A 52 year old male presented with complaints of pain on left side of face radiating to head Recurrent seizure (last episode 3 years ago), on medication.
Previous H/O invasive rhinocerebral fungal sinusitis (5 years ago) with post FESS and craniotomy status
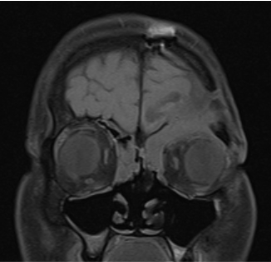
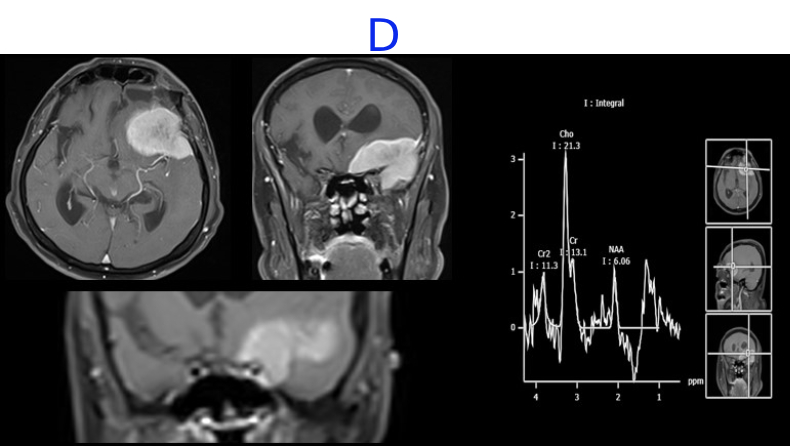
A. FINDINGS –MR BRAIN WITH IV CONTRAST
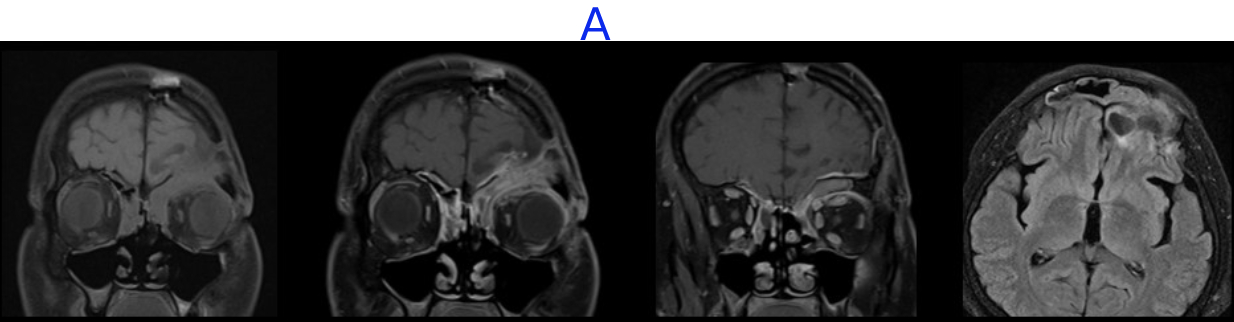
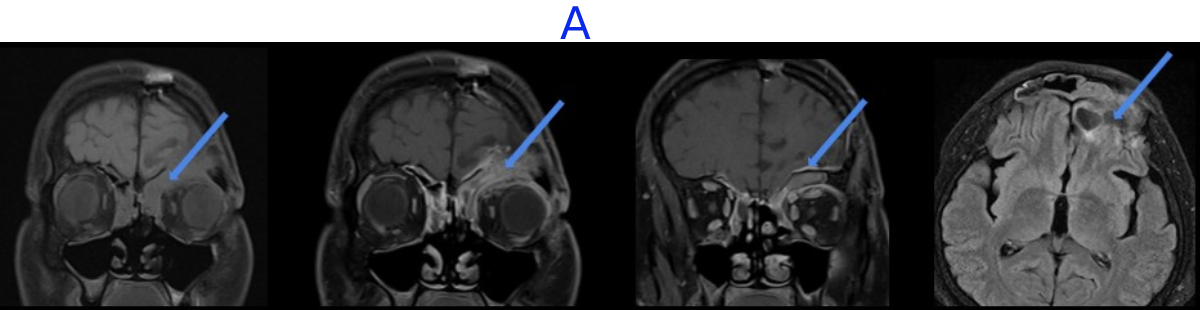
B. FINDINGS – CT PNS
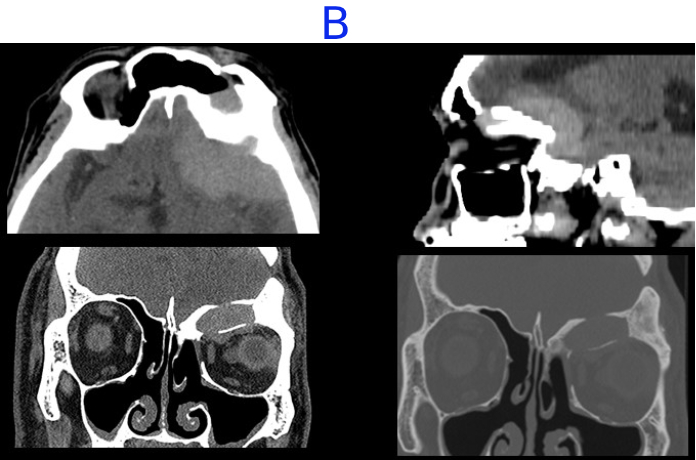
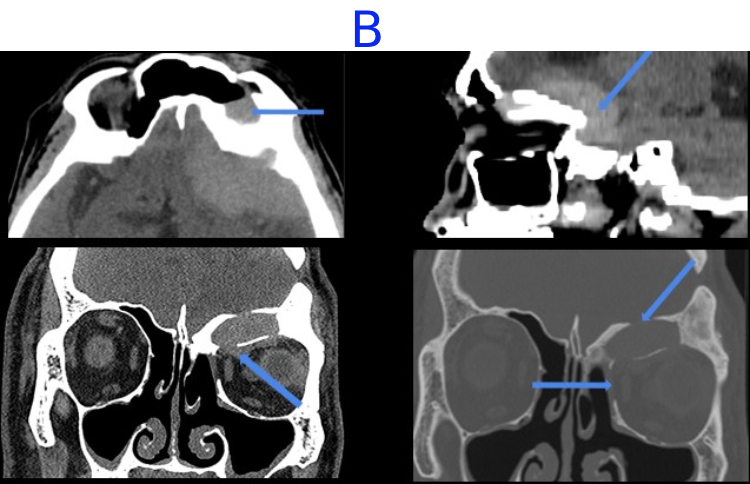
C. FINDINGS –MR BRAIN WITH IV CONTRAST
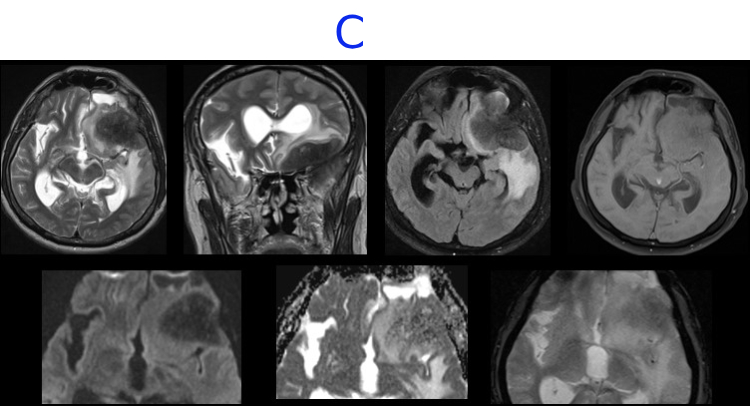
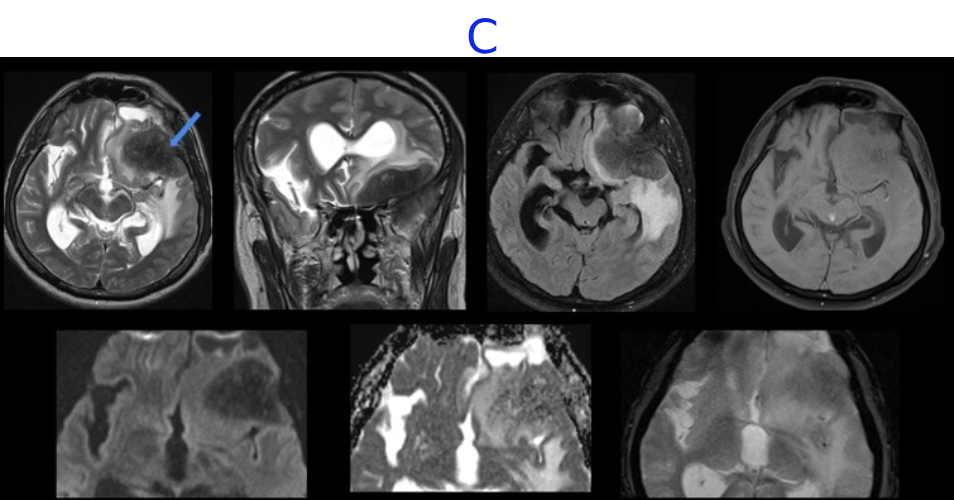
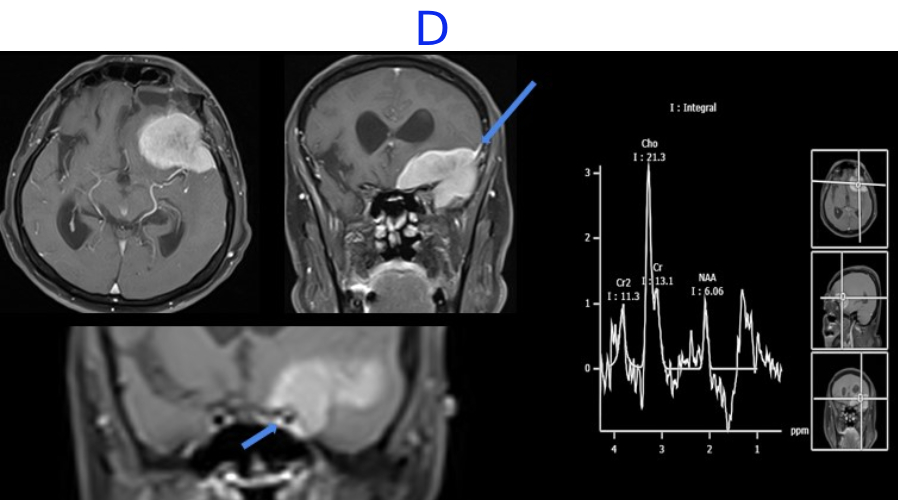
D. FINDINGS –MR BRAIN WITH IV CONTRAST, MR SPECTROSCOPY
A. LEGENDS:
- Opacification in bilateral frontal and ethmoid sinus showing enhancement on post contrast images.
- The mucosal thickening seen extending along the craniectomy defect with adjacent dural thickening.
