://pubs.rsna.org/doi/10.1148/rg.312105144 - Endometriosis – MRI detection – The Radiology Assistant
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr SOHAM NAIK
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.