- Cystic encephalomalacic changes seen in the anterior part of left frontal lobe.
B. LEGENDS:
- Mucosal thickening in left frontal sinus with hyperdense content, suggestive of fungal elements/ inspissated secretions.
- Hyperdense soft tissue component is seen extending into anterior and middle cranial fossa and into extraconal compartment of left orbit with mild displacement of superior oblique and superior rectus muscle.
- Bony erosion of superior and medial wall of left orbit and floor of anterior cranial fossa
C. LEGENDS:
- Well-defined T2/ FLAIR hypointense, T1 isointense extra-axial, broad based lesion in left frontal and temporal regions along lesser wing of sphenoid with surrounding vasogenic edema noted.
- No diffusion restriction.
- No blooming on GRE images.
D. LEGENDS:
- On post contrast the lesion shows homogeneous enhancement with impression of a dural tail laterally.
- Medially the lesion abuts the left cavernous sinus and encases the cavernous segment of left ICA.
- MR spectroscopy shows choline peak.
Intracranial Fungal granuloma
TREATMENT
- Endonasal clearance of PNS with left frontotemporal craniotomy and tumor excision.
- On the 3rd post operative day, the patient had one episode of seizure with altered sensorium.
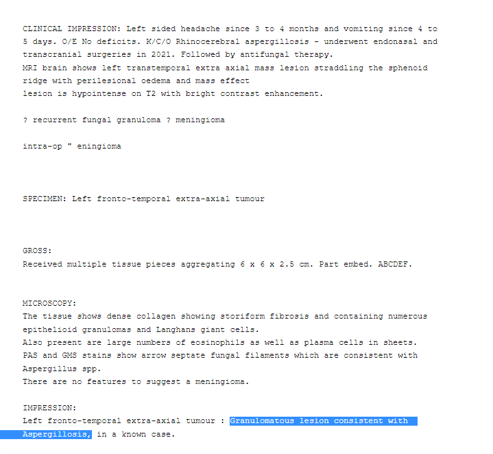
DIAGNOSIS
Angio-invasive intracranial aspergillosis with left PCA pseudoaneurysm, SAH and left SCA territory infarct
TREATMENT
Flow diverter deployment and partial coiling of left P1 PCA aneurysm
DISCUSSION:
- Fungal infections can spread by inhalation, ingestion, or direct contact such as trauma
- MC - Zygomycetes class (Rhizopus, Mucorale, and Rhizomucor species) and Aspergillus
- Risk factors - poorly controlled diabetes, haematologic malignancies, organ transplant, immunosuppressive agents, and immunosuppressive diseases
Pathophysiology
- Fungal infection makes phagocytes dysfunctional and can adhere to endothelial cells causing endothelial damage.
- They manipulate their environment while acquiring iron from the patient, which is essential for their growth and replication
- Neutrophils helps in destruction of the hyphae and the prevention of germination. In neutropenic pts, high chances of getting fungal infection.
C/F
- Facial swelling and pain, headache.
- Fever
- Nasal congestion
- Proptosis,
- Cranial nerve palsy
MC anatomic locations - Nasal cavities (middle turbinates), maxillary sinuses.
A definitive diagnosis of fungal rhinosinusitis is made on the basis of tissue biopsy.
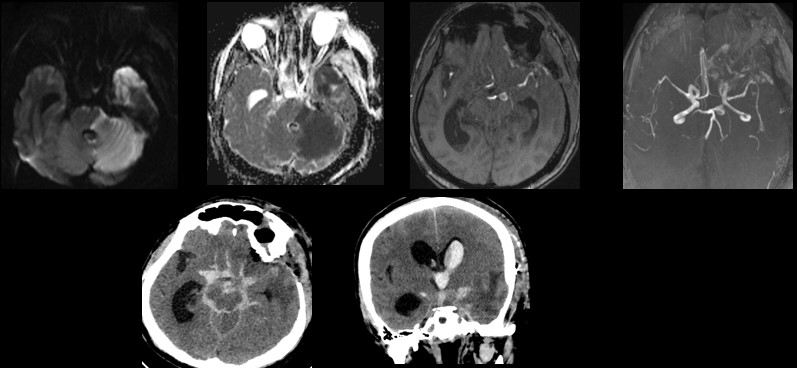
Cavernous Sinus Extension
Symptom:
- headache visual impairment, ophthalmoplegia thrombosis and narrowing of the internal carotid artery Direct findings
- Enlargement and expansion of the cavernous sinus with bulging lateral walls
- Loss of flow voids, with restricted diffusion suggests cavernous sinus thrombosis
- Bone destruction.
Indirect findings
- Narrowing of ICA flow void
- Dilatation and/or subsequent thrombosis of the superior and inferior ophthalmic veins
Large- and Small-Vessel Involvement
Symptoms - vision change, ptosis or cranial nerve palsy, headache
Imaging findings
- Because of the decreased resistance to intra-arterial pressure caused by the destruction fungal aneurysms tend to be fusiform, with a longer shape and a more proximally localized
- Tendency of fungi to invade proximal arteries leads to a larger infarction.
- Thickening and enhancement of the ICA wall with or without narrowing indicate ICA involvement
- Vascular involvement - smooth or nodular wall enhancement
- Thrombus - absence of contrast enhancement, diffusion restriction, loss of flow voids
Direct Intracranial Extension and Intracranial Dissemination
- Many fungi penetrate BBB by transcellular (transendothelial cells) migration, degradation of the tight junctions or crossing the endothelial cell layer in phagocytes
- Cerebritis, infarction, hemorrhage, meningitis, abscess, subdural empyema, thrombosis of dural sinuses, and arterial involvement.
- Perineural invasion (most commonly along trigeminal nerve)
- Involvement of the ipsilateral pterygopalatine fossa in sinusitis, without bone destruction, indicates perineural or perivascular spread along the sphenopalatine artery.
REFERENCE
Deadly fungi: Invasive fungal rhinosinusitis in the head and neck
Mariko Kurokawa, Ryo Kurokawa, Akira Baba, John Kim, Christopher Tournade, Jonathan Mchugh, Jonathan D.Trobe, Ashok Srinivasan, Jayapalli Rajiv Bapuraj, Toshio Moritani
https://doi.org/10.1148/rg.220059
Dr ANITA NAGADI
Senior Consultant Radiologist
Manipal Hospital, Yeshwanthpur, Bengaluru.
Dr SHIKHA JOSHI
Radiology resident
Manipal Hospital, Yeshwanthpur, Bengaluru.